- Research article
- Open access
- Published: 29 February 2024

The effectiveness, implementation, and experiences of peer support approaches for mental health: a systematic umbrella review
- Ruth E. Cooper 1 na1 ,
- Katherine R. K. Saunders 1 na1 ,
- Anna Greenburgh 2 ,
- Prisha Shah 6 ,
- Rebecca Appleton 2 ,
- Karen Machin 6 ,
- Tamar Jeynes 6 ,
- Phoebe Barnett 2 , 3 , 4 ,
- Sophie M. Allan 2 , 5 ,
- Jessica Griffiths 1 ,
- Ruth Stuart 1 ,
- Lizzie Mitchell 6 ,
- Beverley Chipp 6 ,
- Stephen Jeffreys 6 ,
- Brynmor Lloyd-Evans 2 ,
- Alan Simpson 1 , 7 &
- Sonia Johnson 2 , 8
BMC Medicine volume 22 , Article number: 72 ( 2024 ) Cite this article
9066 Accesses
2 Citations
26 Altmetric
Metrics details
Peer support for mental health is recommended across international policy guidance and provision. Our systematic umbrella review summarises evidence on the effectiveness, implementation, and experiences of paid peer support approaches for mental health.
We searched MEDLINE, EMBASE, PsycINFO, The Campbell Collaboration, and The Cochrane Database of Systematic Reviews (2012–2022) for reviews of paid peer support interventions for mental health. The AMSTAR2 assessed quality. Results were synthesised narratively, with implementation reported using the CFIR (Consolidated Framework for Implementation Research). The protocol was registered with PROSPERO (registration number: CRD42022362099).
We included 35 reviews (426 primary studies, n = 95–40,927 participants): systematic reviews with ( n = 13) or without ( n = 13) meta-analysis, or with qualitative synthesis ( n = 3), scoping reviews ( n = 6). Most reviews were low or critically low (97%) quality, one review was high quality. Effectiveness was investigated in 23 reviews. Results were mixed; there was some evidence from meta-analyses that peer support may improve depression symptoms (particularly perinatal depression), self-efficacy, and recovery. Factors promoting successful implementation, investigated in 9 reviews, included adequate training and supervision, a recovery-oriented workplace, strong leadership, and a supportive and trusting workplace culture with effective collaboration. Barriers included lack of time, resources and funding, and lack of recognised peer support worker (PSW) certification. Experiences of peer support were explored in 11 reviews, with 3 overarching themes: (i) what the PSW role can bring, including recovery and improved wellbeing for service users and PSWs; (ii) confusion over the PSW role, including role ambiguity and unclear boundaries; and (iii) organisational challenges and impact, including low pay, negative non-peer staff attitudes, and lack of support and training.
Conclusions
Peer support may be effective at improving some clinical outcomes, self-efficacy, and recovery. Certain populations, e.g. perinatal populations, may especially benefit from peer support. Potential strategies to successfully implement PSWs include co-production, clearly defined PSW roles, a receptive hierarchical structure and staff, appropriate PSW and staff training with clinical and/or peer supervision alongside safeguarding. Services could benefit from clear, coproduced, setting specific implementation guidelines for PSW. PSW roles tend to be poorly defined and associations between PSW intervention content and impacts need further investigation. Future research should reflect the priorities of providers/service users involved in peer support.
Peer Review reports
Peer support in mental health care is a recovery-orientated approach delivered by individuals who have lived experience of mental health difficulties (as service users, carers, parents or supporters). Peer support workers (PSWs) are employed to draw on these experiences to support mental health service users or carers of people with mental health conditions [ 1 , 2 ]. As such, PSWs are uniquely positioned to facilitate recovery through empathic engagement with service users and their support networks. The success of peer support is thought to be based in the sharing of lived experiences and mental health knowledge and through interpersonal connection [ 3 , 4 ]. Across diagnoses, peer support may promote recovery through the modelling of coping strategies, and by providing hope and an example of recovery to those dealing with mental health difficulties [ 5 ].
Peer support has been utilised across various populations and types of service, for example in services for early intervention in psychosis [ 6 ], for people with co-occurring substance abuse and mental health difficulties [ 7 ], and in community interventions to reduce mental health inpatient admissions [ 8 ]. The format of peer support varies across services, for example it may involve one-to-one or group sessions, online or face-to-face delivery, unstructured open-ended conversations or more structured manualised support, or activities such as walking groups [ 9 , 10 ]. Peer support may be delivered by trained peer support staff or on a more ad hoc basis among peers [ 11 ]. Peer support for mental health takes place within mental health services in both statutory and voluntary sector settings [ 11 ]. Although PSWs may be paid or unpaid [ 6 , 12 ], paid roles have become increasingly available in mental health care settings [ 13 ]. Professionalising PSW roles as paid demonstrates the value of the role and appropriately rewards work done, should ensure formal training, supervision and management, and may help to clarify the boundaries of the role [ 14 ].
Service user networks and researchers in relevant fields have strongly advocated for provision of peer support [ 14 , 15 ], and peer support is now recognised and recommended across international mental health policy guidance, reflecting an increased understanding of the value of embedding lived experience support in formal mental health services [ 16 , 17 , 18 , 19 , 20 ]. In the UK, peer support is currently being expanded in the NHS [ 16 ].
There have been many reviews of the peer support literature separately evaluating the efficacy, implementation, and experiences of peer support from a variety of different perspectives (e.g. [ 21 , 22 , 23 , 24 ]). Given the numerous and sometimes inconclusive results from existing reviews on this topic, our research group, the NIHR Mental Health Policy Research Unit, agreed with policy makers in England to conduct an umbrella review of peer support to provide clinicians, policy makers and researchers with an overall assessment on the evidence available, comparing results between reviews, while taking the quality of these reviews into account [ 25 , 26 ]. The aim of this systematic umbrella review is to collate, synthesise and summarise the available evidence from published reviews to address the following research questions:
What is the effectiveness (e.g. clinical, social, functional) and cost-effectiveness of paid peer support approaches for mental health?
What influences the implementation of peer support approaches for mental health?
What are the experiences of peer support approaches for mental health (e.g. of acceptability) from the perspective of PSWs, healthcare practitioners, service users, carers?
This umbrella review was conducted by the NIHR Mental Health Policy Research Unit (MHPRU), based at King’s College London and University College London, which delivers evidence to inform government and NHS policy in England, agreeing a programme of rapid research with policymakers.
Study design and protocol
We conducted a systematic umbrella review following guidance from Fusar-Poli et al. [ 27 ] and Cochrane [ 28 ]. The review is reported according to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) (see Additional file 1 : Appendix 1 for the PRISMA checklist) [ 29 ]. The protocol was registered with PROSPERO (registration number: CRD42022362099) [ 30 ]. One amendment was made to the protocol after registration. We amended the ‘intervention’ section to state that reviews were excluded if the majority of interventions did not meet eligibility criteria, e.g. because we found that reviews often included paid and unpaid peer support interventions and did not report results separately.
Lived experience researcher involvement
Members of the MHPRU Lived Experience Working Group (LEWG), who collectively have substantial experience of delivering or receiving peer support, contributed extensively to this review, including protocol development, study selection, data extraction, quality appraisal, data synthesis, drafting the manuscript and lived experience commentary, and attending working group meetings.
Eligibility criteria
The eligibility criteria are detailed in full in the protocol [ 30 ]. In summary, we included:
Study designs : Published, peer-reviewed systematic, scoping or realist reviews which synthesised quantitative or qualitative data (narratively or formally using, e.g. a meta-analysis or meta-synthesis) that examined outcomes or experiences relevant to our research questions.
Intervention : We defined peer support as ‘involving a person who has lived experience of mental health condition(s), or caring for those with mental health conditions, being employed to use and draw on their experiences and empathy to support service users who have mental health conditions or carers or parents of people with mental health conditions.’ Eligible peer support approaches were paid, meaning that the PSW was paid for their work, and delivered face-to-face or remotely, for people with mental health conditions or for carers of people with mental health conditions, across any mental healthcare settings. Peer support approaches were ineligible if the PSWs were not in a dedicated peer support role, if they were primarily for physical health, or automated (i.e. peer support ‘bots’ or avatars). We excluded reviews where over 50% of primary studies in the review did not meet eligibility criteria, e.g. if the majority of people delivering the interventions were unpaid.
Population : Children, young people and adults with a mental health condition (including substance use disorders), carers, paid PSWs and mental healthcare practitioners working alongside PSWs. We excluded service users with a primary diagnosis of an organic mental disorder (e.g. dementia), neurodevelopmental disorders, acquired cognitive impairment and adjustment disorders.
Outcome measures : Included reviews reported outcomes or data on at least one of the following peer support related outcomes that addressed our research questions: (i) clinical outcomes, (ii) economic or cost-effectiveness, (iii) recovery outcomes, e.g. hope, empowerment, goal-attainment, quality of life, (iv) social outcomes, (v) implementation outcomes and barriers and facilitators to implementation, (vi) experiences of delivering, receiving or working alongside peer support and (vii) theories of what works for whom in peer support.
Information sources and search strategy
We combined terms for peer support, reviews and mental health conditions using Boolean operators (AND, OR). We searched the following databases: MEDLINE, EMBASE, PsycINFO, The Campbell Collaboration and The Cochrane Database of Systematic Reviews (see Additional file 1 : Appendix 2 for full search strategy). Searches were run from January 2012 to November 2022 as these reviews will include primary research published before 2012 [ 31 ]. There was no time limit for the primary papers in the included reviews. We had no language restrictions.
Selection process
Reviewers (KS, RC, JG, RS, RA, KM, PS, SA) screened titles and abstracts, and subsequently full texts. To ensure consistent application of eligibility criteria all reviewers initially independently screened the same ten titles and abstracts and discussed inclusion/exclusion. The remaining titles and abstracts were then screened. Records were double screened blind by two reviewers at both the title and abstract (94% agreement) and full text (86% agreement) stages. All disagreements were resolved through discussion with the study team.
Data extraction
Data extraction was completed in Microsoft Excel by the review team (RC, KS, KM, PS, JG, RS, PB, RA). The data used in the paper were checked by another member of the review team. The extracted data included basic information about reviews (e.g. number of included studies, number of participants, review type, aim/objectives), basic information about primary studies (e.g. references, designs), search strategy (e.g. databases searched, eligibility criteria), population (e.g. gender, age), peer support approach (e.g. peer support type and description), type of comparator, additional information (e.g. quality appraisal methods, review author conclusions), primary and secondary outcomes of systematic review or qualitative results.
Quality appraisal of included reviews
The quality of included reviews was independently assessed by reviewers (RC, KS, KM, PS, JG, RS, PB, RA) using the AMSTAR 2 (A MeaSurement Tool to Assess systematic Reviews), a 16-point tool for assessment of the methodological quality of systematic reviews [ 32 ]. We adapted the AMSTAR 2 to apply for scoping reviews and systematic reviews of qualitative data (described in full in Additional file 1 : Appendix 3). The following questions were adapted: (1) PICO criteria, (2) Protocol requirements, (8) Detail of included studies, (9) Risk of Bias requirement. Two reviewers (KS, AG) 100% double-scored reviews blind with any outstanding disagreements resolved through discussion between AG, KS, and RC. Overall ratings for each study were calculated according to guidance [ 32 ], based on 7 critical domains and 6 non-critical domains within the AMSTAR 2 tool. Studies with no or one non-critical weakness and no critical flaws were rated as high quality. Studies with more than one non-critical weakness and no critical weaknesses were rated as moderate quality. Studies with one critical flaw irrespective of non-critical weaknesses were rated as low quality, and those with more than one critical flaw irrespective of non-critical weaknesses were rated as critically low quality. The AMSTAR 2 guidance [ 32 ] states that reviews of critically low quality should not be relied on for comprehensive and accurate summaries of the literature.
Synthesis methods
Rq 1: what is the effectiveness (e.g. clinical, social, functional) and cost-effectiveness of paid peer support approaches for mental health.
Data were tabulated and summarised narratively by two researchers (KS, AG); effectiveness meta-analysis data calculated from two or more studies were tabulated separately from non-meta-analysis effectiveness outcomes. Review outcomes were similar, but not similar enough to combine meaningfully in a meta-analysis. Effect sizes (with 95% CIs and p -values) were reported along with I 2 statistic (with 95% CIs, p -values, χ 2 , and degrees of freedom) where available. We did not tabulate data for subgroup analyses.
RQ 2: What influences the implementation of peer support approaches for mental health?
Outcomes were tabulated according to the main domains in the Consolidated Framework for Implementation Research (CFIR) [ 33 ]. The CFIR provides a comprehensive framework, composed of 5 domains, associated with the effective implementation of interventions [ 33 ]. The 5 domains are as follows: Innovation (the ‘thing’ being implemented); Outer setting (the setting in which the inner setting exists, e.g. hospital system); Inner setting (the setting in which the innovation is implemented, e.g. hospital); Individuals (the roles and characteristics of individuals); Implementation process (the activities and strategies used to implement the innovation) [ 33 ]. Synthesis was conducted using a collaborative process involving one member of the study team (RA) and one lived experience researcher (PS).
RQ 3: What are the experiences of peer support approaches for mental health (e.g. of acceptability) from the perspective of PSWs, healthcare practitioners, service users and carers?
Experiences were synthesised narratively, by three researchers, including two lived experience researchers (TJ, KM, RC) [ 34 ]. Themes from reviews which were identified as addressing research question 3 were extracted and similar themes across the reviews were grouped together. Each group was accounted for using an existing theme from one or more of the reviews or if this was not possible a new theme was developed. Three overarching themes were identified through iterative scrutiny of the data and discussion between TJ, KM, and RC. A summary of the common themes across the reviews, grouped under the three overarching themes, was then developed, including highlighting contrasting findings.
Study selection
The search strategy identified 777 references to be screened (a further 2 papers were identified through other methods); 93 full text articles were assessed for eligibility with 57 excluded (see Additional file 1 : Appendix 4 for reasons for exclusion). Thirty-five reviews (reported in 36 papers) were included (see Fig. 1 ).
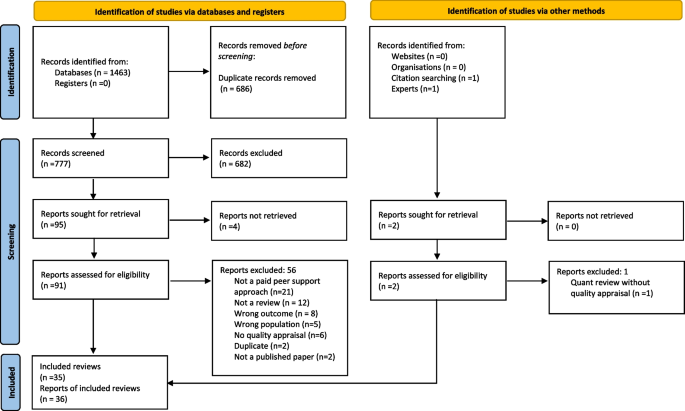
PRISMA flow diagram [ 29 ]
Characteristics of included reviews
Review characteristics are detailed in Table 1 . Of the 35 included reviews, 13 were systematic reviews with meta-analyses, 13 were systematic reviews without meta-analyses, 3 were systematic reviews with a qualitative synthesis and 6 were scoping reviews. The individual reviews included between 95 and 40,927 participants; 6 reviews did not report the number of participants. For reviews where the population were service users, almost all were categorised as adults with mental health problems. Thirteen reviews specified that participants had severe mental illness (SMI) diagnoses [ 1 , 21 , 22 , 35 , 36 , 37 , 38 , 39 , 40 , 41 , 42 , 43 , 44 , 45 ], six reviews explicitly included studies with participants accessing mental health services [ 22 , 37 , 38 , 43 , 45 ] [ 46 ], three reviews were conducted in perinatal populations [ 47 , 48 , 49 ], three reviews included participants with any/common mental health conditions [ 50 , 51 , 52 ], four reviews included participants with substance use disorders [ 1 , 38 , 53 , 54 ], two reviews included participants with eating disorders [ 55 , 56 ], one included people experiencing suicidality [ 57 ] and one included articles on peer support for crisis management [ 58 ]. The samples in the remaining reviews were PSWs and various stakeholders (e.g. non-peer staff, service users) [ 23 , 24 , 34 , 59 , 60 , 61 , 62 , 63 , 64 ]. Most reviews included interventions involving any form of peer support, individual, group or combined, although three reviews looked at group peer support alone [ 35 , 43 , 49 ], and three reviews looked at individual peer support alone [ 1 , 40 , 45 ]. Reviews looked at peer support delivered in-person, online or over the phone, and surveyed a range of approaches including both structured and unstructured peer support (see Table 1 ). The reviews included 426 primary studies. We assessed study overlap; most primary studies ( n = 300) were only included in one review; however, many primary studies were included twice ( n = 72), three times ( n = 18) to a maximum of nine times ( n = 1) (see Additional file 1 : Appendix 5 for overlapping studies). Only 1 review reported that people with lived experience were involved in the review [ 57 ]. Only 2 reviews assessed certainty of evidence (using GRADE) [ 21 , 22 ].
Most reviews were appraised as low or critically low (97%) quality and one review was appraised as high quality. The most common weaknesses were in critical domains concerning registering protocols before commencement of the review (21 studies), justification of excluding individual studies (28 studies) and considering risk of bias when interpreting results (13 studies). Reviews without meta-analyses were not scored in the critical domains assessing meta-analytical method or publication bias. There were 13 studies with meta-analyses assessed in these two domains: two of these exhibited one critical weakness and two exhibited two critical weaknesses. As scoping reviews are intended to provide overviews of existing literature regardless of risk of bias [ 65 ], scoping reviews were not scored in the critical domain concerning risk of bias assessment techniques (see Additional file 1 : Appendix 3 for adjustments to quality appraisal for scoping and qualitative reviews). Of the 29 reviews that were eligible to be scored in this domain, 10 exhibited a critical weakness. The review eliciting high confidence was a Cochrane review [ 21 ]. No reviews were rated as moderate. AMSTAR 2 ratings are detailed in Table 1 and in full in Additional file 1 : Appendix 3.
Results of synthesis
Rq1: what is the effectiveness (e.g. clinical, social, functional) and cost-effectiveness of paid peer support approaches for mental health.
Effectiveness outcomes were reported in 23 reviews (66% of total). A wide variety of clinical, recovery and psychosocial effectiveness outcomes were reported across both meta-analysis [ 21 , 22 , 37 , 40 , 41 , 42 , 43 , 44 , 45 , 47 , 48 , 51 , 52 ] and narrative results [ 1 , 21 , 22 , 35 , 36 , 37 , 38 , 40 , 41 , 42 , 43 , 44 , 48 , 50 , 51 , 53 , 54 , 56 , 57 , 58 , 60 ]. Comparator groups also varied across the primary studies included in the reviews, including Treatment as Usual (TaU), active controls (e.g. a comparable standard treatment) and waitlist control groups.
All outcomes except for one (family or carer use of formal community support services; [ 44 ]) were service user outcomes, rather than carer, staff or PSW outcomes. Outcomes from systematic reviews with meta-analysis are reported in Tables 2 , 3 and 4 . Effectiveness results from reviews not including meta-analysis are summarised at the end of this section and reported in full in Additional file 1 : Appendix 6. Evidence was heterogenous across all outcomes and reviews, with many analyses reporting no effect. In the meta-analysis results, there was often notable heterogeneity. There was limited data on cost and cost-effectiveness, but the evidence available from three systematic reviews without meta-analyses (See Additional file 1 : Appendix 6) suggested that peer support interventions were low cost and cost-saving [ 38 , 48 , 50 ].
Results from meta-analyses
Clinical outcomes.
For depression outcomes, evidence from two reviews with meta-analyses suggested that peer support is effective in improving perinatal depression [ 47 , 48 ]. Three reviews of peer support for adults and adolescents with mental health problems including those with SMI diagnoses reported no effect on depression post-intervention [ 22 , 35 , 43 ], where two of these reviews looked at group-based peer support alone [ 35 , 43 ]. Two of these reviews reported follow-up results; one review of group peer support for adults with any mental health condition continued to find no effect at 3–6 months follow-up [ 35 ], while the other involving adults with SMI reported improvements in depression and anxiety at 6 months follow-up, despite reporting no effect at post-intervention [ 22 ]. One review [ 52 ] measured clinical recovery in adults with any mental health diagnosis, reporting improvements post-intervention and at 6–9-month follow-up, but no improvement at 12–18-month follow-up.
Most evidence regarding mental health symptom severity among adults and adolescents with mental health diagnoses or who were using mental health services suggested no effect [ 22 , 35 , 41 , 42 , 43 , 44 ], other than for perinatal depression as previously summarised. One review [ 40 ] of individual peer support for adults with primarily SMI diagnoses reported improvements in symptom severity, while another involving adults with SMI [ 44 ] reported symptom improvements following family-led peer support, but no improvement following individual-led peer support. Results for service use varied depending on the measure, for example, peer support was associated with reduced risk of hospitalisation [ 44 ], including after a follow-up period [ 45 ], but no effect was found regarding length of stay [ 41 , 42 ].
All reviews providing meta-analytic evidence relevant to this question were rated low or critically low quality, except from one high-quality review [ 21 ] which found no effect of peer support on patient activation between 1 and 6 months follow-up (a person’s perceived ability to manage their illness and their approach to healthcare) in adults with schizophrenia diagnoses or similar SMI.
Recovery outcomes
Of the seven reviews with meta-analyses reporting data on overall self-reported recovery, five reported improvements in recovery in adults with mental health diagnoses including SMI [ 22 , 35 , 40 , 44 , 45 ]. Two studies found effects for individual peer support interventions alone [ 40 , 45 ], and one reported an effect for group-based peer support alone [ 35 ]. Only two reviews reported no effect [ 21 , 43 ], where one included studies of adults with SMI in both individual and group-based peer support [ 21 ], and the other involved studies with adults and adolescents with any mental health problem in group-based peer support alone [ 43 ].
Three reviews reported follow-up data showing continued improvements for adults with mental health diagnoses including SMI at follow-ups of 6 months [ 22 ], 3–6 months [ 35 ] and 12–18 months [ 45 ], the former and the latter reviewing individual and group peer support, and the second focussing on group peer support alone. One further review reported no improvements at medium-term follow-up (1–6 months) [ 21 ]. One review of adults with any mental health diagnosis identified improvements in personal recovery post-intervention, but not at 6–9 or 12–18 months follow-up, and found no improvements in functional recovery post-intervention or at 12–18 months follow-up, but did report improvements at 6–9 months follow-up [ 52 ].
All reviews providing meta-analytic evidence for these outcomes were rated as critically low or low quality, except for one [ 21 ] which was rated high quality. Based on evidence from three studies, this latter review [ 21 ] found no effect of peer support on recovery in the medium term for adults with schizophrenia diagnoses or similar SMI.
Psychosocial outcomes
Evidence regarding hope or hopefulness was mixed. Four reviews with meta-analyses suggested that peer support resulted in improvements in adults with SMI [ 22 , 37 , 40 , 44 ], where one of these studies looked at individual peer support alone [ 40 ] and the rest included both individual and group peer support. However, three reviews of studies including SMI and mixed mental health diagnoses samples reported no effect [ 21 , 35 , 43 ], where two of these reviews focussed on group-based peer support alone [ 35 , 43 ]. One study [ 22 ] followed up adults with SMI and those using secondary MH services at 3–6 months and found continued improvements in hope. However, another review investigating longer-term outcomes (over 6 months) in adults with SMI found no effect [ 21 ].
Improvements in empowerment were evidenced by two reviews with meta-analyses [ 40 , 51 ] of studies involving adults with any mental health diagnosis including SMI. No effects were reported in four reviews [ 22 , 35 , 43 , 44 ]. One of the meta-analyses finding positive effects of peer support on empowerment looked at individual peer support alone [ 40 ], whereas two of the meta-analyses with no effect solely involved group-based peer support [ 35 , 43 ]. Three studies reported follow-up data. Two showed improvements at 6 months in adults with SMI [ 22 ] and at 6–12 months follow-up among adults using mental health services with any diagnoses [ 45 ]. The other showed no improvements from group-based peer support only in adults with mental health diagnoses including SMI between 3 weeks and 6 months follow-up [ 35 ].
Quality of life reportedly improved in two reviews with meta-analyses [ 37 , 44 ] of studies involving adults with SMI, while there was no evidence of improvement in one other with an SMI sample [ 22 ]. The two studies which reported follow-up data continued to find no effect [ 22 , 45 ].
There were improvements in self-efficacy in adults with any mental health problem in all three reviews with meta-analyses reporting this outcome [ 43 , 44 , 51 ]. Decreases in self-stigma and stigma-related stress in adults and adolescents with any mental health problem were found by one review with meta-analysis of group-based peer support [ 43 ]. There was no evidence for peer support improving satisfaction with care [ 22 , 41 , 42 , 44 , 45 ] or relational outcomes (including social support and network) and building relationships (both personally and with staff) [ 41 , 42 , 44 , 45 ].
All reviews providing meta-analytic evidence for these outcomes were rated as critically low or low quality, except one high-quality review [ 21 ] which found no effect of peer support on hope in adults with schizophrenia diagnoses or similar SMI in the medium or long term.
Summary of results from systematic reviews without meta-analysis
Effectiveness results from systematic reviews without meta-analyses are tabulated in full in Additional file 1 : Appendix 6. These reviews presented mixed results pertaining to clinical outcomes including depression, anxiety, eating disorder pathology, and psychosis. However, two scoping reviews reported evidence of peer support in improving suicidal ideation [ 57 , 58 ]. Evidence was deemed inconclusive regarding the impact of peer support on indicators of service use, where three reviews failed to find evidence for peer support [ 21 , 22 , 41 , 42 ], three reported mixed results [ 1 , 38 , 54 ], and one found evidence for improvements associated with peer support [ 36 ]. More consistent evidence was found indicating peer support improves recovery outcomes [ 1 , 36 , 38 , 40 , 44 , 53 ]. For most psychosocial outcomes, systematic reviews presented mixed evidence, for example different effects were found by one high-quality review for empowerment, hope and self-efficacy, depending on what measures were used [ 21 ]. Despite mixed effects being reported overall for the impact of peer support on satisfaction with care, one review cited some possible associated moderating factors such as the number of conversations had between peer supporter and recipient [ 48 ]. Evidence was marginally less mixed for relational outcomes, such as strength of interpersonal relationships and sense of community, as the majority (three) of relevant reviews found evidence in support of peer support [ 21 , 38 , 58 ], although one review found this did not persist long term [ 21 ].
Implementation was investigated in nine reviews [ 23 , 24 , 36 , 39 , 46 , 50 , 55 , 59 , 62 ]. Table 5 shows an overview of implementation outcomes by CFIR domain [ 33 ]. All reviews relevant to this research question were rated as critically low quality based on the adapted AMSTAR 2 rating scale (see Additional file 1 : Appendix 3).
Studies reported generally high acceptability and feasibility of PSW-led interventions [ 36 , 39 , 46 , 50 ]. When planning a peer-led service, co-producing the design of peer support provision with the community and stakeholders was found to be key [ 59 ].
Outer setting
The existence of national policy and funding provisions for employing and retaining PSWs facilitated PSW-led care [ 39 , 46 , 59 ], as did integration of interventions within existing healthcare systems [ 50 ]. However, barriers included power hierarchies [ 39 ], difficulties incorporating PSWs in medical mental health care models [ 24 , 39 , 46 ], interference of work with welfare benefits [ 62 ] and a lack of recognised PSW certification [ 62 ].
Inner setting
A workplace culture emphasising recovery-orientated practice [ 24 , 59 ], and organisational openness and readiness to employ PSWs [ 39 ], was important. Facilitators included strong leadership and support at the highest level [ 46 ], and flexible and understanding employers, especially in times of crisis [ 59 ]. A key facilitator was a supportive, accepting and trusting workplace culture where PSWs occupy a central position and fit in well with other staff members [ 24 ]. A trusting culture allowed the management of risk in a psychologically safe space [ 59 ]; effective communication and collaboration between PSWs and other workers facilitated this [ 24 ], while stigmatising staff attitudes were a barrier [ 62 ]. It was easier to implement PSWs in a more collaborative and less hierarchical service [ 59 ]. There were practical facilitators and barriers for PSWs also, such as access to desk space or administrative data [ 24 , 46 ], time restraints, high caseloads [ 23 , 24 ] and insufficient funding for PSW role [ 24 , 50 ].
Individuals
The professionalisation and legitimisation of the PSW role was seen as important, with associated performance standards and/or a code of ethics [ 24 ] which was linked to rigorous recruitment practices, ensuring parity in the recruitment of PSWs and other staff [ 46 ]. A further facilitator was high levels of competency among peer-counsellors when delivering interventions and having relevant skills and knowledge, e.g. mental health conditions [ 50 ]. PSWs were often required to have recovered from their mental health difficulties [ 55 ] and be able to use their coping skills and resilience to avoid potential negative impacts on their wellbeing [ 24 ]. PSWs reported a conflicted sense of identity between being a ‘peer’ with experience of mental health problems and a ‘professional’ as a barrier to their work [ 62 ]. The use of champions and implementation leaders to drive the set up and maintenance of PSW interventions was reported as a facilitator [ 46 ], as was staff willingness and ability to work with PSWs and accept them as part of the service [ 24 ].
Implementation process
Studies emphasised the importance of comprehensive training for PSWs delivered both prior to starting work and on an ongoing basis, alongside regular clinical supervision [ 24 , 46 , 50 , 55 ] supporting the management of any problems encountered [ 59 ]. PSW roles should be clearly defined [ 24 , 62 ] and training should also be delivered to other members of staff to help them work effectively with PSWs [ 46 ]. Establishing sustainable models of cost and supervision from the outset was key for the longevity of PSW [ 50 ].
Experiences of both the benefits and challenges of peer support were reported in 11 reviews [ 23 , 34 , 39 , 42 , 46 , 49 , 55 , 60 , 61 , 63 , 64 ] from a range of perspectives: PSWs [ 23 , 34 , 39 , 55 , 61 ], service users [ 39 , 55 , 61 ], non-peer staff [ 61 ], peer support group members [ 49 ], and mixed samples which consisted of combinations of PSWs, service users, non-peer staff, carers, mental health organisations, policy makers and peer programme developers [ 23 , 39 , 42 , 46 , 55 , 60 , 61 , 63 , 64 ]. In one review, it was unclear whose perspective was being presented [ 46 ], although this review only contributed to one theme. All reviews providing evidence for this research question were rated as critically low quality based on the adapted AMSTAR 2 rating scale (see Additional file 1 : Appendix 3). We identified 3 overarching themes: (i) what the PSW role can bring, (ii) confusion over the PSW role and (iii) organisational challenges and impact. Table 6 gives an overview of the overarching themes and subthemes (with more detail in Additional file 1 : Appendix 7). The following provides an overview of each overarching theme from the perspective of the different samples (i.e. PSWs, service users, mixed samples).
What the PSW role can bring
Perspective of psws.
PSWs experienced improved wellness and recovery from working in the role, reporting increased self-esteem, personal growth, and social networks [ 23 , 34 , 55 , 61 ]. They benefited in a variety of ways, e.g. the role provided a route back into employment, improving functioning and social inclusion, and allowed them to learn more about their own mental health [ 23 , 34 ]. PSWs also reported increased self-acceptance as they no longer had to hide their mental health issues [ 34 ]. The role was therefore often reported to be mutually beneficial for PSWs and service users [ 34 , 55 ]. PSWs felt it was important that they were role models for service users, being ‘the evidence of recovery’ [ 34 ]. However, working as a PSW could also have a negative impact on the PSWs’ wellbeing and recovery [ 23 , 34 ]. Reasons for this included the role reminding them of their mental health condition and the ‘sick’ label staying with them [ 23 ].
Perspective of service users
For service users, PSWs could be role models, giving them hope of recovery [ 39 , 55 , 61 ]. PSW support normalised and de-medicalised service user experiences [ 55 ]. Lack of judgement from PSWs reduced feelings of self-stigma for service users [ 55 ]. Service users felt empowered by and valued gaining experiential knowledge from PSWs, perceiving them to be more insightful than non-peer staff, and trusting their services [ 39 ]. Service users also built rapport more easily with PSWs than non-peer staff, feeling they were more approachable and had greater empathy than non-peer staff [ 39 , 61 ]. However, some service users reported that PSWs are not role models and found it challenging to view them as professionals or fully trust their knowledge, due to their lack of training and concerns about their mental health history [ 39 , 61 ].
Perspective of non-peer staff
From working with PSWs, non-peer staff developed increased empathy towards service users and a belief in recovery [ 61 ].
Perspective of peer support group members
Forming relationships in peer support groups and having their experiences validated by others was valuable for recovery [ 49 ]. However, group members could feel isolated when other members’ experiences contrasted with their own [ 49 ].
Perspective of mixed samples
PSWs were perceived to be role models, providing valuable support to service users and giving them hope of recovery [ 60 , 64 ]. Working as a PSW could enable service users to find a role in the community, beyond the identity of being a ‘patient’ [ 61 ]. PSWs could build trust-based pathways to function as a bridge between service users and non-peer staff [ 64 ]. Within teams, working with PSWs could improve recovery-oriented care and PSWs carried out various roles, such as providing psychosocial support, advocating for service users, providing insights based on their lived experiences [ 64 ]. For mental health organisations, PSW roles decreased stigma towards mental health problems and set a positive example [ 61 ]. However, there were fears that the PSWs’ mental health condition could impact the provided support, such as increased PSW absenteeism which could increase non-peer staff caseloads and concerns that service users’ and PSWs’ could experience distress due to exposure to difficult (‘triggering’) content [ 42 , 55 , 60 ]. PSWs experienced pressure due to the perception that they were pioneers, leading to expectations, e.g. failure could reduce future PSW opportunities [ 64 ]. There was also concern that PSWs lacked mental health knowledge, beyond their own experience [ 64 ].
Confusion over the PSW role
A lack of clarity about the PSW job description led PSWs to feel the role was undervalued and tokenistic and meant they felt confused in their role. This impacted their perception of competence which affected their recovery and led to uncertainty in their responsibilities with service users [ 23 , 34 ]. PSWs also found the transition from service user to PSW and knowing where to draw the line between friend and service provider to be challenging [ 23 , 61 ]. Linked to this, their dual identity as a service user and provider could be a source of stress. For example, it meant they could closely connect with service users who had similar difficulties to their own, but this could also be triggering and lead to a recurrence of the PSWs’ own mental health issues [ 34 ]. PSWs expressed varying views on disclosing their recovery story [ 34 , 39 ]. For some, sharing elements of their story was linked to their own personal recovery [ 34 ]. However, other PSWs felt fearful of disclosure, e.g. they were concerned about being labelled ‘mentally ill’ and service users not trusting them [ 39 ].
A lack of clarity on the PSW role could lead service users to view the role as informal, leading to negative perceptions of the PSW services. Perceptions of tokenism of peer support could lead to the content of the PSW intervention ‘feeling irrelevant’ [ 39 ].
PSWs and non-peer staff found the PSW role to be ambiguous, e.g. the role was not clearly defined [ 63 ] and job descriptions were ‘vague’ [ 64 ]. Although this gave flexibility to define the role [ 64 ], it also led to challenges. Some PSWs felt they were expected to develop the role over time and received insufficient training, which hampered service delivery and could result in perceptions that PSWs were tokenistic [ 42 , 63 , 64 ]. Uncertainty about the role also led to a lack of support from non-peer staff [ 63 ]. Relatedly, there was confusion for PSWs over when/with whom to disclose their lived experience [ 63 , 64 ]. Some PSWs felt vulnerable and were reluctant to disclose, but disclosure could build trust with service users, enabled PSWs to be recovery role models, and could educate non-peer staff on alternative views [ 63 , 64 ]. Disclosure was also felt to require discretion when fitting with professional relationships. However, ‘professionalisation’ of PSWs may not challenge the existing boundaries (e.g. traditional hospital-based boundaries which could make it difficult for the sharing of lived experience to be valuable), when challenging these boundaries could change culture [ 63 , 64 ]. The transition for PSWs from patient to staff was challenging, e.g. non-peer staff were concerned about the PSW becoming unwell, making PSWs feel like they are being treated like patients [ 63 , 64 ]. There were issues around boundaries, including whether PSWs should relate to service users as friends or service users [ 63 ].
Organisational challenges and impact
PSWs experienced a lack of support and training for their role, potentially related to unclear job descriptions, and insufficient supervision [ 23 , 34 ]. This meant that PSWs struggled to develop the skills for their roles, including to work with service users with more complex needs than their own experiences [ 23 ]. Although there were some contrasting views, PSWs were concerned that they received low pay which made them feel that they were not valued, and they perceived themselves to be ‘cheap labour’ [ 23 , 34 , 61 ]. Some PSWs felt accepted in their teams however others experienced negative and rejecting non-peer staff attitudes [ 23 , 34 , 61 ]. For example, PSWs reported not being invited to social events and being treated like patients [ 61 ]. Consequently, some PSWs felt excluded, that their roles were tokenistic and experienced self-stigma [ 23 , 34 ]. PSWs as part of the newer recovery model reported challenges around integrating into traditional treatment models, e.g. where doctors spent the least time with service users but held the majority of power and decision making for service users. PSWs were expected to contest the traditional treatment model in support of a recovery focus, e.g. by their presence or in some cases being openly challenging, and this clash between old and new treatment models could lead to friction [ 23 ].
There was a fear that ‘cheap labour’ provided by PSWs may lead to fewer non-peer staff positions [ 61 ].
PSWs often received low pay, which led to role dissatisfaction for PSWs, suggesting the job was tokenistic or the role was unclear [ 63 , 64 ]. One reason for low pay was due to PSWs not requiring certification (i.e. specific qualifications, which e.g. a social worker would require) [ 63 ]. Some PSWs were positive about certification but others felt it could conflict with the grassroots ethos of peer support. However, there was the view that lived experience was not solely sufficient to work in interprofessional teams [ 64 ]. Despite this, supervision and support were often not offered to PSWs leading to risks [ 60 , 64 ].
There were challenges in PSW relationships with non-peer staff which could lead to a lack of support and hostility from non-peer staff. Non-peer staff felt threatened that they may be replaced by PSWs [ 64 ], were uneasy about working with people they previously treated [ 46 ], were concerned about the effectiveness of peer support [ 39 ], and felt expectations to support PSWs, increasing their workload [ 42 ]. This undermined the role of PSWs, e.g. they were subsequently given fewer responsibilities [ 39 ]. For PSWs, they wanted to challenge stigma by taking on more responsibility but high, varying workloads could jeopardise relationships with non-peer staff and team hierarchies hindered their ability to challenge clinically dominant ways of thinking [ 64 ].
A final theme was the perception that service users should be able to choose among PSWs as service providers [ 60 ].
Summary of key findings
An overview and summary of the key findings for each research question is presented in Table 7 .
Key findings
Our umbrella review of 35 reviews explored the effectiveness, implementation and experiences of peer support for mental health.
Effectiveness was reported in 23 reviews. Many reviews reporting effectiveness data reported no effect of peer support on a range of outcomes, mirroring the findings from other reviews [ 9 , 66 ] including those focusing on other types of peer support (e.g. online peer support for young people) [ 67 ]. However, there was consistent evidence from meta-analyses that peer support may improve the clinical outcomes of perinatal depression and risk of hospitalisation of adults with severe mental illness, as well as recovery outcomes, and self-efficacy and stigma-related outcomes. Mixed meta-analytic results were found for the clinical outcomes of overall psychiatric symptoms in adults with SMI, psychosis symptoms, length of hospital stay and patient activation, and for psychosocial outcomes such as hope, empowerment, and quality of life. There was no meta-analytic evidence for improvements in relational support. Evidence from systematic reviews without meta-analysis similarly gave a mixed picture regarding psychosocial and clinical outcomes, but indicated more consistent evidence that peer support has a positive impact on recovery, suicidal ideation, and, to some degree, satisfaction with care.
Many possible sources of heterogeneity across the included reviews could contribute to the mixed findings in this study, such as low-quality methodologies, differences in the populations included, and poor specification of peer support roles or the content of interventions delivered. One important potential contributor to our mixed results is that the primary studies contributing to the included reviews often varied in the type of control groups they considered, for example studies with treatment as usual, active controls and waitlist controls were often reviewed within the same paper. As such, it was not possible to determine whether peer support is effective in comparison to certain types of care provision but not others. In a similar vein, we could not perform subgroup analysis to determine whether specific forms of peer support are more effective on certain populations as most reviews with meta-analyses involved a combination of different formats and a range of participant groups. Nevertheless, there was some indication that differences in the format of peer support may impact its effectiveness on empowerment, as the two meta-analyses involving individual peer support alone found a positive effect on empowerment, but the two looking at group-based peer support alone did not. However, further research is needed to adequately address such questions.
Although this overview of quantitative evidence does not give unequivocal support for peer support on a variety of outcomes, the mixed results must be understood not only in the context of heterogeneity of the quantitative research conducted thus far, but with regard to the qualitative evidence documenting strong support for this intervention (as discussed in more detail below). Given that the implementation of peer support in mental health services is still relatively rare and highly variable, many of the trials conducted thus far may have tested peer support in environments where it is not fully embedded in the organisation and culture. Indeed, peer support may have positive impacts on the operation of mental health services that have not been measured as quantitative outcomes in existing trials—such as a stronger culture of person-centred care. More consistent quantitative results demonstrating the benefit of peer support may increasingly emerge as it becomes better integrated in the mental health care system.
We identified several factors reported to be important for the successful implementation of peer support, which were summarised and structured using the CFIR. These factors included adequate training and supervision for PSWs, a recovery-oriented workplace structure, strong leadership and a supportive and trusting workplace culture with effective collaboration between PSWs and non-peer staff. Barriers to peer support being implemented effectively included a lack of time, resources, and appropriate funding, and a lack of recognised PSW certification. Policy, research and campaign groups have advocated implementation approaches in line with these findings, for example, ImROC (implementing Recovery through Organisational Change) [ 14 , 68 ], who support peer support implementation globally and international competence frameworks from New Zealand [ 69 , 70 ], outline recovery focus as a core principle of peer support and emphasise the importance of training and ongoing professional development; peer support practice guidelines in the USA outline the importance of and give guidelines for supervision [ 71 ]. Formalised career pathways for PSWs [ 72 ] may help to address some of the identified barriers to effective implementation of peer support work, although these are still early in their development [ 68 ].
Experiences of peer support were from a range of perspectives (e.g. PSWs, service users, non-peer staff) and were organised under three main themes. The benefits of peer support for PSWs, service users and non-peer staff were expressed in many reviews; however, there were also conflicting and challenging experiences of the role. The mental health experience of PSWs was viewed as valuable, but also subject to some stigmatising views. For PSWs, the role could improve their personal wellness and recovery, providing a route back into employment and improving functioning, and provide service users with role models of recovery. The reciprocal benefits of peer support have also been highlighted as an advantage of peer support in resources developed by NHS England [ 19 ]. However, PSWs reported the ‘sick’ label stayed with them in the role, with non-peer staff at times concerned that PSWs mental health would impact their work, and some service users reported that they found it challenging to trust PSWs knowledge due to their lack of training and mental health history. A key experience, which became the core of our second theme, was the ambiguity of the PSW job description, including lack of clarity over boundaries with service users and when to disclose PSWs’ personal experiences. This ambiguity meant that the role was flexible, but also led to the perception that it was tokenistic and left PSWs feeling confused which impacted their own recovery. IMROC recommend the prioritisation of clear roles when implementing peer support [ 68 ]. Professional accreditation can counter the view of peer support as tokenistic, e.g. the UK Peer Support Competence Framework outlined by the Royal College of Psychiatrists [ 73 ] and the Canadian Peer support Accreditation and Certification, a national standard endorsing peer support work as a valuable career, developed in 2017 by PSWs themselves [ 74 ]. The final theme ‘organisational challenges and impact’ included experiences such as PSWs receiving inadequate support, training and supervision, and receiving low pay, leaving them feeling undervalued. Some non-peer staff attitudes were also a reported issue; while some PSWs felt accepted within teams, others experienced negative and rejecting non-peer staff attitudes, such as being treated as patients and not being invited to staff social events. Organisations should prepare, structurally and culturally, for the introduction of PSWs in order to ensure PSW wellbeing and reduce the risk of absences due to sickness [ 68 , 75 ].
Strengths and limitations
We conducted a comprehensive search of several relevant databases and identified a large number of reviews for inclusion, providing the first detailed summary of review findings relating to effectiveness, implementation and experiences of peer support. We also had consistent involvement of researchers with lived experience of mental health and peer support delivery and receipt throughout the design, data screening and extraction, analysis and synthesis, and manuscript drafting for this paper, which allowed lived experience priorities and experiences to guide our approaches to data and our decision making throughout.
We aimed to focus our review on paid peer support; however, this information was underreported in the reviews, and even when reported, interventions were often grouped with peer support interventions that did not fully meet our eligibility criteria (e.g. were unpaid). We also synthesised data from studies where payment status of PSWs was ambiguous, i.e. not reported. This limits our ability to draw firm conclusions around paid peer support specifically, as a significant portion of the data synthesised was from studies investigating unpaid or voluntary peer support. Another limitation was the lack of involvement of people with lived experience in the included reviews, with involvement reported in only one review [ 57 ]. Given the service user-led origins of peer support, future reviews should ensure involvement of people with lived experience. This is addressed in more detail later in this paper. Most included reviews were appraised by the AMSTAR 2 as low or critically low (97%) quality with only one review appraised as high quality. Although the low quality of reviews is a limitation, we aimed to report an overview of all current evidence for peer support to inform policy makers and healthcare practitioners, therefore to maximise the evidence base, we synthesised the reviews scored as ‘critically low quality’. Our ratings are also in line with a prior umbrella review of peer support which rated 87% of reviews as critically low quality and the remainder as low quality, but reported outcomes from all reviews [ 66 ].
Beyond the aforementioned limitations regarding variation in studies within each review, there is also a loss of granular detail through the umbrella review process of summarising data across reviews, which themselves contain many studies which have been summarised. The person-centred nature of peer support may mean that there are meaningful outcomes for the service user which are not easily captured in standard outcome measurement tools or recognised as clinically significant. Variation in peer support roles across studies may have contributed to the contradictions in our findings for RQ3, e.g. the challenges around PSW roles being ambiguous, but also the reported benefits of a flexible role.
A strength of our review was our broad inclusion criteria, for example, for qualitative data on experiences of peer support we reported data from the perspectives of service users, non-peer staff and PSWs. Though some data was reported separately by role, there were studies where experiences were reported together, and these perspectives were difficult to disentangle. Finally, we did not conduct a formal meta-synthesis of the qualitative experiences data; therefore, some detail may have been missed.
Implications for practice
Peer support may be effective at improving some clinical outcomes, self-efficacy and recovery outcomes for some people and could augment the standard service range. Certain groups may benefit from peer support more than others; evidence was strongest for depression outcomes within perinatal populations, but extremely variable for other populations. Peer support may differ in effectiveness depending on population needs and characteristics. PSWs need adequate pay, clear role descriptions and guidelines (e.g. about boundaries and disclosure), ongoing training and supervision, and opportunities for progression. Attitudes about peer support held by non-peer staff may significantly support or impede the implementation and experience of PSWs, and non-peer staff may require training about PSW roles and how to work collaboratively with PSWs. Culture, hierarchical structure and staff acceptability of peer support impact implementation and experience of peer support—structural and cultural change may be required for peer support to succeed, e.g. ensuring a recovery-oriented care model is operating in the service.
Implications for policy
Successful implementation of PSWs in healthcare settings is likely to require a coproduction approach with clearly defined PSW roles, a receptive hierarchical structure and staff, strong leadership and appropriate training (for PSWs and staff) with clinical and/or peer supervision alongside safeguarding. Issues relating to cost, lack of time and lack of resources are key considerations for service providers aiming to implement PSW that is sustained and effective within services. Additionally, Services could benefit from clear, coproduced guidelines, outlining the steps that are most likely to lead to successful PSW implementation.
Implications for research
Future primary and secondary research could usefully explore the differences in efficacy, implementation and experiences in paid PSW over time as it becomes more established; an important distinction as there are likely to be differences in these outcomes as the role of PSW develops. Such studies could consider using more personalised outcome measures such as goal-based outcome measurement [ 76 ]. Current PSW roles are still poorly defined and PSW content, including PSW variations (such as whether PSWs should deliver structured or more loosely structured, informal interventions, or whether interventions should vary according to need and context), need further exploration. Realist investigations around what works for whom, how and in which contexts would uncover more fine-grained detail on the specific contexts and mechanisms that explain these differences. Very few reviews included in this umbrella review reported lived experience researcher leadership or involvement in the undertaking of the study. It is imperative for future research in this area to appropriately reflect the priorities of those who are directly involved in PSW, either as providers or as service users. As the number of PSWs increases and more formalised roles are created, positive impact may not be restricted to outcomes of those supported by PSWs, but also to the functioning of services at an organisational level [ 68 ]. Further research is needed to evaluate how teams function with and without PSWs in order to understand how they may impact experiences through changes at a system level [ 68 ].
Our umbrella review has summarised data from 35 reviews on the effectiveness, implementation, and experiences of peer support for mental health. Although we attempted to focus solely on paid peer support, this detail was often not reported in the reviews. While data on effectiveness was mixed, there was some evidence of improvements on outcomes including depression, particularly perinatal depression, self-efficacy, and recovery, illustrating the potential benefits of wider PSW implementation across mental health services. Good implementation of peer support depends on co-design with people with lived experience, clear job descriptions, a recovery-oriented workplace culture, strong leadership, appropriate training for PSWs and staff , and supervision for PSWs. However due to limited information on cost or cost-effectiveness, we are unable to draw conclusions around resources required to implement PSWs. Experiences of peer support were from a range of perspectives. Peer support was mutually beneficial for PSWs’ and service users’ wellbeing and recovery and PSWs became role models. However, at times PSW roles were ambiguous, this meant that the role was flexible but could also lead to confusion which could impact PSWs own recovery. Potential strategies to successfully implement peer support include that the PSW roles should be clear, PSWs should be appropriately trained and paid, as well as supported and supervised within a trusting and accepting workplace structure and culture that advocates for a recovery-oriented model of care.
Lived experience commentary, written by LM and KM
This study provides a useful summary of the available research on peer support. By providing an overarching review of 35 reviews including 426 available studies, the paper brings together the knowledge on a topic of growing importance and understanding of the experiences, effectiveness, and implementation of peer support. However, this evidence is limited to ‘paid peer support workers’ included in data from academic literature of systematic reviews.
The nature of an umbrella review means that the systematic reviews themselves are synthesised, limiting our ability to look at specific details in the primary studies, for example to look for evidence of lived experience involvement or co-authorship or demographics of participants. The papers within the review are likely to have originated from traditionally funded research enquiries, and an umbrella review potentially magnifies academic or clinical perspectives over user voices and interests. While this is a frustration in any mental-health-related topic, this is particularly concerning in relation to peer support, with its origins in our user-led history.
The roots in user-led peer support are also overlooked when limiting the studies to paid peer support work. Although they might use the same language of mutuality and reciprocity, the two feel different. We are hesitant to suggest that we would prefer the skills and expertise of our supporters to be voluntary and unpaid; we strongly believe their expertise should be valued and funded. But there is something magical about informal peer support which can be lost when it is over-policed in bureaucratic cultures. Additionally, with studies included in the review dating back to 1979, we question how relevant these studies are in informing England’s evolving peer support landscape.
A crucial area of future research is exploring what type of peer support works best for whom and in what circumstances, and how we can deliver this. Furthermore, we need to better understand how NHS cultures can be supported to value the expertise that originates in our lived experience, including the marginalised experiences which have been disproportionately represented in mental health services.
Availability of data and materials
The data used and/or analysed during the current study are available from the corresponding author on reasonable request.
Abbreviations
A MeaSurement Tool to Assess systematic Reviews
Consolidated Framework for Implementation Research
Implementing Recovery through Organisational Change
Lived Experience Working Group
Population, Intervention, Comparator group, Outcome
Peer support worker
Chinman M, George P, Dougherty RH, Daniels AS, Ghose SS, Swift A, et al. Peer support services for individuals with serious mental illnesses: assessing the evidence. Psychiatr Serv. 2014;65:429–41.
Article PubMed Google Scholar
NHS Health Education England: Peer support workers. https://www.hee.nhs.uk/our-work/mental-health/new-roles-mental-health/peer-support-workers . Accessed 4 Aug 2023.
Gillard S. Peer support in mental health services: where is the research taking us, and do we want to go there? J Ment Heal. 2019;28:341–4.
Article Google Scholar
Watson E. The mechanisms underpinning peer support: a literature review. J Ment Heal. 2019;28:677–88.
Salzer MS, Shear SL. Identifying consumer-provider benefits in evaluations of consumer-delivered services. Psychiatr Rehabil J. 2002;25:281–8.
Galloway A, Pistrang N. “We’re stronger if we work together”: experiences of naturally occurring peer support in an inpatient setting. J Ment Heal. 2019;28:419–26.
O’Connell MJ, Flanagan EH, Delphin-Rittmon ME, Davidson L. Enhancing outcomes for persons with co-occurring disorders through skills training and peer recovery support. J Ment Heal. 2020;29:6–11.
Lawn S, Smith A, Hunter K. Mental health peer support for hospital avoidance and early discharge: an Australian example of consumer driven and operated service. J Ment Heal. 2008;17:498–508.
Bellamy C, Schmutte T, Davidson L. An update on the growing evidence base for peer support. Ment Heal Soc Incl. 2017;21:161–7.
Mental Health Mates. https://www.mentalhealthmates.co.uk/our-story/ . Accessed 4 Aug 2023.
Peer Support. https://www.england.nhs.uk/personalisedcare/supported-self-management/peer-support/ . Accessed 4 Aug 2023.
National Voices. Peer support. What is it and does it work ? 2015. p. 58.
Watson E, Meddings S. Peer support in mental health. London: Bloomsbury Publishing; 2019.
Repper J, Aldridge B, Gilfoyle S, Gillard S, Perkins R, Rennison J. Briefing: Peer support workers: theory and practice. CentreformentalhealthOrgUk. 2013. p. 1–16.
Faulkner A, Basset T. A helping hand: taking peer support into the 21st century. Ment Heal Soc Incl. 2012;16:41–7.
NICE. NHS Long Term Plan » NHS Mental Health Implementation Plan 2019/20 – 2023/24. 2019.
Department of Health. The fifth national mental health and suicide prevention plan. 2017.
Farmer P, Dyer J. The five year forward view for mental health. 2016.
Integrated personal commisioning. Community capacity and peer support: summary guide. NHS Engl. 2017:66. https://pdf4pro.com/view/community-capacity-and-peer-support-nhs-england-78a0d2.html . Accesed 5 June 2023.
Mental Health Commission of Canada: Peer Support. https://mentalhealthcommission.ca/what-we-do/access/peer-support/ . Accessed 4 Aug 2023.
Chien WT, Clifton AV, Zhao S, Lui S. Peer support for people with schizophrenia or other serious mental illness. Cochrane Database Syst Rev. 2019;2019:CD010880.
PubMed Central Google Scholar
Lloyd-Evans B, Mayo-Wilson E, Harrison B, Istead H, Brown E, Pilling S, et al. A systematic review and meta-analysis of randomised controlled trials of peer support for people with severe mental illness. BMC Psychiatry. 2014;14:1–12.
du Plessis C, Whitaker L, Hurley J. Peer support workers in substance abuse treatment services: a systematic review of the literature. J Subst Use. 2020;25:225–30.
Ibrahim N, Thompson D, Nixdorf R, Kalha J, Mpango R, Moran G, et al. A systematic review of influences on implementation of peer support work for adults with mental health problems. Soc Psychiatry Psychiatr Epidemiol. 2020;55:285–93.
Belbasis L, Bellou V, Ioannidis JPA. Conducting umbrella reviews. BMJ Med. 2022;1:e000071.
Article PubMed PubMed Central Google Scholar
Aromataris E, Fernandez R, Godfrey CM, Holly C, Khalil H, Tungpunkom P. Summarizing systematic reviews: methodological development, conduct and reporting of an umbrella review approach. Int J Evid Based Healthc. 2015;13:132–40.
Fusar-Poli P, Radua J. Ten simple rules for conducting umbrella reviews. Evid Based Ment Health. 2018;21:95–100.
Higgins JPT, Thomas J, Chandler J, Cumpston M, Li T, Page MJ WV (editors), editor. Cochrane Handbook for Systematic Reviews of Interventions version 6.3 (updated February 2022). Cochrane, 2022. Available from www.training.cochrane.org/handbook .
Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. 2020;2021:372.
Google Scholar
Cooper R, Saunders K. The effectiveness, implementation, and experiences of peer support approaches for mental health: an umbrella review of reviews. PROSPERO 2022 CRD42022362099. 2022. Available from: https://www.crd.york.ac.uk/prospero/display_record.php?ID=CRD42022362099 .
Aromataris E, Fernandez R, Godfrey C, Holly C, Khalil H, Tungpunkom P. Chapter 10: Umbrella Reviews. In: Aromataris E, Munn Z (editors). JBI manual for evidence synthesis. JBI. 2020. https://doi.org/10.46658/JBIMES-20-11 . Available from: https://synthesismanual.jbi.global .
Shea BJ, Reeves BC, Wells G, Thuku M, Hamel C, Moran J, et al. AMSTAR 2: a critical appraisal tool for systematic reviews that include randomised or non-randomised studies of healthcare interventions, or both. BMJ. 2017;358:1–9.
Damschroder LJ, Aron DC, Keith RE, Kirsh SR, Alexander JA, Lowery JC. Fostering implementation of health services research findings into practice: a consolidated framework for advancing implementation science. Implement Sci. 2009;4:1–15.
Bailie HA, Tickle A. Effects of employment as a peer support worker on personal recovery: a review of qualitative evidence. Ment Heal Rev J. 2015;20:48–64.
Lyons N, Cooper C, Lloyd-Evans B. A systematic review and meta-analysis of group peer support interventions for people experiencing mental health conditions. BMC Psychiatry. 2021;21:1–17.
Fortuna KL, Naslund JA, LaCroix JM, Bianco CL, Brooks JM, Zisman-Ilani Y, et al. Digital peer support mental health interventions for people with a lived experience of a serious mental illness: systematic review. JMIR Ment Heal. 2020;7:e16460.
Fuhr DC, Salisbury TT, De Silva MJ, Atif N, van Ginneken N, Rahman A, et al. Effectiveness of peer-delivered interventions for severe mental illness and depression on clinical and psychosocial outcomes: a systematic review and meta-analysis. Soc Psychiatry Psychiatr Epidemiol. 2014;49:1691–702.
Gaiser MG, Buche JL, Wayment CC, Schoebel V, Smith JE, Chapman SA, et al. A systematic review of the roles and contributions of peer providers in the behavioral health workforce. Am J Prev Med. 2021;61:e203–10.
Ong QS, Yang HZ, Kuek JHL, Goh YS. Implementation of peer-support services in Asia: a scoping review. J Psychiatr Ment Health Nurs. 2022;30:309–25.
Peck CKH, Thangavelu DP, Li Z, Goh YS. Effects of peer-delivered self-management, recovery education interventions for individuals with severe and enduring mental health challenges: a meta-analysis. J Psychiatr Ment Health Nurs. 2023;30:54–73.
Pitt VJ, Lowe D, Prictor M, Hetrick S, Ryan R, Berends L, et al. A systematic review of consumer-providers’ effects on client outcomes in statutory mental health services: the evidence and the path beyond. J Soc Social Work Res. 2013;4:333–56.
Pitt V, Lowe D, Hill S, Prictor M, Hetrick SE, Ryan R, et al. Consumer-providers of care for adult clients of statutory mental health services. Cochrane Database Syst Rev. 2013;2013:CD004807.
PubMed PubMed Central Google Scholar
Sun J, Yin X, Li C, Liu W, Sun H. Stigma and peer-led interventions: a systematic review and meta-analysis. Front Psychiatry. 2022;13:1–12.
Wang Y, Chen Y, Deng H. Effectiveness of family-and individual-led peer support for people with serious mental illness a meta-analysis. J Psychosoc Nurs Ment Health Serv. 2022;60:20–6.
White S, Foster R, Marks J, Morshead R, Goldsmith L, Barlow S, et al. The effectiveness of one-to-one peer support in mental health services: a systematic review and meta-analysis. BMC Psychiatry. 2020;20:1–20.
Mutschler C, Bellamy C, Davidson L, Lichtenstein S, Kidd S. Implementation of peer support in mental health services: a systematic review of the literature. Psychol Serv. 2022;19:360–74.
Fang Q, Lin L, Chen Q, Yuan Y, Wang S, Zhang Y, et al. Effect of peer support intervention on perinatal depression: a meta-analysis. Gen Hosp Psychiatry. 2022;74:78–87.
Huang R, Yan C, Tian Y, Lei B, Yang D, Liu D, et al. Effectiveness of peer support intervention on perinatal depression: a systematic review and meta-analysis. J Affect Disord. 2020;276:788–96.
Jones CCG, Jomeen J, Hayter M. The impact of peer support in the context of perinatal mental illness: a meta-ethnography. Midwifery. 2014;30:491–8.
Triece P, Massazza A, Fuhr DC. Effectiveness and implementation outcomes for peer-delivered mental health interventions in low- and middle-income countries: a mixed-methods systematic review. Soc Psychiatry Psychiatr Epidemiol. 2022;57:1731–47.
Burke E, Pyle M, Machin K, Varese F, Morrison AP. The effects of peer support on empowerment, self-efficacy, and internalized stigma: a narrative synthesis and meta-analysis. Stigma Heal. 2019;4:337–56.
Smit D, Miguel C, Vrijsen JN, Groeneweg B, Spijker J, Cuijpers P. The effectiveness of peer support for individuals with mental illness: systematic review and meta-analysis. Psychol Med. 2022;53:5332–41.
Bassuk EL, Hanson J, Greene RN, Richard M, Laudet A. Peer-delivered recovery support services for addictions in the united states: a systematic review. J Subst Abuse Treat. 2016;63:1–9.
Reif S, Braude L, Lyman DR, Dougherty RH, Daniels AS, Ghose SS, et al. Peer recovery support for individuals with substance use disorders: assessing the evidence. Psychiatr Serv. 2014;65:853–61.
Lewis HK, Foye U. From prevention to peer support: a systematic review exploring the involvement of lived-experience in eating disorder interventions. Ment Heal Rev J. 2022;27:1–17.
Pellizzer ML, Wade TD. The effectiveness of lived experience involvement in eating disorder treatment: a systematic review. Int J Eat Disord. 2022;56:331–49.
Schlichthorst M, Ozols I, Reifels L, Morgan A. Lived experience peer support programs for suicide prevention: a systematic scoping review. Int J Ment Health Syst. 2020;14:1–13.
Bowersox NW, Jagusch J, Garlick J, Chen JI, Pfeiffer PN. Peer-based interventions targeting suicide prevention: a scoping review. Am J Community Psychol. 2021;68:232–48.
Zeng G, McNamara B. Strategies used to support peer provision in mental health: a scoping review. Adm Policy Ment Heal Ment Heal Serv Res. 2021;48:1034–45.
Åkerblom KB, Ness O. Peer Workers in co-production and co-creation in mental health and substance use services: a scoping review. Adm Policy Ment Heal Ment Heal Serv Res. 2023;50:296–316.
Walker G, Bryant W. Peer support in adult mental health services: a metasynthesis of qualitative findings. Psychiatr Rehabil J. 2013;36:28–34.
Vandewalle J, Debyser B, Beeckman D, Vandecasteele T, Van Hecke A, Verhaeghe S. Peer workers’ perceptions and experiences of barriers to implementation of peer worker roles in mental health services: a literature review. Int J Nurs Stud. 2016;60:234–50.
Miyamoto Y, Sono T. Lessons from peer support among individuals with mental health difficulties: a review of the literature. Clin Pract Epidemiol Ment Heal. 2012;8:22–9.
Viking T, Wenzer J, Hylin U, Nilsson L. Peer support workers’ role and expertise and interprofessional learning in mental health care: a scoping review. J Interprof Care. 2022;36:828–38.
Article CAS PubMed Google Scholar
Tricco AC, Lillie E, Zarin W, O’Brien KK, Colquhoun H, Levac D, et al. PRISMA extension for scoping reviews (PRISMA-ScR): checklist and explanation. Ann Intern Med. 2018;169:467–73.
Yim CST, Chieng JHL, Tang XR, Tan JX, Kwok VKF, Tan SM. Umbrella review on peer support in mental disorders. Int J Ment Health. 2023;52:379–400.
Ali K, Farrer L, Gulliver A, Griffiths KM. Online peer-to-peer support for young people with mental health problems: a systematic review. JMIR Ment Heal. 2015;2:1–9.
Repper J, Aldridge B, Gilfoyle S, Gillard S, Perkins R, Rennison J. Peer support workers: a practical guide to implementation. 2013:1–32.
Te Pou. Competencies for the mental health and addiction service user, consumer and peer workforce. 2014:1–26. https://www.hqsc.govt.nz/assets/Our-work/Mental-health-and-addiction/Resources/DG038-Te-Poucompetencies-for-mental-health.pdf . Accessed 4 Aug 2023.
Te Pou. Competencies for the mental health and addiction consumer, peer support and lived experience workforce. 2021:1–26.
Foglesong D, Knowles K, Cronise R, Wolf J, Edwards JP. National practice guidelines for peer support specialists and supervisors. Psychiatr Serv. 2022;73:215–8.
Ball M, Skinner S. Raising the glass ceiling : considering a career pathway for peer support workers - 2021. 2021.
National Health Service [NHS]. The competence framework for mental health peer support workers. 2020.
Peer C, Mentors S. Peer Support Accreditation and Certification (Canada). National Certification Handbook. 2014.
Poremski D, Kuek JHL, Yuan Q, Li Z, Yow KL, Eu PW, et al. The impact of peer support work on the mental health of peer support specialists. Int J Ment Health Syst. 2022;16:1–8.
Law D. The Goal-based Outcome (GBO) tool guidance notes. 2019.
Download references
Acknowledgements
This work is supported by the NIHR UCLH BRC.
This study is funded by the National Institute for Health and Care Research (NIHR) Policy Research Programme. The views expressed are those of the author(s) and not necessarily those of the NIHR or the Department of Health and Social Care.
Author information
Ruth E. Cooper and Katherine R. K. Saunders are joint first-authors.
Authors and Affiliations
NIHR Mental Health Policy Research Unit, Institute of Psychiatry, Psychology and Neuroscience, King’s College London, London, UK
Ruth E. Cooper, Katherine R. K. Saunders, Jessica Griffiths, Ruth Stuart & Alan Simpson
NIHR Mental Health Policy Research Unit, Division of Psychiatry, University College London, London, UK
Anna Greenburgh, Rebecca Appleton, Phoebe Barnett, Sophie M. Allan, Brynmor Lloyd-Evans & Sonia Johnson
Centre for Outcomes Research and Effectiveness, Research Department of Clinical, Educational and Health Psychology, University College London, London, UK
Phoebe Barnett
National Collaborating Centre for Mental Health, Royal College of Psychiatrists, London, UK
University of East Anglia, Norwich, UK
Sophie M. Allan
MHPRU Lived Experience Working Group, London, UK
Prisha Shah, Karen Machin, Tamar Jeynes, Lizzie Mitchell, Beverley Chipp & Stephen Jeffreys
Florence Nightingale Faculty of Nursing, Midwifery and Palliative Care, London, UK
Alan Simpson
Camden and Islington NHS Foundation Trust, London, UK
Sonia Johnson
You can also search for this author in PubMed Google Scholar
Contributions
All authors (RC, KS, AG, PS, RA, KM, TJ, PB, SA, JG, RS, LM, BC, SJ, BLE, AS, SJ) substantially contributed to the conception or design of this study. Data acquisition was undertaken by: KS, RC, JG, RS, RA, KM, PS, SA, PB. The data were synthesised and interpreted by: KS, AG, RA, PS, KM, TJ, and RC. KS and RC led on drafting the manuscript with input and/or editing by all other authors (AG, PS, RA, KM, TJ, PB, SA, JG, RS, LM, BC, SJ, BLE, AS, SJ). All authors (RC, KS, AG, PS, RA, KM, TJ, PB, SA, JG, RS, LM, BC, SJ, BLE, AS, SJ) read and approved the final manuscript.
Authors’ Twitter handles
Twitter handles: @soniajohnson (Sonia Johnson); @cityalan (Alan Simpson); @MentalHealthPRU (Mental Health Policy Research Unit).
Corresponding authors
Correspondence to Ruth E. Cooper or Katherine R. K. Saunders .
Ethics declarations
Ethics approval and consent to participate.
Not applicable.
Consent for publication
Competing interests.
KM is a Director of With-you Consultancy Ltd who provide peer support training and consultancy. All other authors declare no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1: appendix 1..
Prisma checklist [ 29 ]. Appendix 2. Full search strategy. Appendix 3. AMSTAR2 ratings. Appendix 4. Excluded studies following full text screening, with reasons. Appendix 5. Study overlap. Appendix 6. Effectiveness of peer support outcomes: results for non-meta-analysis results. Appendix 7. Experiences of peer support (detailed themes).
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Cooper, R.E., Saunders, K.R.K., Greenburgh, A. et al. The effectiveness, implementation, and experiences of peer support approaches for mental health: a systematic umbrella review. BMC Med 22 , 72 (2024). https://doi.org/10.1186/s12916-024-03260-y
Download citation
Received : 07 November 2023
Accepted : 15 January 2024
Published : 29 February 2024
DOI : https://doi.org/10.1186/s12916-024-03260-y
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Peer support
- Mental health
- Systematic review
- Umbrella review
BMC Medicine
ISSN: 1741-7015
- General enquiries: [email protected]
This paper is in the following e-collection/theme issue:
Published on 9.6.2020 in Vol 7 , No 6 (2020) : June
Peer Support in Mental Health: Literature Review
Authors of this article:

- Reham A Hameed Shalaby * , MD ;
- Vincent I O Agyapong * , MD, PhD
Department of Psychiatry, University of Alberta, Edmonton, AB, Canada
*all authors contributed equally
Corresponding Author:
Reham A Hameed Shalaby, MD
Department of Psychiatry
University of Alberta
1E1 Walter Mackenzie Health Sciences Centre
8440 112 St NW
Edmonton, AB, T6G 2B7
Phone: 1 4034702050
Email: [email protected]
Background: A growing gap has emerged between people with mental illness and health care professionals, which in recent years has been successfully closed through the adoption of peer support services (PSSs). Peer support in mental health has been variously defined in the literature and is simply known as the help and support that people with lived experience of mental illness or a learning disability can give to one another. Although PSSs date back to several centuries, it is only in the last few decades that these services have formally evolved, grown, and become an integral part of the health care system. Debates around peer support in mental health have been raised frequently in the literature. Although many authors have emphasized the utmost importance of incorporating peer support into the health care system to instill hope; to improve engagement, quality of life, self-confidence, and integrity; and to reduce the burden on the health care system, other studies suggest that there are neutral effects from integrating PSSs into health care systems, with a probable waste of resources.
Objective: In this general review, we aimed to examine the literature, exploring the evolution, growth, types, function, generating tools, evaluation, challenges, and the effect of PSSs in the field of mental health and addiction. In addition, we aimed to describe PSSs in different, nonexhaustive contexts, as shown in the literature, that aims to draw attention to the proposed values of PSSs in such fields.
Methods: The review was conducted through a general search of the literature on MEDLINE, Google Scholar, EMBASE, Scopus, Chemical Abstracts, and PsycINFO. Search terms included peer support, peer support in mental health, social support, peer, family support, and integrated care.
Results: There is abundant literature defining and describing PSSs in different contexts as well as tracking their origins. Two main transformational concepts have been described, namely, intentional peer support and transformation from patients to peer support providers. The effects of PSSs are extensive and integrated into different fields, such as forensic PSSs, addiction, and mental health, and in different age groups and mental health condition severity. Satisfaction of and challenges to PSS integration have been clearly dependent on a number of factors and consequently impact the future prospect of this workforce.
Conclusions: There is an internationally growing trend to adopt PSSs within addiction and mental health services, and despite the ongoing challenges, large sections of the current literature support the inclusion of peer support workers in the mental health care workforce. The feasibility and maintenance of a robust PSS in health care would only be possible through collaborative efforts and ongoing support and engagement from all health care practitioners, managers, and other stakeholders.
Introduction
Peer support services (PSSs) are novel interventions recently adopted in mental health systems worldwide. It is believed, however, that PSSs date back to more than three centuries to the moral treatment era [ 1 ], albeit on an informal basis. Diverse definitions and classifications for PSSs have been provided in the literature [ 2 - 4 ], and numerous reports have praised and supported the service provided by peer support workers (PSWs) [ 5 - 8 ]. However, other literature suggests the neutral effects of PSSs, with weak associated evidence to support such services [ 9 , 10 ]. The potential impact of PSWs on their peers [ 11 - 14 ] has received considerable attention in the literature.
PSSs have been introduced in different contexts, such as family PSWs [ 15 - 19 ], the forensic field [ 20 , 21 ], and online PSSs. A considerable number of strategies were proposed to generate an effective PSS in the mental health field amid a number of associated concerns and challenges [ 22 - 25 ].
This general review sheds light on PSWs’ experiences, benefits, challenges, opportunities to expand access to quality addiction, and mental health care using PSSs. The review was conducted through a general search of the literature on MEDLINE, Google Scholar, EMBASE, Scopus, Chemical Abstracts, and PsycINFO. Search terms included peer support, peer support in mental health, social support, peer, family support, and integrated care. We began the review with an examination of the definitions, origins, and types of peer support contributions and within different clinical contexts, aiming at deepening the view to the diverse effects of such a workforce. We then continued with examining the transition from a patient role to a PSW role and their incorporation into mental health systems. Thereafter, we provided a conceptual framework for the effects of peer support and stigma in relation to PSWs. We concluded the review by examining the benefits and challenges associated with PSSs and provided a commentary on future directions for PSSs in mental health.
Definitions
Peer support has diverse meanings in the literature. For example, it is a system of giving and receiving help founded on key principles of respect, shared responsibility, and an agreement of what is helpful [ 26 ]. A peer is defined as an equal , someone with whom one shares demographic or social similarities, whereas support refers to “the kind of deeply felt empathy, encouragement, and assistance that people with shared experiences can offer one another within a reciprocal relationship” [ 3 ]. The Mental Health Foundation in the United Kingdom defined peer support in mental health as “the help and support that people with lived experience of a mental illness or a learning disability can give to one another” [ 27 ]. Peer employees were also defined as “individuals who fill designated unique peer positions as well as peers who are hired into traditional MH positions” [ 28 ]. In 1976, authors defined self-help groups as “voluntary small group structures for mutual aid in the accomplishment of a specific purpose...usually formed by peers who have come together for mutual assistance in satisfying a common need, overcoming a common handicap or life-disrupting problem, and bringing about desired social and/or personal change” [ 28 ]. Although the mutual relationship was sometimes overlooked and rather described as an asymmetric or nearly one-directional relationship [ 29 ], it is emphasized upon as 1 of the 4 main tasks for peer support accomplishments, which are mutuality, connection, worldwide, and moving toward rather than moving away [ 30 ].
Origin and Growth of Peer Support
Davidson et al [ 11 ] have expressed the paradigm that calls for new models of community-based practice, which turned away from case management and from conceptualizing old practices under new terms. In the 1990s, peer support was formally introduced as a service in community mental health care. However, there is evidence of its practice throughout history, including during the moral treatment era in France at the end of the 18th century [ 1 ]. Recently, peer support has been rapidly growing in many countries and could attract a considerable amount of research [ 22 ]. Although Lunatic Friends’ Society is known as the earliest peer support group in mental health, which was founded in England in the middle of the 19th century [ 31 ], self-help groups were described as the oldest and most pervasive of peer support types [ 28 ]. Some peer-run groups also formed in Germany in the late 19th century, which protested on involuntary confinement laws. In addition to this, several individuals in the 18th and 19th centuries publicized their protests about their treatment in autobiographies and petitions [ 32 ]. The origin of peer support even reaches further back than the earliest asylums [ 33 ]. Some authors suggest that peer support is not based on psychiatric models and diagnostic criteria [ 3 ]; however, it is about “understanding another’s situation empathically through the shared experience of emotional and psychological pain” [ 34 ]. In the United States, the start of legitimacy for peer support was ignited in 2007 by considering the conditions under which PSSs could be reimbursed by Medicaid [ 35 ]. Although this reform was entailing a recovery model, which has been adopted by health care providers and stakeholders in many “English-speaking” countries, it was not the case in many other countries, in which this reform was yet to be well formulated [ 36 ].
Transformational Concepts in Peer Support Service
Intentional peer support: informal to formal peer support evolution.
Intentional peer support (IPS) is described as a philosophical descendant of the informal peer support of the ex-patients’ movement in the 1970s [ 3 ]. It depends on a way of communication that immerses the provider into the recipient experience by stepping back from one’s story and being eagerly open to others’ stories [ 30 ]. In the field of psychiatry, trauma is blamed for playing a pivotal role in the experience, diagnosis, and treatment, and peer support is described as the logical environment for disseminating trauma-informed care (TIC) or service, which enables building relationships based on mutuality, shared power, and respect [ 37 ]. In the same context, trauma-informed peer support usually begins with the main question, “What happened to you?” instead of “What is wrong with you?” [ 30 ]. TIC is an explanatory model that identifies PSWs sharing lived experiences, ensuring safety and functioning as an advocate, and a liaison to patient management plans, where empowerment and intervention models are strongly emphasized upon [ 38 , 39 ]. The shift from a traditional biomedical model to recovery-oriented practice is meant to perceive trauma as a coping mechanism rather than a pathology [ 38 , 40 ]. This clearly entails training of all service providers for better acknowledgment and comfort in dealing with trauma survivors , with an understanding of trauma as an expectation rather than an exception [ 41 ]. Although the TIC concept has evolved over the years, it still lacks guidance, training, staff knowledge, and governmental support, which are necessary to ensure successful policy implementation [ 40 ]. The role of PSWs also extended to support those at risk of trauma events because of the nature of their work, including child protection workers, who are at risk of posttraumatic stress disorder or anxiety disorder [ 42 ]. Although IPS grew from the informal practices of grassroots-initiated peer support, it differs from earlier approaches because it is a theoretically based, manualized approach with clear goals and a fidelity tool for practitioners [ 14 ]. It instead focuses on the nature and purpose of the peer support relationship and its attention to skill building to purposefully engage in peer support relationships that promote mutual healing and growth [ 3 ]. Transitioning from informal to formal roles provides not only well-formulated expectations of the role but also a better chance to identify the potential conflict of the PSWs’ mixed identity [ 43 ].
Research conducted on PSWs has been conceptualized throughout history [ 22 ]. Starting with feasibility studies, at the initial stage, it is followed by studies comparing peer staff with nonpeer staff and, finally, the studies that answer questions such as the following:
- Do interventions provided by peers differ from those provided by nonpeers?
- What makes peer support a unique form of service delivery?
If so, to the previous question, what are the active ingredients of these aspects of peer support, and what outcomes can they produce?
Studies that provide answers to the latter set of questions are expected to provide a deeper understanding of the philosophical underpinnings of the IPS concept for PSSs.
The Transformation From Patient to Peer Support Providers
The shift from being a service recipient to a service provider has been contributing as a driving force to restore fundamental human rights, especially among those with serious mental illnesses (SMIs) [ 22 ]. Telling the personal lived experience leads to a profound shift, from telling an “illness story” to a “recovery story” [ 4 ]. This involved an identity transformation from being perceived as a victim or a patient to a person fully engaged in life with various opportunities ahead [ 4 ]. This transition is seen as a gradual process and one that is supported by several other personal changes with expected challenges [ 44 ]. Moving a full circle to include PSWs as the service provider has been undertaken by mental health services to further exceed the transformational role, which was primarily the main aim of providing such a service [ 45 ]. A liminal identity was given for PSWs as laying between several roles, being service users, friends, and staff. Thus, the professionalism of the PSW role might not be a successful way to ensure individual well-being or to promote the peer support initiative [ 46 ]. Thus, successful transitioning from the patient to PSW role involves fundamental functional shifts achieved through overcoming multiple barriers at the personal, health system, and societal levels.
Effects of Peer Support Service in Different Contexts
Trained PSWs or mentors can use communication behaviors useful to different client groups. Many studies showed the effectiveness and feasibility of applying for peer support as follows:
Severe or Serious Mental Illness
Generally, the evidence for peer support interventions for people with SMIs has been described as moderate to limited with mixed intervention effects [ 2 , 47 ]. On the one hand, adding PSSs to intensive case management teams proved to improve activation in terms of knowledge, skills, confidence, and attitudes for managing health and treatment. Hence, patients become healthier, report better quality of life (QOL), engage in more health care practices, and report more treatment satisfaction [ 48 , 49 ]. On the other hand, a systematic review of randomized controlled trials (RCTs) involving adults with SMIs, while showing some evidence of positive effects on measures of hope, recovery, and empowerment at and beyond the end of the PSS intervention in this review, did not show any positive effects on hospitalization, satisfaction, or overall symptoms [ 10 ]. Similarly, a Cochrane systematic review of PSSs for people with schizophrenia found inconclusive results, with a high risk of bias in most of the studies and insufficient data to support or refute the PSS for this group [ 50 ].
Addiction and Drug Users
In recent years, peer recovery support services have become an accepted part of the treatment for substance use disorders, providing a more extensive array of services that are typically associated with the mutual supportive intervention [ 51 ]. This is in contrast to the use of peer support for SMIs where evidence is still developing. The Substance Abuse and Mental Health Services Administration (SAMHSA) defined peer recovery support for substance use disorders as “a set of nonclinical, peer-based activities that engage, educate, and support individuals so that they can make life changes that are necessary to recover from substance use disorders” [ 51 ]. Despite the long-term nature of substance abuse, immersion in peer support groups and activities and active engagement in the community are considered the 2 critical predictors of recovery for more than half the dependent substance users [ 52 ].
A number of trials studied the peer support effect on drug users, especially in the emergency department [ 53 , 54 ]. Another randomized trial found that a socially focused treatment can affect change in the patient’s social network and hence increase support for abstinence, for example, an increase of one nondrinking friend in the social network is translated into a 27% increase in the probability of reporting abstinence on 90% of days or more at all follow-up visits, which extended to 15 months [ 55 ].
Forensic Peer Support Service
The forensic peer system refers to the engagement of peer specialists who have histories of mental illness as well as criminal justice involvement and who are trained to help other patients sharing similar accounts [ 20 ]. As referred to by Davidson and Rowe [ 20 ], “Forensic Peer Specialists embody the potential for recovery for people who confront the dual stigmas associated with SMI and criminal justice system involvement.”
They offer day-to-day support for those released early from jail by accompanying them to initial probation meetings or treatment appointments and referring them to potential employers and landlords, helping people to negotiate and minimize continuing criminal sanctions and training professional staff on engaging consumers with criminal justice history [ 20 , 21 ]. PSWs with incarceration histories could successfully identify the liminal space in being supportive rather than providing support for the criminal offense, in contrast with the conventional methods that directly confront criminality [ 56 ]. In fact, having criminal history is the “critical component” for achieving recovery [ 56 ]. Multiple initiatives have been introduced to facilitate a reentry process for people recently released from incarceration, including Forensic Assertive Community Treatment, Assertive Community Treatment, Critical Time Intervention, and Women’s Initiative Supporting Health Transitions Clinic, through diverse community support groups involving PSWs [ 57 , 58 ].
A peer support program undertaken by older community volunteers was effective in improving general and physical health, social functioning, depression parameters, and social support satisfaction, especially in socially isolated, low-income older adults [ 59 ]. The Reclaiming Joy Peer Support intervention (a mental health intervention that pairs an older adult volunteer with a participant) has the potential for decreasing depression symptoms and improving QOL indicators for both anxiety and depression [ 60 ]. Engaging the community in health research could be of a high value in acknowledging their own health needs [ 61 ].
Youth and Adolescents
Peer support programs are mostly needed for university students, where challenges with loneliness and isolation are well recognized [ 62 ]. Hence, a need emerged for training peers to support their peer adolescents with the prospective challenges at this age [ 63 ]. Trained peer support students without necessarily having a lived experience were also examined in England [ 64 ]. The study included university students measuring the acceptability and impact of the volunteer peer support program through 6 weekly sessions. Students with lower mental well-being were more likely to complete the course, and an improvement in mental well-being was recorded for those who attended more frequently. Overall, peers remain to be an essential source of support for young people experiencing mental health and substance use problems [ 65 ].
Medically and Socially Disadvantaged Subgroups
A peer-led, medical self-management program intervention has been beneficial for medically and socially disadvantaged subgroups [ 60 ]. The Reclaiming Joy Peer Support intervention has the potential for increasing QOL and reducing depression in low-income older adults who have physical health conditions [ 60 ]. Similarly, for those who are “hardly reached,” it was indicated that the PSS provided is even more effective in these marginalized populations [ 66 ]. A Health and Recovery Peer program was delivered by mental health peer leaders for people with SMIs, resulting in an improvement in the physical health–related QOL parameters such as physical activity and medication adherence [ 49 ]. Peer-delivered and technology-supported interventions are feasible and acceptable and are associated with improvements in psychiatric, medical self-management skills, QOL, and empowerment of older adults with SMIs and or chronic health conditions [ 67 , 68 ].
Persons With Disabilities
The United Nations’ Convention on the Rights of Persons with Disabilities (CRPD) was adopted in 2007 and stated that “persons with disabilities should have equal recognition before the law and the right to exercise their legal capacity” [ 69 - 71 ]. Therefore, a positive emphasis upon the supported decision making and the fight against discrimination is evident through the convention. Nevertheless, these initiatives have been perceived as incomplete considering many challenges such as the community social status and ongoing perceived stigma of people with disabilities (PWDs) [ 70 , 72 ]. “Circle of support” is an elaborate example of an applicable peer support model for PWDs that has helped in decision making and facilitating communication [ 70 , 73 , 74 ]. This is clearly aligned with the paradigm shift from the biomedical to the socially supportive model of disability, which was provided by CRPD [ 70 ].
Peer Support for Families
Families may act either as sources of understanding and support or stigmatization through ignorance, prejudice, and discrimination, with subsequent negative impact [ 19 ]. In addition, the distress and burden associated with caring for a family member with mental illness are evident, where 29% to 60% endure significant psychological distress [ 17 ]. Family support can be financial or emotional; however, moral support was perceived as the substantial motivating factor for relatives who are ill [ 19 ]. In the last few decades, consistent and growing evidence that supports the inclusion of family members in the treatment and care of their misfortunate relatives has been developed. This has been mainly evident in the youth mental health system that urged the transformation change, which incorporates family members in the health care service provided to their youth [ 18 , 75 ]. Many PSWs have been engaged in family psychoeducation as family peers or parent partners, especially for those with the first episode of psychosis [ 76 ]. Although familial education is crucial and needs to be provided through different scales [ 19 ], an extensive matching of PSWs and the caregivers has not been perceived as a necessity to create a successful volunteer mentoring relationship [ 77 ]. Multiple initiatives have taken place all over the world. In India, a program titled “Saathi” was established for family members of residential and outpatient mental health service users that had dual goals of offering information and developing a peer support mechanism for family members of people with different mental health conditions [ 19 ]. In Melbourne, Australia, “Families Helping Families” was developed, where family PSWs are positioned in the service assessment area and in the inpatient unit to ensure early involvement [ 18 ]. An impressive peer support guide for parents of children or youth with mental health problems is provided by the Canadian Mental Health Association, British Colombia Division [ 15 ]. In Ontario, family matters programs are provided through provincial peer support programs [ 16 ].
The term “transforming mental health care” entails active involvement of families in orienting the mental health system toward recovery [ 78 ]. Family members are to have access to timely and accurate information that promotes learning, self-monitoring, and accountability [ 79 ]. The inclusion of family members as partners of the medical service is the new philosophy, with a subsequent shift from the concept of clinic-based practice to a community-based service approach [ 78 ].
Peer Support Service in Low- and Middle-Income Countries
Several initiatives took place in low- and middle-income countries, such as in rural Uganda, where a trained peer-led team provided 12 successful training sessions of perinatal service for a group of parents over a 6-month period, which resulted in better maternal well-being and child development, compared with another control group [ 80 ]. Similarly, successful community peer groups were conducted in rural India and Nepal, with high feasibility and effectiveness rates, and perceived as “potential alternative to health-worker-led interventions” [ 81 - 83 ]. In addition, adding counseling and social support groups entailing PSWs to the conventional medication treatment for patients with psychotic disorders was tried in a cohort study in Uganda; however, the results were not significantly different from those who received only medications [ 84 ]. This might be because of the underpowering of community services offered, compared with the robust medication regimens [ 85 ].
It is evident from the aforementioned information that there is mixed evidence on the effectiveness of PSW interventions in different contexts. For example, for patients with SMIs, systematic reviews suggest that there is some evidence of positive effects on measures of hope, recovery, and empowerment but no positive effects on hospitalization, satisfaction, or overall symptoms [ 10 ]. Similarly, for patients with addiction issues, although being involved in a peer network did not reduce social assistance for alcohol, they somewhat increased behavioral and attitudinal support for abstinence as well as involvement with Alcoholics Anonymous [ 55 ]. Furthermore, although many observational studies support the PSW role in the other contexts described above, there is a current dearth of literature involving RCTs and systematic reviews reporting on the effectiveness of PSWs in these specific contexts. Thus, there exist opportunities for conducting RCTs in the described contexts.
The Conceptual Framework for the Effects of Peer Support Service
The conceptual framework is based on empirical evidence, suggesting that the impact of PSWs reflects upon the recipients of such a service [ 4 , 76 , 86 - 90 ], the global health system [ 22 , 47 , 76 , 86 , 91 , 92 ], and the PSWs themselves [ 13 , 28 , 76 , 93 ], as shown in Figure 1 . The framework has, therefore, been developed by authors through a general review of the literature that examines the effects of PSSs on patients, health care systems, and also PSWs themselves so as to provide evidence-based material supporting all possible effects of PSW roles.
Supportive social relationships can have a dual opposing effect on individuals’ lives, either as a family member or as social and professional networks through sharing their disappointments and pains or their joy and successes [ 11 ]. Useful roles for PSSs are identified in many studies. For example, adding 3 peer specialists to a team of 10 intensive case managers provided better QOL with greater satisfaction [ 12 ], stigma reduction, and less health service utilization [ 89 , 91 ]. The economic impact of PSSs has been extensively studied in the literature, concluding cost containment for the health care system in terms of reduction of readmission rates, emergency visits, and fewer hospital stays, which altogether substantially exceed the cost of running a peer support program [ 92 ]. Moreover, PSWs are looked at as providers of a service at a cheaper cost compared with other health care providers [ 94 , 95 ]. For example, about US $23,000 is paid to PSWs in the United States compared with around US $100,000 for a nurse practitioner [ 96 ]. However, a PSS is not posited as a substitute for clinical services, rather it is perceived as an intrapersonal and social service that provides a dual role of effective service and with humanizing care and support [ 14 , 26 , 97 ]. This role extends to cover PSWs themselves, in terms of improved overall well-being and self-confidence, reframing identity, and enhancing responsibility either toward themselves or their peers [ 13 , 93 ].

Although PSWs can play a variety of tasks, managers who hire them may want to ensure that improving patient activation is included in their range of duties [ 48 ]. In 2 concurrent studies, a significant increase in QOL satisfaction, reduction of rehospitalization rates, and reduction in the number of hospital days were recorded when adding PSSs to usual care [ 22 , 98 ]. In another study engaging 31 peer providers in diverse mental health, agencies identified 5 broad domains of wellness, including foundational, emotional, growth and spiritual, social, and occupational wellness [ 4 ]. In a systematic literature review for people with SMIs, peer-navigator interventions and self-management were the most promising interventions [ 47 ]. PSWs’ effects are diversified through sharing in different contexts. For example, positive impacts on the physical health of their peers have been recorded [ 49 ]. Peer-based approaches have been used to deliver behavioral weight loss interventions [ 90 ]. For young students, structured peer support for depression may have benefits in improving students’ mental well-being [ 64 ]. In the case of crisis houses, greater satisfaction was achieved through a provided informal PSS [ 99 ]. Robust studies, therefore, recommend implementing peer support programs [ 10 , 18 ].
On the other hand, authors found that PSSs met moderate levels of evidence and that effectiveness varied across service types, for example, with “peers in existing clinical roles” was described as being less effective than the “peer staff added to traditional services” and “peer staff delivering structured curricula” [ 3 ]. Other reviews suggested that current evidence does not support recommendations or mandatory requirements from policy makers to offer programs for peer support [ 9 , 10 ].
Peer Support Workers’ Satisfaction and Challenges
PSWs experience different problems alongside their diverse job roles, including low pay, stigma, unclear work roles, alienation, struggling with skill deficits, lack of training opportunities, emotional stress in helping others, and, on top of that, maintaining their personal physical and mental health wellness [ 100 , 101 ]. Researchers found that PSWs experience discrimination and prejudice from nonpeer workers, in addition to the encountered difficulties of how to manage the transition from being a patient to a PSW. As a result, high attrition rates were noted among PSWs in mental health settings [ 102 , 103 ]. Peer job satisfaction is strongly dependent on several factors [ 100 , 104 , 105 ]. Role clarity and psychological empowerment, organizational culture, and working partnership with peers were the most significant predictors of PSW job satisfaction, while professional prejudice was not perceived as a significant predictor [ 106 , 107 ]. Other studies noted that the main problems were experiencing marginalization, lack of understanding, and a sense of exclusion [ 108 - 110 ]. Payment could also contribute to the amount of satisfaction of PSWs [ 76 ], as compensation helps through facilitation and engagement motivation [ 109 ]. Nevertheless, it seems that not the payment, which ranged from US $10 to US $20 per hour, but the lack of recognition and acknowledgment are the causes for job nonsatisfaction [ 104 ].
An interesting literature review grouped these challenges and barriers facing PSWs during fulfilling their assigned roles into 6 main categories: nature of the innovation, individual professional, service user, social context, organizational context, and economic and political contexts [ 111 ].
It is evident from the abovementioned information that the PSW role is challenged at multiple levels, including at the personal, societal, and organizational levels. These challenges have a direct bearing on PSW satisfaction, and the successful integration of the PSW role into the health care system depends to a great extent on how these challenges are overcome.
Novel Technology in Peer Support Service (Online and Telephone)
Online support groups are usually conducted through bulletin boards, emails, or live chatting software [ 28 ]. Online groups are familiar with people whose illnesses are similar to SMIs or affecting the body shape that have forced them to experience embarrassment and social stigmatization [ 23 , 24 ]. Therefore, they split from the social contexts and redirect toward novel ways of help, such as PSWs and online support groups, and web-based communities provided a suitable medium for people with SMIs by following and learning from their peers on the web, which positively helped them to fight against stigma, instilling hope and gaining insight and empowerment for better health control [ 25 ]. Increasingly, social media grew as a target for individuals with SMIs, such as schizophrenia, schizoaffective disorder, or bipolar disorder, seeking advice and supporting each other [ 112 - 114 ]. For someone with SMIs, the decision to reach out and connect with others typically occurs at a time of increased instability or when facing significant life challenges [ 115 ]. In a qualitative study, popular social media, such as YouTube, appeared useful for allowing people with SMIs to feel less alone, find hope, support each other, and share personal experiences and coping strategies with day-to-day challenges of living with mental illness through listening and posting comments [ 114 ]. Mobile phone–based peer support was found to be a feasible and acceptable way to the youngsters during their pregnancy as well as in the postpartum period [ 116 ]. In addition, when coupled with frequent face-to-face meetings with PSWs and with “text for support,” it could be of high value for patients with different mental illnesses [ 117 ]. Although online peer networks actively fight against discrimination and stigma, their accessibility to diverse patients’ sectors regarding their income and ethnicity is still questionable [ 25 ].
Future of Peer Support Services
Potential new roles, such as community health workers, peer whole health coaches, peer wellness coaches, and peer navigators, have been suggested for such a workforce [ 76 ]. They are described as an “ill-defined potential new layer of professionals” [ 118 ]. Through an initiative undertaken by SAMHSA via its “Bringing Recovery Supports to Scale Technical Assistance Center Strategy,” a successful identification of abilities and critical knowledge necessarily required for PSWs who provide help and support for those recovering from mental health and substance abuse was noted [ 76 ]. At present, peer support is seen as a growing paradigm in many countries, including the United Kingdom, Canada, New Zealand, France, and the Netherlands [ 103 , 119 ]. As an evolving culture, peer support has the opportunity to forge not just mental health system change but social change as well [ 37 ]. A novel peer support system termed “Edmonton peer support system” (EPSS) is currently being tested in a randomized controlled pilot trial [ 117 ]. In this study, investigators are evaluating the effectiveness of an innovative peer support program that incorporates leadership training, mentorship, recognition, and reward systems for PSWs, coupled with automated daily supportive text messaging, which has proven effectiveness in feasibility trials involving patients with depression and alcohol use disorders [ 120 , 121 ]. Previous studies have examined the effect of PSSs in different contexts, including outpatient departments [ 122 ], emergency departments [ 53 , 54 ], community mental health clinics [ 123 , 124 ], and inpatient sites [ 125 ]. On the contrary, the EPSS study focuses on patients who have been discharged from acute care hospitals. These patients are being randomized into 1 of the 4 main groups: enrollment in a peer support system, enrollment in a peer support system plus automated daily supportive and reminder text messages, enrollment in automated daily supportive and reminder text messages alone, or treatment as usual follow-up care. The research team hypothesizes that patients who are assigned to a peer support system plus automated daily supportive and reminder text messages will show the best outcome.
Organizations may facilitate peer support through their values, actions, and oversight [ 119 ] and through a robust supervision system with available educational access, which could be the adequate path for creating a positive and risk-free environment for PSWs throughout their complex workloads [ 126 ]. On the other hand, ethics committees play essential roles in the inclusion of PSWs in applied research studies by avoiding repetition of the work of other trusted agencies and considering the ethical validity of consent procedures for peer support interventions [ 127 ].
There is an internationally growing trend to adopt PSSs within addiction and mental health services, and despite the ongoing challenges, large sections of the current literature support the inclusion of the PSWs into the mental health care workforce. The literature suggests that the benefits of PSSs impact not only the recipients of mental health services but also extend to the PSWs and the whole health care system. Although the expected benefits of PSSs might be directly measured in terms of service utilization or patient improvement indicators, this could also extend to include wellness and empowerment for PSWs, who may still be fragile, vulnerable, and in need of ongoing acknowledgment and recognition. Thus, the potential for PSSs to be embedded into routine care and the opportunities for the development of innovative models of care for addiction and mental health patients such as the EPSS, which incorporates PSSs and supportive text messaging [ 117 ], are evidently a high valued priority. However, the feasibility and maintenance of a robust PSS in health care would only be possible through collaborative efforts and ongoing support and engagement from all health care practitioners, managers, and other stakeholders.
This literature review has several limitations. First, the review is not a systematic review or meta-analysis, and as such, there were no well-defined inclusion or exclusion criteria of studies, which potentially could lead to the exclusion of some essential related studies. Second, the search was conducted in English publications only. Consequently, there is a high probability of missing critical related publications published in non-English languages. Finally, as the review depended mainly on the available literature from the aforementioned sources, which showed marked variability in their design and covered diverse ideas under the central theme, the different weights for each idea throughout the review could be noted.
Acknowledgments
This work was supported by Douglas Harding Trust Fund and Alberta Health Services.
Conflicts of Interest
None declared.
- Weiner DB. The apprenticeship of Philippe Pinel: a new document, 'observations of Citizen Pussin on the insane'. Am J Psychiatry. Sep 1979;136(9):1128-1134. [ CrossRef ] [ Medline ]
- Chinman M, George P, Dougherty RH, Daniels AS, Ghose SS, Swift A, et al. Peer support services for individuals with serious mental illnesses: assessing the evidence. Psychiatr Serv. Apr 1, 2014;65(4):429-441. [ CrossRef ] [ Medline ]
- Penney D. Advocates for Human Potential. 2018. URL: https://www.ahpnet.com/AHPNet/media/AHPNetMediaLibrary/White%20Papers/DPenney_Defining_peer_support_2018_Final.pdf [accessed 2019-03-30]
- Moran GS, Russinova Z, Gidugu V, Yim JY, Sprague C. Benefits and mechanisms of recovery among peer providers with psychiatric illnesses. Qual Health Res. Mar 2012;22(3):304-319. [ CrossRef ] [ Medline ]
- Clarke GN, Herinckx HA, Kinney RF, Paulson RI, Cutler DL, Lewis K, et al. Psychiatric hospitalizations, arrests, emergency room visits, and homelessness of clients with serious and persistent mental illness: findings from a randomized trial of two ACT programs vs. usual care. Ment Health Serv Res. Sep 2000;2(3):155-164. [ CrossRef ] [ Medline ]
- Davidson L, Shahar G, Stayner DA, Chinman MJ, Rakfeldt J, Tebes JK. Supported socialization for people with psychiatric disabilities: lessons from a randomized controlled trial. J Commun Psychol. 2004;32(4):453-477. [ CrossRef ]
- O'Donnell M, Parker G, Proberts M, Matthews R, Fisher D, Johnson B, et al. A study of client-focused case management and consumer advocacy: the Community and Consumer Service Project. Aust N Z J Psychiatry. Oct 1999;33(5):684-693. [ CrossRef ] [ Medline ]
- Solomon P, Draine J. The efficacy of a consumer case management team: 2-year outcomes of a randomized trial. J Ment Health Adm. 1995;22(2):135-146. [ CrossRef ] [ Medline ]
- Pitt V, Lowe D, Hill S, Prictor M, Hetrick SE, Ryan R, et al. Consumer-providers of care for adult clients of statutory mental health services. Cochrane Database Syst Rev. Mar 28, 2013;(3):CD004807. [ CrossRef ] [ Medline ]
- Lloyd-Evans B, Mayo-Wilson E, Harrison B, Istead H, Brown E, Pilling S, et al. A systematic review and meta-analysis of randomised controlled trials of peer support for people with severe mental illness. BMC Psychiatry. Feb 14, 2014;14:39. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Davidson L, Tondora J, Staeheli M, Martha C, Maria F, Jennifer M, et al. Recovery guides: an emerging model of community-based care for adults with psychiatric disabilities. In: Lightburn A, Sessions P, editors. Handbook Of Community-based Clinical Practice. London. Oxford University Press; 2005:476-501.
- Felton CJ, Stastny P, Shern DL, Blanch A, Donahue SA, Knight E, et al. Consumers as peer specialists on intensive case management teams: impact on client outcomes. Psychiatr Serv. Oct 1995;46(10):1037-1044. [ CrossRef ] [ Medline ]
- Beales A, Wilson J. Peer support – the what, why, who, how and now. J Ment Health Train Educ Prac. 2015;10(5):314-324. [ CrossRef ]
- MacNeil C, Mead S. A narrative approach to developing standards for trauma-informed peer support. Am J Eval. 2016;26(2):231-244. [ CrossRef ]
- Canadian Mental Health Association. Canadian Mental Health Association, BC Division; 2007. URL: https://cmha.bc.ca/wp-content/uploads/2016/07/ParentPeerSupportGuide.pdf [accessed 2020-02-29]
- Mood Disorders Association of Ontario. URL: https://www.mooddisorders.ca/family-matters-programs [accessed 2020-02-29]
- Quinn J, Barrowclough C, Tarrier N. The Family Questionnaire (FQ): a scale for measuring symptom appraisal in relatives of schizophrenic patients. Acta Psychiatr Scand. Oct 2003;108(4):290-296. [ CrossRef ] [ Medline ]
- Leggatt M, Woodhead G. Family peer support work in an early intervention youth mental health service. Early Interv Psychiatry. Oct 2016;10(5):446-451. [ CrossRef ] [ Medline ]
- Mahomed F, Stein MA, Chauhan A, Pathare S. 'They love me, but they don't understand me': Family support and stigmatisation of mental health service users in Gujarat, India. Int J Soc Psychiatry. Feb 2019;65(1):73-79. [ CrossRef ] [ Medline ]
- Davidson L, Rowe M. The Family-Run Executive Director Leadership Association (FREDLA). 5600 Fishers Ln, Rockville, MD 20857. The CMHS National GAINS Center; May 2008. URL: https://fredla.org/wp-content/uploads/2016/01/davidsonrowe_peersupport1.pdf [accessed 2020-03-01]
- Short R, Woods-Nyce K, Cross SL, Hurst MA, Gordish L, Raia J. The impact of forensic peer support specialists on risk reduction and discharge readiness in a psychiatric facility: A five-year perspective. Int J Psychosoc Rehabil. 2012;16(2):3-10. [ FREE Full text ]
- Davidson L, Bellamy C, Guy K, Miller R. Peer support among persons with severe mental illnesses: a review of evidence and experience. World Psychiatry. Jun 2012;11(2):123-128. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Berger M, Wagner TH, Baker LC. Internet use and stigmatized illness. Soc Sci Med. Oct 2005;61(8):1821-1827. [ CrossRef ] [ Medline ]
- Highton-Williamson E, Priebe S, Giacco D. Online social networking in people with psychosis: a systematic review. Int J Soc Psychiatry. Feb 2015;61(1):92-101. [ CrossRef ] [ Medline ]
- Naslund JA, Aschbrenner KA, Marsch LA, Bartels SJ. The future of mental health care: peer-to-peer support and social media. Epidemiol Psychiatr Sci. Apr 2016;25(2):113-122. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Mead S, Hilton D, Curtis L. Peer support: a theoretical perspective. Psychiatr Rehabil J. 2001;25(2):134-141. [ CrossRef ] [ Medline ]
- Mental Health Foundation. URL: https://www.mentalhealth.org.uk/a-to-z/p/peer-support [accessed 2020-02-29]
- Solomon P. Peer support/peer provided services underlying processes, benefits, and critical ingredients. Psychiatr Rehabil J. 2004;27(4):392-401. [ CrossRef ] [ Medline ]
- Davidson L, Chinman M, Sells D, Rowe M. Peer support among adults with serious mental illness: a report from the field. Schizophr Bull. Jul 2006;32(3):443-450. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Mead S. Intentional Peer Support: An Alternative Approach. West Chesterfield, NH. Intentional Peer Support; 2014.
- Sunderland K, Mishkin W, Peer Leadership Group, Mental Health Commission of Canada. Mental Health Commission of Canada. 2013. URL: https://www.mentalhealthcommission.ca/sites/default/files/peer_support_guidelines.pdf.pdf [accessed 2020-02-29]
- Peterson D. A Mad People’s History of Madness. Pittsburgh, PA. University Of Pittsburgh Press; 1981.
- Shaw C. Together: A leading UK mental health charity. 2014. URL: https://www.together-uk.org/wp-content/uploads/downloads/2014/11/Peer-Support-in-Secure-Settings-Final-Report-4-Nov-14.pdf [accessed 2020-02-28]
- Mead S. Defining Peer Support. Mar 2003. URL: http://164.156.7.185/parecovery/documents/DefiningPeerSupport_Mead.pdf [accessed 2020-02-29]
- Ostrow L, Steinwachs D, Leaf PJ, Naeger S. Medicaid reimbursement of mental health peer-run organizations: results of a national survey. Adm Policy Ment Health. Jul 2017;44(4):501-511. [ CrossRef ] [ Medline ]
- Stratford AC, Halpin M, Phillips K, Skerritt F, Beales A, Cheng V, et al. The growth of peer support: an international charter. J Ment Health. Dec 2019;28(6):627-632. [ CrossRef ] [ Medline ]
- Mead S. Google Docs. PO Box 259, West Chesterfield, NH 03466. Intentional Peer Support; 2001. URL: https://docs.google.com/document/d/1trJ35i4dXX5AIWRnbg78OaT7-RfPE9_DbPm5kSST9_Q/edit [accessed 2020-02-28]
- Wilson AM, Hutchinson M, Hurley J. Literature review of trauma-informed care: implications for mental health nurses working in acute inpatient settings in Australia. Int J Ment Health Nurs. Aug 2017;26(4):326-343. [ CrossRef ] [ Medline ]
- Goetz SB, Taylor-Trujillo A. A change in culture: violence prevention in an acute behavioral health setting. J Am Psychiatr Nurses Assoc. 2012;18(2):96-103. [ CrossRef ] [ Medline ]
- Ashmore TR. Massey University. 2013. URL: https://mro.massey.ac.nz/bitstream/handle/10179/5855/02_whole.pdf [accessed 2020-02-29]
- Brown VB, Harris M, Fallot R. Moving toward trauma-informed practice in addiction treatment: a collaborative model of agency assessment. J Psychoactive Drugs. 2013;45(5):386-393. [ CrossRef ] [ Medline ]
- Guay S, Tremblay N, Goncalves J, Bilodeau H, Geoffrion S. Effects of a peer support programme for youth social services employees experiencing potentially traumatic events: a protocol for a prospective cohort study. BMJ Open. Jun 24, 2017;7(6):e014405. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Gillard SG, Edwards C, Gibson SL, Owen K, Wright C. Introducing peer worker roles into UK mental health service teams: a qualitative analysis of the organisational benefits and challenges. BMC Health Serv Res. May 24, 2013;13:188. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Tookey P, Mason K, Broad J, Behm M, Bondy L, Powis J. From client to co-worker: a case study of the transition to peer work within a multi-disciplinary hepatitis c treatment team in Toronto, Canada. Harm Reduct J. Aug 14, 2018;15(1):41. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Stastny P, Brown C. [Peer specialist: origins, pitfalls and worldwide dissemination]. Vertex. 2013;24(112):455-459. [ Medline ]
- Simpson A, Oster C, Muir-Cochrane E. Liminality in the occupational identity of mental health peer support workers: a qualitative study. Int J Ment Health Nurs. Apr 2018;27(2):662-671. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Cabassa LJ, Camacho D, Vélez-Grau CM, Stefancic A. Peer-based health interventions for people with serious mental illness: a systematic literature review. J Psychiatr Res. Jan 2017;84:80-89. [ CrossRef ] [ Medline ]
- Chinman M, Oberman RS, Hanusa BH, Cohen AN, Salyers MP, Twamley EW, et al. A cluster randomized trial of adding peer specialists to intensive case management teams in the Veterans Health Administration. J Behav Health Serv Res. Jan 2015;42(1):109-121. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Druss BG, Zhao L, von Esenwein SA, Bona JR, Fricks L, Jenkins-Tucker S, et al. The Health and Recovery Peer (HARP) Program: a peer-led intervention to improve medical self-management for persons with serious mental illness. Schizophr Res. May 2010;118(1-3):264-270. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Chien W, Clifton AV, Zhao S, Lui S. Peer support for people with schizophrenia or other serious mental illness. Cochrane Database Syst Rev. Apr 4, 2019;4:CD010880. [ CrossRef ] [ Medline ]
- Reif S, Braude L, Lyman DR, Dougherty RH, Daniels AS, Ghose SS, et al. Peer recovery support for individuals with substance use disorders: assessing the evidence. Psychiatr Serv. Jul 2014;65(7):853-861. [ CrossRef ] [ Medline ]
- Best DW, Lubman DI. The recovery paradigm - a model of hope and change for alcohol and drug addiction. Aust Fam Physician. Aug 2012;41(8):593-597. [ Medline ]
- Watson DP, Brucker K, McGuire A, Snow-Hill NL, Xu H, Cohen A, et al. Replication of an emergency department-based recovery coaching intervention and pilot testing of pragmatic trial protocols within the context of Indiana's Opioid State Targeted Response plan. J Subst Abuse Treat. Jan 2020;108:88-94. [ CrossRef ] [ Medline ]
- McGuire AB, Powell KG, Treitler PC, Wagner KD, Smith KP, Cooperman N, et al. Emergency department-based peer support for opioid use disorder: emergent functions and forms. J Subst Abuse Treat. Jan 2020;108:82-87. [ CrossRef ] [ Medline ]
- Litt MD, Kadden RM, Kabela-Cormier E, Petry N. Changing network support for drinking: initial findings from the network support project. J Consult Clin Psychol. Aug 2007;75(4):542-555. [ CrossRef ] [ Medline ]
- Barrenger SL, Hamovitch EK, Rothman MR. Enacting lived experiences: peer specialists with criminal justice histories. Psychiatr Rehabil J. Mar 2019;42(1):9-16. [ CrossRef ] [ Medline ]
- Angell B, Matthews E, Barrenger S, Watson AC, Draine J. Engagement processes in model programs for community reentry from prison for people with serious mental illness. Int J Law Psychiatry. 2014;37(5):490-500. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Thomas K, Wilson JL, Bedell P, Morse DS. 'They didn't give up on me': a women's transitions clinic from the perspective of re-entering women. Addict Sci Clin Pract. Apr 2, 2019;14(1):12. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Kim SH. [Effects of a volunteer-run peer support program on health and satisfaction with social support of older adults living alone]. J Korean Acad Nurs. Aug 2012;42(4):525-536. [ CrossRef ] [ Medline ]
- Chapin RK, Sergeant JF, Landry S, Leedahl SN, Rachlin R, Koenig T, et al. Reclaiming joy: pilot evaluation of a mental health peer support program for older adults who receive Medicaid. Gerontologist. Apr 2013;53(2):345-352. [ CrossRef ] [ Medline ]
- Ahmed SM, Palermo AS. Community engagement in research: frameworks for education and peer review. Am J Public Health. Aug 2010;100(8):1380-1387. [ CrossRef ] [ Medline ]
- Student Minds. 2014. URL: https://www.studentminds.org.uk/uploads/3/7/8/4/3784584/grand_challenges_report_for_public.pdf [accessed 2020-02-29]
- Davies EB, Wardlaw J, Morriss R, Glazebrook C. An experimental study exploring the impact of vignette gender on the quality of university students' mental health first aid for peers with symptoms of depression. BMC Public Health. Feb 25, 2016;16:187. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Byrom N. An evaluation of a peer support intervention for student mental health. J Ment Health. Jun 2018;27(3):240-246. [ CrossRef ] [ Medline ]
- Lubman DI, Cheetham A, Jorm AF, Berridge BJ, Wilson C, Blee F, et al. Australian adolescents' beliefs and help-seeking intentions towards peers experiencing symptoms of depression and alcohol misuse. BMC Public Health. Aug 16, 2017;17(1):658. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Sokol R, Fisher E. Peer support for the hardly reached: a systematic review. Am J Public Health. Jul 2016;106(7):e1-e8. [ CrossRef ] [ Medline ]
- Fortuna KL, DiMilia PR, Lohman MC, Bruce ML, Zubritsky CD, Halaby MR, et al. Feasibility, acceptability, and preliminary effectiveness of a peer-delivered and technology supported self-management intervention for older adults with serious mental illness. Psychiatr Q. Jun 2018;89(2):293-305. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Whiteman KL, Naslund JA, DiNapoli EA, Bruce ML, Bartels SJ. Systematic review of integrated general medical and psychiatric self-management interventions for adults with serious mental illness. Psychiatr Serv. Nov 1, 2016;67(11):1213-1225. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Pathare S, Shields LS. Supported decision-making for persons with mental illness: a review. Pub Health Rev. 2012;34(15). [ CrossRef ]
- Mahomed F, Stein MA, Patel V. Involuntary mental health treatment in the era of the United Nations Convention on the Rights of Persons with Disabilities. PLoS Med. Oct 2018;15(10):e1002679. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Morrissey F. The United Nations Convention on the Rights of Persons with Disabilities: a new approach to decision-making in mental health law. Eur J Health Law. Dec 2012;19(5):423-440. [ CrossRef ] [ Medline ]
- Szmukler G. 'Capacity', 'best interests', 'will and preferences' and the UN Convention on the Rights of Persons with Disabilities. World Psychiatry. Feb 2019;18(1):34-41. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Jeste DV, Eglit GM, Palmer BW, Martinis JG, Blanck P, Saks ER. Supported decision making in serious mental illness. Psychiatry. 2018;81(1):28-40. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Craigie J. A fine balance: reconsidering patient autonomy in light of the UN convention on the rights of persons with disabilities. Bioethics. Jul 2015;29(6):398-405. [ CrossRef ] [ Medline ]
- Henderson JL, Cheung A, Cleverley K, Chaim G, Moretti ME, de Oliveira C, et al. Integrated collaborative care teams to enhance service delivery to youth with mental health and substance use challenges: protocol for a pragmatic randomised controlled trial. BMJ Open. Feb 6, 2017;7(2):e014080. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Gagne CA, Finch WL, Myrick KJ, Davis LM. Peer workers in the behavioral and integrated health workforce: opportunities and future directions. Am J Prev Med. Jun 2018;54(6 Suppl 3):S258-S266. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Smith R, Greenwood N. The impact of volunteer mentoring schemes on carers of people with dementia and volunteer mentors: a systematic review. Am J Alzheimers Dis Other Demen. Feb 2014;29(1):8-17. [ CrossRef ] [ Medline ]
- Huang L, Stroul B, Friedman R, Mrazek P, Friesen B, Pires S, et al. Transforming mental health care for children and their families. Am Psychol. Sep 2005;60(6):615-627. [ CrossRef ] [ Medline ]
- Hogan MF. The President's New Freedom Commission: recommendations to transform mental health care in America. Psychiatr Serv. Nov 2003;54(11):1467-1474. [ CrossRef ] [ Medline ]
- Singla DR, Kumbakumba E, Aboud FE. Effects of a parenting intervention to address maternal psychological wellbeing and child development and growth in rural Uganda: a community-based, cluster randomised trial. Lancet Glob Health. Aug 2015;3(8):e458-e469. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Manandhar DS, Osrin D, Shrestha BP, Mesko N, Morrison J, Tumbahangphe KM, et al. Members of the MIRA Makwanpur trial team. Effect of a participatory intervention with women's groups on birth outcomes in Nepal: cluster-randomised controlled trial. Lancet. 2004;364(9438):970-979. [ CrossRef ] [ Medline ]
- Balaji M, Andrews T, Andrew G, Patel V. The acceptability, feasibility, and effectiveness of a population-based intervention to promote youth health: an exploratory study in Goa, India. J Adolesc Health. May 2011;48(5):453-460. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Tripathy, Nair N, Barnett S, Mahapatra R, Borghi J, Rath S, et al. Effect of a participatory intervention with women's groups on birth outcomes and maternal depression in Jharkhand and Orissa, India: a cluster-randomised controlled trial. Lancet. Apr 3, 2010;375(9721):1182-1192. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Jordans MJ, Aldridge L, Luitel NP, Baingana F, Kohrt BA. Evaluation of outcomes for psychosis and epilepsy treatment delivered by primary health care workers in Nepal: a cohort study. Int J Ment Health Syst. 2017;11:70. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Kohrt B, Asher L, Bhardwaj A, Fazel M, Jordans M, Mutamba B, et al. The role of communities in mental health care in low- and middle-income countries: a meta-review of components and competencies. Int J Environ Res Public Health. Jun 16, 2018;15(6):pii: E1279. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Arnold I. Workplace Strategies for Mental Health. 2005. URL: https://www.workplacestrategiesformentalhealth.com/job-specific-strategies/peer-support-programs [accessed 2020-02-29]
- Bartels SJ, DiMilia PR, Fortuna KL, Naslund JA. Integrated care for older adults with serious mental illness and medical comorbidity: evidence-based models and future research directions. Psychiatr Clin North Am. Mar 2018;41(1):153-164. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Bates A, Kemp V, Isaac M. Peer support shows promise in helping persons living with mental illness address their physical health needs. Can J Commun Ment Health. 2008;27(2):21-36. [ CrossRef ]
- Hardy S, Hallett N, Chaplin E. Evaluating a peer support model of community wellbeing for mental health: a coproduction approach to evaluation. Ment Health Prev. 2019;13(7):149-158. [ FREE Full text ] [ CrossRef ]
- Cabassa LJ, Stefancic A, O'Hara K, El-Bassel N, Lewis-Fernández R, Luchsinger JA, et al. Peer-led healthy lifestyle program in supportive housing: study protocol for a randomized controlled trial. Trials. Sep 2, 2015;16:388. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Repper J, Carter T. A review of the literature on peer support in mental health services. J Ment Health. Aug 2011;20(4):392-411. [ CrossRef ] [ Medline ]
- Fisher EB, Coufal MM, Parada H, Robinette JB, Tang PY, Urlaub DM, et al. Peer support in health care and prevention: cultural, organizational, and dissemination issues. Annu Rev Public Health. 2014;35:363-383. [ CrossRef ] [ Medline ]
- MacLellan J, Surey J, Abubakar I, Stagg HR. Peer support workers in health: a qualitative metasynthesis of their experiences. PLoS One. 2015;10(10):e0141122. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Fisher EB, Boothroyd RI, Coufal MM, Baumann LC, Mbanya JC, Rotheram-Borus MJ, et al. Peer support for self-management of diabetes improved outcomes in international settings. Health Aff (Millwood). Jan 2012;31(1):130-139. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Singh P, Chokshi DA. Community health workers--a local solution to a global problem. N Engl J Med. Sep 5, 2013;369(10):894-896. [ CrossRef ] [ Medline ]
- Kangovi S, Long JA, Emanuel E. Community health workers combat readmission. Arch Intern Med. Dec 10, 2012;172(22):1756-1757. [ CrossRef ] [ Medline ]
- Fisher EB, Ayala GX, Ibarra L, Cherrington AL, Elder JP, Tang TS, et al. Peers for Progress Investigator Group. Contributions of peer support to health, health care, and prevention: papers from peers for progress. Ann Fam Med. Aug 2015;13(Suppl 1):S2-S8. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Tondora J, O'Connell M, Miller R, Dinzeo T, Bellamy C, Andres-Hyman R, et al. A clinical trial of peer-based culturally responsive person-centered care for psychosis for African Americans and Latinos. Clin Trials. Aug 2010;7(4):368-379. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Sweeney A, Fahmy S, Nolan F, Morant N, Fox Z, Lloyd-Evans B, et al. The relationship between therapeutic alliance and service user satisfaction in mental health inpatient wards and crisis house alternatives: a cross-sectional study. PLoS One. 2014;9(7):e100153. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Mancini MA. An exploration of factors that effect the implementation of peer support services in community mental health settings. Community Ment Health J. Feb 2018;54(2):127-137. [ CrossRef ] [ Medline ]
- Ahmed AO, Hunter KM, Mabe AP, Tucker SJ, Buckley PF. The professional experiences of peer specialists in the Georgia Mental Health Consumer Network. Community Ment Health J. May 2015;51(4):424-436. [ CrossRef ] [ Medline ]
- Walker G, Bryant W. Peer support in adult mental health services: a metasynthesis of qualitative findings. Psychiatr Rehabil J. Mar 2013;36(1):28-34. [ CrossRef ] [ Medline ]
- Villani M, Kovess-Masféty V. [Peer support programs in mental health in France: Status report and challenges]. Encephale. Nov 2018;44(5):457-464. [ CrossRef ] [ Medline ]
- Cronise R, Teixeira C, Rogers ES, Harrington S. The peer support workforce: results of a national survey. Psychiatr Rehabil J. Sep 2016;39(3):211-221. [ CrossRef ] [ Medline ]
- Corrigan PW, Kosyluk KA, Rüsch N. Reducing self-stigma by coming out proud. Am J Public Health. May 2013;103(5):794-800. [ CrossRef ] [ Medline ]
- Davis JK. Predictors of job satisfaction among peer providers on professional treatment teams in community-based agencies. Psychiatr Serv. Feb 1, 2013;64(2):181-184. [ CrossRef ] [ Medline ]
- Clossey L, Solomon P, Hu C, Gillen J, Zinn M. Predicting job satisfaction of mental health peer support workers (PSWs). Soc Work Ment Health. 2018;16(6):682-695. [ CrossRef ]
- Kemp V, Henderson AR. Challenges faced by mental health peer support workers: peer support from the peer supporter's point of view. Psychiatr Rehabil J. 2012;35(4):337-340. [ CrossRef ] [ Medline ]
- Greer AM, Amlani A, Burmeister C, Scott A, Newman C, Lampkin H, et al. Peer engagement barriers and enablers: insights from people who use drugs in British Columbia, Canada. Can J Public Health. Apr 2019;110(2):227-235. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Clossey L, Gillen J, Frankel H, Hernandez J. The experience of certified peer specialists in mental health. Soc Work Ment Health. 2015;14(4):408-427. [ CrossRef ]
- Vandewalle J, Debyser B, Beeckman D, Vandecasteele T, Van Hecke A, Verhaeghe S. Peer workers' perceptions and experiences of barriers to implementation of peer worker roles in mental health services: A literature review. Int J Nurs Stud. Aug 2016;60:234-250. [ CrossRef ] [ Medline ]
- Gowen K, Deschaine M, Gruttadara D, Markey D. Young adults with mental health conditions and social networking websites: seeking tools to build community. Psychiatr Rehabil J. 2012;35(3):245-250. [ CrossRef ] [ Medline ]
- Miller BJ, Stewart A, Schrimsher J, Peeples D, Buckley PF. How connected are people with schizophrenia? Cell phone, computer, email, and social media use. Psychiatry Res. Feb 28, 2015;225(3):458-463. [ CrossRef ] [ Medline ]
- Naslund JA, Grande SW, Aschbrenner KA, Elwyn G. Naturally occurring peer support through social media: the experiences of individuals with severe mental illness using YouTube. PLoS One. 2014;9(10):e110171. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Perry BL, Pescosolido BA. Social network activation: the role of health discussion partners in recovery from mental illness. Soc Sci Med. Jan 2015;125:116-128. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Chyzzy B, Dennis C. 16. Mobile phone-based peer support in the prevention of postpartum depression among adolescent mothers: a pilot randomized controlled trial. J Adolesc Health. 2019;64(2):S8-S9. [ CrossRef ]
- Urichuk L, Hrabok M, Hay K, Spurvey P, Sosdjan D, Knox M, et al. Enhancing peer support experience for patients discharged from acute psychiatric care: protocol for a randomised controlled pilot trial. BMJ Open. Aug 17, 2018;8(8):e022433. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Hurley J, Cashin A, Mills J, Hutchinson M, Graham I. A critical discussion of Peer Workers: implications for the mental health nursing workforce. J Psychiatr Ment Health Nurs. Mar 2016;23(2):129-135. [ CrossRef ] [ Medline ]
- Burke EM, Pyle M, Machin K, Morrison AP. Providing mental health peer support 1: A Delphi study to develop consensus on the essential components, costs, benefits, barriers and facilitators. Int J Soc Psychiatry. 2018;64(8):799-812. [ CrossRef ]
- Agyapong VI, Juhás M, Mrklas K, Hrabok M, Omeje J, Gladue I, et al. Randomized controlled pilot trial of supportive text messaging for alcohol use disorder patients. J Subst Abuse Treat. Nov 2018;94:74-80. [ CrossRef ] [ Medline ]
- Agyapong VI, Ahern S, McLoughlin DM, Farren CK. Supportive text messaging for depression and comorbid alcohol use disorder: single-blind randomised trial. J Affect Disord. Dec 10, 2012;141(2-3):168-176. [ CrossRef ] [ Medline ]
- Gill K. New Moves: Targeting physical and mental illness well-being in people with mental illness. Health Issues J. 2012;108(1):18-23. [ FREE Full text ] [ CrossRef ]
- Martin M, Martin SL. Healthy Amistad: improving the health of people with severe mental illness. Issues Ment Health Nurs. Oct 2014;35(10):791-795. [ CrossRef ] [ Medline ]
- Lorig K, Ritter PL, Pifer C, Werner P. Effectiveness of the chronic disease self-management program for persons with a serious mental illness: a translation study. Community Ment Health J. Jan 2014;50(1):96-103. [ CrossRef ] [ Medline ]
- Bouchard L, Montreuil M, Gros C. Peer support among inpatients in an adult mental health setting. Issues Ment Health Nurs. Sep 2010;31(9):589-598. [ CrossRef ] [ Medline ]
- Hurley J, Cashin A, Mills J, Hutchinson M, Kozlowski D, Graham I. Qualitative study of peer workers within the 'Partners in Recovery' programme in regional Australia. Int J Ment Health Nurs. Feb 2018;27(1):187-195. [ CrossRef ] [ Medline ]
- Simmons D, Bunn C, Nakwagala F, Safford MM, Ayala GX, Riddell M, et al. Challenges in the ethical review of peer support interventions. Ann Fam Med. Aug 2015;13(Suppl 1):S79-S86. [ FREE Full text ] [ CrossRef ] [ Medline ]
Abbreviations
| Convention on the Rights of Persons with Disabilities |
| Edmonton peer support system |
| intentional peer support |
| peer support service |
| peer support worker |
| people with disability |
| quality of life |
| randomized controlled trial |
| Substance Abuse and Mental Health Services Administration |
| serious mental illness |
| trauma-informed care |
Edited by J Torous; submitted 21.07.19; peer-reviewed by F Mahomed, K Machin; comments to author 27.07.19; revised version received 06.09.19; accepted 15.02.20; published 09.06.20.
©Reham A Hameed Shalaby, Vincent I O Agyapong. Originally published in JMIR Mental Health (http://mental.jmir.org), 09.06.2020.
This is an open-access article distributed under the terms of the Creative Commons Attribution License (https://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work, first published in JMIR Mental Health, is properly cited. The complete bibliographic information, a link to the original publication on http://mental.jmir.org/, as well as this copyright and license information must be included.
Peer Support and Mental Health: A Review of the Evidence
- First Online: 12 April 2023
Cite this chapter

- Megan Evans 2
432 Accesses
1 Citations
Despite the proliferation of peer support services in practice, the evidence base lags and is largely inconclusive regarding effectiveness. This is likely due, at least in part, to continued confusion and lack of clarity around the definition of peer support services. Additionally, significant variability in peer programs, participants, and outcomes measured further complicates evidence synthesis. This chapter highlights findings from several important systematic reviews of peer support for mental health. Thus far, the literature suggests that peer support services might be unique in their ability to instill hope through positive self-disclosure and use experiential knowledge. Additionally, peers’ lived experience often means that they are better positioned to address concrete concerns of living, such as housing, transportation, finances, and navigating social services programs. They may act as advocates and encourage self-advocacy among those they support. While peer support has been widely studied in chronic disease care and mental health, far less research has focused on peer support specifically for people with schizophrenia or related psychoses. Reflecting research in the field more broadly, studies of peer support reaching people with schizophrenia are diverse. More research is needed to understand what works, for whom, and in what circumstances.
This is a preview of subscription content, log in via an institution to check access.
Access this chapter
Subscribe and save.
- Get 10 units per month
- Download Article/Chapter or eBook
- 1 Unit = 1 Article or 1 Chapter
- Cancel anytime
- Available as PDF
- Read on any device
- Instant download
- Own it forever
- Available as EPUB and PDF
- Compact, lightweight edition
- Dispatched in 3 to 5 business days
- Free shipping worldwide - see info
- Durable hardcover edition
Tax calculation will be finalised at checkout
Purchases are for personal use only
Institutional subscriptions
Gillard S. Peer support in mental health services: where is the research taking us, and do we want to go there? Taylor & Francis; 2019. p. 341–4.
Google Scholar
Davidson L. Peer support: coming of age of and/or miles to go before we sleep? An introduction. J Behav Health Serv Res. 2015;42(1):96–9.
Article PubMed PubMed Central Google Scholar
Bellamy C, Schmutte T, Davidson L. An update on the growing evidence base for peer support. Ment Health Soc Incl. 2017;21(3):161–7.
Article Google Scholar
White S, Foster R, Marks J, Morshead R, Goldsmith L, Barlow S, et al. The effectiveness of one-to-one peer support in mental health services: a systematic review and meta-analysis. BMC Psychiatry. 2020;20(1):1–20.
Lloyd-Evans B, Mayo-Wilson E, Harrison B, Istead H, Brown E, Pilling S, et al. A systematic review and meta-analysis of randomised controlled trials of peer support for people with severe mental illness. BMC Psychiatry. 2014;14(1):39.
Salzer MS, Schwenk E, Brusilovskiy E. Certified peer specialist roles and activities: results from a national survey. Psychiatr Serv. 2010;61(5):520–3.
Article PubMed Google Scholar
Daniels AS, Bergeson S, Fricks L, Ashenden P, Powell I. Pillars of peer support: advancing the role of peer support specialists in promoting recovery. J Ment Health Train Educ Pract. 2012;7(2):60–9.
Evans M, Barker H, Peddireddy S, Zhang A, Luu S, Qian Y, et al. Peer-delivered services and peer support reaching people with schizophrenia: a scoping review. Int J Ment Health. 2021:1–23. https://doi.org/10.1080/00207411.2021.1975441 .
Barbic S, Krupa T, Armstrong I. A randomized controlled trial of the effectiveness of a modified recovery workbook program: preliminary findings. Psychiatr Serv. 2009;60(4):491–7.
Cook JA, Copeland ME, Jonikas JA, Hamilton MM, Razzano LA, Grey DD, et al. Results of a randomized controlled trial of mental illness self-management using Wellness Recovery Action Planning. Schizophr Bull. 2011;38(4):881–91.
Chinman M, Oberman RS, Hanusa BH, Cohen AN, Salyers MP, Twamley EW, et al. A cluster randomized trial of adding peer specialists to intensive case management teams in the Veterans Health Administration. J Behav Health Serv Res. 2013;42(1):109–21.
Clarke GN, Herinckx HA, Kinney RF, Paulson RI, Cutler DL, Lewis K, et al. Psychiatric hospitalizations, arrests, emergency room visits, and homelessness of clients with serious and persistent mental illness: findings from a randomized trial of two ACT programs vs. usual care. Ment Health Serv Res. 2000;2(3):155–64.
Craig T, Doherty I, Jamieson-Craig R, Boocock A, Attafua G. The consumer-employee as a member of a Mental Health Assertive Outreach Team. I. Clinical and social outcomes. J Ment Health. 2004;13(1):59–69.
Kaplan K, Salzer MS, Solomon P, Brusilovskiy E, Cousounis P. Internet peer support for individuals with psychiatric disabilities: a randomized controlled trial. Soc Sci Med. 2011;72(1):54–62.
Proudfoot J, Parker G, Manicavasagar V, Hadzi-Pavlovic D, Whitton A, Nicholas J, et al. Effects of adjunctive peer support on perceptions of illness control and understanding in an online psychoeducation program for bipolar disorder: a randomised controlled trial. J Affect Disord. 2012;142(1–3):98–105.
Davidson L, Shahar G, Stayner DA, Chinman MJ, Rakfeldt J, Tebes JK. Supported socialization for people with psychiatric disabilities: lessons from a randomized controlled trial. J Community Psychol. 2004;32(4):453–77.
Pitt V, Lowe D, Hill S, Prictor M, Hetrick SE, Ryan R, et al. Consumer-providers of care for adult clients of statutory mental health services. Cochrane Database Syst Rev. 2013;2013(3):CD004807.
PubMed PubMed Central Google Scholar
Fuhr DC, Salisbury TT, De Silva MJ, Atif N, van Ginneken N, Rahman A, et al. Effectiveness of peer-delivered interventions for severe mental illness and depression on clinical and psychosocial outcomes: a systematic review and meta-analysis. Soc Psychiatry Psychiatr Epidemiol. 2014;49(11):1691–702.
Chinman M, George P, Dougherty RH, Daniels AS, Ghose SS, Swift A, et al. Peer support services for individuals with serious mental illnesses: assessing the evidence. Psychiatr Serv. 2014;65(4):429–41. https://doi.org/10.1176/appi.ps.201300244 .
Fisher EB, Boothroyd RI, Elstad EA, Hays L, Henes A, Maslow GR, et al. Peer support of complex health behaviors in prevention and disease management with special reference to diabetes: systematic reviews. Clin Diabetes Endocrinol. 2017;3(1):4.
Landers GM, Zhou M. An analysis of relationships among peer support, psychiatric hospitalization, and crisis stabilization. Community Ment Health J. 2011;47(1):106–12.
Sells D, Davidson L, Jewell C, Falzer P, Rowe M. The treatment relationship in peer-based and regular case management for clients with severe mental illness. Psychiatr Serv. 2006;57(8):1179–84.
Jones N, Corrigan PW, James D, Parker J, Larson N. Peer support, self-determination, and treatment engagement: a qualitative investigation. Psychiatr Rehabil J. 2013;36(3):209.
Gidugu V, Rogers ES, Harrington S, Maru M, Johnson G, Cohee J, et al. Individual peer support: a qualitative study of mechanisms of its effectiveness. Community Ment Health J. 2015;51(4):445–52.
Davidson L, Bellamy C, Guy K, Miller R. Peer support among persons with severe mental illnesses: a review of evidence and experience. World Psychiatry. 2012;11(2):123–8.
Festinger L. A theory of social comparison processes. Hum Relat. 1954;7(2):117–40.
Bandura A. Social learning theory. Englewood Cliffs: Prentice Hall; 1977.
Bandura A. Self-efficacy: the exercise of control. New York: W.H. Freeman; 1997.
Dixon LB, Dickerson F, Bellack AS, Bennett M, Dickinson D, Goldberg RW, et al. The 2009 schizophrenia PORT psychosocial treatment recommendations and summary statements. Schizophr Bull. 2009;36(1):48–70.
Chien WT, Clifton AV, Zhao S, Lui S. Peer support for people with schizophrenia or other serious mental illness. Cochrane Database Syst Rev. 2019;2019(4):CD010880.
PubMed Central Google Scholar
Chien W-T, Norman I. The effectiveness and active ingredients of mutual support groups for family caregivers of people with psychotic disorders: a literature review. Int J Nurs Stud. 2009;46(12):1604–23.
Chien W-T, Thompson DR, Norman I. Evaluation of a peer-led mutual support group for Chinese families of people with schizophrenia. Am J Community Psychol. 2008;42(1–2):122–34.
Chien WT. Effectiveness of psychoeducation and mutual support group program for family caregivers of chinese people with schizophrenia. Open Nurs J. 2008;2:28.
Chien WT, Thompson DR. An RCT with three-year follow-up of peer support groups for Chinese families of persons with schizophrenia. Psychiatr Serv. 2013;64(10):997–1005.
Castelein S, Mulder PJ, Bruggeman R. Guided peer support groups for schizophrenia: a nursing intervention. Psychiatr Serv. 2008;59(3):326.
Castelein S, Bruggeman R, Van Busschbach JT, Van Der Gaag M, Stant A, Knegtering H, et al. The effectiveness of peer support groups in psychosis: a randomized controlled trial. Acta Psychiatr Scand. 2008;118(1):64–72.
Boardman G, McCann T, Kerr D. A peer support programme for enhancing adherence to oral antipsychotic medication in consumers with schizophrenia. J Adv Nurs. 2014;70(10):2293–302.
Rummel-Kluge C, Stiegler-Kotzor M, Schwarz C, Hansen W-P, Kissling W. Peer-counseling in schizophrenia: patients consult patients. Patient Educ Couns. 2008;70(3):357–62.
Dixon LB, Holoshitz Y, Nossel I. Treatment engagement of individuals experiencing mental illness: review and update. World Psychiatry. 2016;15(1):13–20.
Pawson R, Greenhalgh T, Harvey G, Walshe K. Realist review-a new method of systematic review designed for complex policy interventions. J Health Serv Res Policy. 2005;10(1_suppl):21–34.
Rycroft-Malone J, McCormack B, Hutchinson AM, DeCorby K, Bucknall TK, Kent B, et al. Realist synthesis: illustrating the method for implementation research. Implement Sci. 2012;7(1):33.
Jagosh J. Realist synthesis for public health: building an ontologically deep understanding of how programs work, for whom, and in which contexts. Annu Rev Public Health. 2019;40:361.
Rogers ES, Swarbrick M. Peer-delivered services: current trends and innovations. Psychiatr Rehabil J. 2016;39(3):193–6.
Gillard S, Gibson S, Holley J, Lucock M. Developing a change model for peer worker interventions in mental health services: a qualitative research study. Epidemiol Psychiatr Sci. 2015;24(5):435–45.
Download references
Author information
Authors and affiliations.
Department of Psychiatry, Yale University, New Haven, CT, USA
Megan Evans
You can also search for this author in PubMed Google Scholar
Rights and permissions
Reprints and permissions
Copyright information
© 2023 The Author(s), under exclusive license to Springer Nature Switzerland AG
About this chapter
Evans, M. (2023). Peer Support and Mental Health: A Review of the Evidence. In: Peer Support Services Reaching People with Schizophrenia. Springer, Cham. https://doi.org/10.1007/978-3-031-29042-8_5
Download citation
DOI : https://doi.org/10.1007/978-3-031-29042-8_5
Published : 12 April 2023
Publisher Name : Springer, Cham
Print ISBN : 978-3-031-29041-1
Online ISBN : 978-3-031-29042-8
eBook Packages : Behavioral Science and Psychology Behavioral Science and Psychology (R0)

Share this chapter
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Publish with us
Policies and ethics
- Find a journal
- Track your research
The Effectiveness of Peer Support in Personal and Clinical Recovery: Systematic Review and Meta-Analysis
Information & authors, metrics & citations, view options, conclusions:, search strategy and selection criteria, inclusion criteria, participants., intervention., comparison., study design, exclusion criteria, bias risk assessment, data extraction, statistical analysis, systematic review, study characteristics., participants and organization., interventions., control conditions, risk for bias.
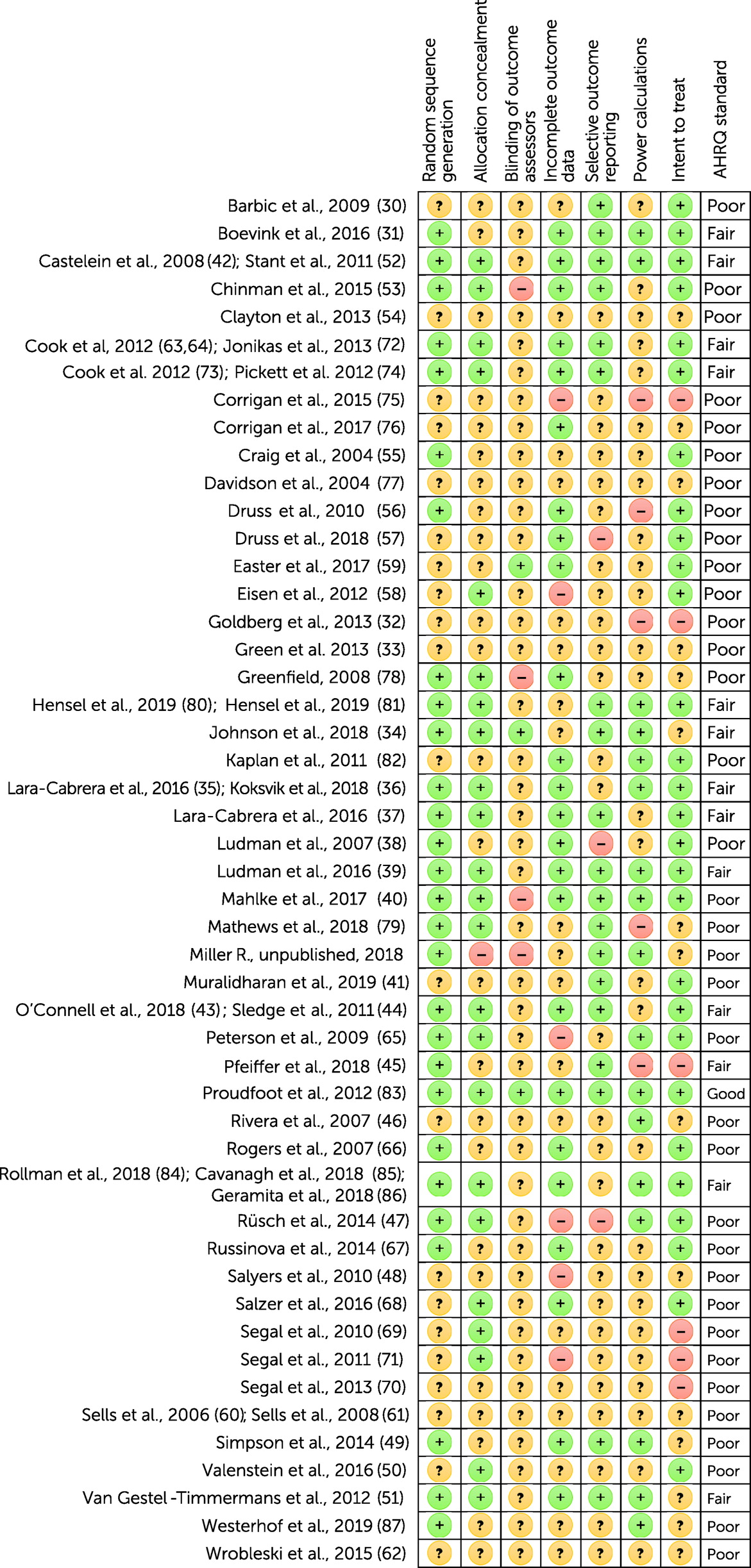
Meta-Analysis
Peer support in general., peers added to hospital services., peers in established service roles., peers independent of hospital services., peers online., heterogeneity, publication bias, post hoc analysis, main findings, comparison with earlier review findings, peer support setting and approach, peer support provider and type, strengths and limitations, conclusions, supplementary material.
- View/Download
Information
Published in.
- Peer support
- Systematic review
- Meta-analysis
- Personal recovery
- Clinical recovery
- Organizational setting
Competing Interests
Export citations.
If you have the appropriate software installed, you can download article citation data to the citation manager of your choice. Simply select your manager software from the list below and click Download. For more information or tips please see 'Downloading to a citation manager' in the Help menu .
| Format | |
|---|---|
| Citation style | |
| Style | |
To download the citation to this article, select your reference manager software.
There are no citations for this item
View options
Login options.
Already a subscriber? Access your subscription through your login credentials or your institution for full access to this article.
Purchase Options
Purchase this article to access the full text.
PPV Articles - Psychiatric Services
Not a subscriber?
Subscribe Now / Learn More
PsychiatryOnline subscription options offer access to the DSM-5-TR ® library, books, journals, CME, and patient resources. This all-in-one virtual library provides psychiatrists and mental health professionals with key resources for diagnosis, treatment, research, and professional development.
Need more help? PsychiatryOnline Customer Service may be reached by emailing [email protected] or by calling 800-368-5777 (in the U.S.) or 703-907-7322 (outside the U.S.).
Share article link
Copying failed.
PREVIOUS ARTICLE
Next article, request username.
Can't sign in? Forgot your username? Enter your email address below and we will send you your username
If the address matches an existing account you will receive an email with instructions to retrieve your username
Create a new account
Change password, password changed successfully.
Your password has been changed
Reset password
Can't sign in? Forgot your password?
Enter your email address below and we will send you the reset instructions
If the address matches an existing account you will receive an email with instructions to reset your password.
Your Phone has been verified
As described within the American Psychiatric Association (APA)'s Privacy Policy and Terms of Use , this website utilizes cookies, including for the purpose of offering an optimal online experience and services tailored to your preferences. Please read the entire Privacy Policy and Terms of Use. By closing this message, browsing this website, continuing the navigation, or otherwise continuing to use the APA's websites, you confirm that you understand and accept the terms of the Privacy Policy and Terms of Use, including the utilization of cookies.
- Research article
- Open access
- Published: 11 November 2020
The effectiveness of one-to-one peer support in mental health services: a systematic review and meta-analysis
- Sarah White 1 ,
- Rhiannon Foster 1 ,
- Jacqueline Marks 1 ,
- Rosaleen Morshead 1 ,
- Lucy Goldsmith 1 ,
- Sally Barlow 2 ,
- Jacqueline Sin 1 &
- Steve Gillard ORCID: orcid.org/0000-0002-9686-2232 1
BMC Psychiatry volume 20 , Article number: 534 ( 2020 ) Cite this article
38k Accesses
135 Citations
26 Altmetric
Metrics details
Peer support is being introduced into mental health services internationally, often in response to workforce policy. Earlier systematic reviews incorporate different modalities of peer support (i.e. group and one-to-one), offer inconsistent evidence of effectiveness, and also indicate substantial heterogeneity and issues of quality in the evidence base at that time. An updated review, focussed on one-to-one peer support, is timely given current policy interest. This study aims to systematically review evidence for the effectiveness of one-to-one peer support interventions for adults using mental health services, and to explore heterogeneity in peer support interventions.
We searched MEDLINE, PsycINFO, Embase, CINAHL and Cochrane databases from inception until 13 June 2019. Included studies were assessed for risk of bias, and meta-analyses conducted where multiple trials provided usable data.
Twenty-three studies reporting nineteen trials were eligible, providing data from 3329 participants. While seven trials were of low to moderate risk of bias, incomplete reporting of data in many studies suggested bias in the evidence base. Peer support interventions included peer workers in paraclinical roles (e.g. case manager), providing structured behavioural interventions, or more flexible support for recovery.
Meta-analyses were conducted for eleven outcomes, with evidence that one-to-one peer support may have a modest positive impact on self-reported recovery and empowerment. There was no impact on clinical symptoms or service use. Analyses of heterogeneity suggest that peer support might improve social network support.
Conclusions
One-to-one peer support in mental health services might impact positively on psychosocial outcomes, but is unlikely to improve clinical outcomes. In order to better inform the introduction of peer support into mental health services, improvement of the evidence base requires complete reporting of outcome data, selection of outcomes that relate to intervention mechanisms, exploration of heterogeneity in the implementation of peer support and focused reviews of specific types of one-to-one peer support.
Trial registration
Prospero identifier: CRD42015025621 .
Peer Review reports
Mental health and workforce policies in a number of countries advocate the introduction of large numbers of peer workers into mental health services [ 1 , 2 ]. In this context, peer workers are people with personal experience of using mental health services and/ or of mental distress, employed to make use of that experience in providing support to others currently using mental health services. Peer support more generally refers to a mutual exchange of emotional and practical support between people who identify as peers on the basis of shared or similar experiences of mental distress, with the recent origins of organised forms of peer support often ascribed to the mutual aid movement [ 3 , 4 ]. The emergence of trained peer workers, providing peer support to people using mental health services, is a comparatively newer phenomenon, stimulated perhaps in part by assumptions about economic prudence [ 5 ], and in part by suggestions that peer support aids individual recovery [ 6 ]. Peer workers have been employed in a range of roles, providing one-to-one support to individuals using mental health services, as we explore below, supporting and facilitating mutual support groups, or running services provided as an alternative to mainstream provision.
The peer support literature has been reviewed before, with Pitt and colleagues [ 7 ] finding a small reduction in emergency service use where peer workers were compared with other mental health professionals working in similar roles (primarily case management), while Lloyd Evans and team [ 8 ] found a modest positive effect of peer-provided interventions on self-reported recovery and hope. However, both reviews combined studies of individual and group-based peer support – noting substantial heterogeneity in both intervention and trial population – and in both reviews authors cautioned that the majority of trials were of low to moderate quality and that reporting bias in particular might explain these results. More focused reviews have considered peer support for people experiencing depression [ 9 ], and for those experiencing psychosis [ 10 ]. The former considered only group interventions, while the latter combined group, one-to-one and service-level modalities of peer support, and found no evidence of effectiveness of one-to-one peer support. However, a recent, informal review has indicated that a number of new trials of one-to-one peer support in mental health services have been reported [ 11 ], offering a timely opportunity for a systematic review focusing on one-to-one peer support in order to provide an evidence base for the ongoing introduction of peer workers into mental health services internationally.
Exploring heterogeneity of peer support interventions
We note that Pitt and colleagues [ 7 ] identified small differences in effect when considering ‘consumer provider [peer] vs professional staff’ in comparison to ‘consumer provider as an adjunct vs usual care alone’, warranting exploration of this aspect of intervention heterogeneity in the context of one-to-one peer support in this review. Both Pitt [ 7 ] and Lloyd Evans [ 8 ] also note that peer support is often under specified in trial papers, and that it is not always clear how peer support is different from mental health support provided by other types of mental health worker. A wider literature has identified a values-base that specifies how peer support is distinctive from other mental health support, suggesting that peer support is characterised by: a relationship grounded in a sense of connection based on shared experiences [ 12 ]; the use of experiential, rather than formal (taught) knowledge in the peer worker role [ 13 ]; the reciprocal nature of the relationship, with both parties learning from each other in contrast to the uni-directional clinician-patient relationship [ 14 ]. However, it is also noted how the formal, health services environment is not always conducive to the delivery of peer support [ 15 , 16 ].
Studies have identified a number of organisational factors that facilitate the implementation of distinctive peer support into practice, including: a clear, shared understanding of the values informing peer support in the peer worker role [ 17 ]; the importance of dedicated peer support training programmes for peer workers [ 18 ]; the need for support and supervision for peer workers [ 19 ]. Some actors in the peer support community have called for standards in the delivery of peer support in mental health services to ensure that a distinctive, values-based peer support is delivered [ 20 ]. Currently there is a lack of evidence of any association between outcomes and organisational variables supporting the delivery of peer support. There is therefore a case for exploring whether it is possible to operationalise, as a subgroup analysis, the quality of organisational support for one-to-one peer support interventions as an additional approach to exploring the heterogeneity of peer support in mental health services.
This study aims to:
systematically review all the available peer-reviewed evidence for one-to-one peer support interventions for adults using mental health services
evaluate the effects of one-to-one peer support in mental health services on a range of pre-specified outcomes
investigate, using subgroup analyses, how heterogeneity in intervention (i.e. type of peer support, quality of organisational support for peer support) is related to outcome.
This systematic review and meta-analysis adheres to PRISMA guidelines and is funded by the UK National Institute for Health Research as part of larger programme of research investigating peer support in mental health services. The review protocol is registered with the International Prospective Register Of Systematic Reviews, identifier: CRD42015025621.
Definitions
For the purpose of this review we consider one-to-one peer support in mental health services to be support delivered by an individual with personal experiences of using mental health services and/or of mental distress. We refer to the person delivering peer support here as a peer worker , noting that other terms, including peer support worker , peer specialist and consumer employee , have been used elsewhere. Peer workers are employed – whether paid or unpaid – and trained to make use of their experiential knowledge in providing support to someone who shares similar experiences, as part of or alongside the care and treatment they are receiving from mental health services.
Eligibility criteria
Studies were included where peer support was:
provided one-to-one;
intentionally provided by a peer worker;
for adults using mental health services.
Studies were excluded if peer support was:
not the primary means of delivering the intervention;
not one-to-one or intentionally provided by a peer worker;
where mental health was not the primary focus of the intervention.
Other exclusions were applied if the study was not in the English language, non-retrievable, or did not contain empirical data.
Study design
All types of randomised controlled trial (RCT) were included. Other study types were excluded.
Intervention and comparison conditions
We noted above that one-to-one peer support in mental health services has been characterised as either: an adjunctive intervention, delivered by peer workers in addition to care as usual or as an additional component to a treatment or therapy; or as peer workers delivering similar interventions to those delivered by other mental health workers (e.g. where peer workers are employed in a substitute capacity) [ 7 ]. We include both ‘adjunctive’ and ‘substitute’ peer support interventions in this review, and consider all comparator conditions in our primary analysis. Where trials had two or more intervention arms (e.g. with and without peer support) and a control arm, in all cases the comparison chosen was peer support (as intervention condition) and the other enhanced or active condition (as control condition), rather than care as usual or an attention control arm.
As noted above, a variety of outcomes have been assessed in peer support trials. Given that a number of additional trials have emerged since the publication of existing systematic reviews, it is of interest to consider whether the range of outcomes of interest remains broad or has begun to coalesce. We extract data using the set of outcomes explored in the review conducted by Lloyd-Evans and colleagues [ 8 ]. In addition, we consider use of emergency services in order to explore further findings in the Pitt review [ 7 ] and, following other published research into the mechanisms of peer support we include a small number of more socially-focused outcomes that may be impacted by peer support [ 21 ]. The full set of outcomes of interest for this review is as follows:
Hospitalisation
Emergency service use
Overall psychiatric symptoms
Symptoms of psychosis
Depression and anxiety
Quality of Life
Recovery (self-rated)
Empowerment
Satisfaction with services.
Social functioning
Social network support
Working alliance (clinician rated/ patient rated)
Self-stigma
Experienced stigma
Engagement with services
Search methods for identification of studies
The following online bibliographic databases were identified in 2015 based on then existing reviews [ 6 , 7 ] – Cochrane Central Register of Controlled Trials, MEDLINE, EMBASE, PsychINFO and CINAHL Plus – and searched initially from inception until the end of April 2015.
Existing reviews were used to provide a basis for search terms, with authors using their knowledge of the area, including service user researchers JM and RF, to add to search terms. The diagnostic manual DSM 5 [ 22 ] was consulted to provide a systematic structure to ensure mental health terms were inclusive. The search strategy was tested and refined as necessary. All databases were searched using a similar set of terms, strategies and Boolean operators, amended solely for the purposes of the research database management interface and not for content. An example of the search strategy, for MEDLINE, EMBASE and PsychINFO using the OVID interface, is given in Supplementary materials 1 .
Searches were updated on 13 June 2019, with no changes to search terms or search strategy. All papers returned by the search were imported into an Endnote library and any duplicates removed first using the software and then by manual review.
Study selection
Titles and abstracts of all studies returned in the search were independently screened for inclusion in the review by two researchers (two of JM, RF and RM). Disagreements were resolved by discussion using the full text of the paper, with remaining differences resolved by discussion with SG. Reference list and forward citation searching of included studies were used to identify additional papers for inclusion in the review.
Data extraction
Data were extracted for study characteristics from each included study by one of JM, RF or RM using a structured data extraction data sheet (see Table 1 below), with a second researcher (SG) checking for accuracy of extraction for 25% of studies.
For the purposes of exploring heterogeneity of intervention as subgroup analyses in the meta-analysis we also recorded where peer support was provided as an adjunctive intervention and where peer workers were working in a substitute role, as defined above, and in addition rated the quality of organisational support provided for peer support. To do this, studies were independently coded by two members of the team (JM and RM) where they reported any of the following indicators:
Dedicated peer support training;
Clear description of theory, processes or understanding of peer support;
Support structures for peer workers (e.g. supervision).
Discrepancies between researchers were discussed until agreement was reached. Studies were then categorised as having a ‘higher level’ of organisational support for peer support if they fulfilled at least two of the three indicators, or ‘lower level’ if they met one or less indicators.
Extraction of data for meta-analysis
One researcher (RM) extracted data for outcomes onto a bespoke extraction sheet. Data were included if they were assessed using a standardised measure or, in the case of service use data, captured in clinical records. For continuous outcomes, sample sizes, mean and standard deviations by arm were extracted, and for dichotomous outcomes, the number of events and sample size per arm were extracted. All outcome data extraction was checked by statistician SW for accuracy and completeness. If data for a particular outcome were only reported by a single paper that outcome was not included in the meta-analysis. We wrote to authors of included studies for additional information and trial data where it was not included in the published article.
Where outcome data were reported for more than one follow-up point, the longest timepoint was used. Where more than one measure was used to report the same outcome in a study, we included the measure more commonly reported by other studies in the analysis.
Assessment of risk of bias
Each included study was assessed for risk of bias by two researchers (RM, JM), with any differences in assessment resolved by a third researcher (SW), in accordance with Cochrane Collaboration Risk of Bias Tool [ 80 ]:
adequate sequence generation (selection bias)
allocation concealment (selection bias)
blinding of outcome assessment (detection bias)
incomplete outcome data (attrition bias)
selective outcome reporting (reporting bias)
It is important to note that although blinding of participants to allocation is usually assessed, in this particular instance the nature of a peer intervention means that all trial participants are unblinded. As such this particular source of bias is not assessed in this review, in line with existing reviews of peer support.
Statistical analysis
Effect sizes for continuous data were calculated as standardised mean difference (SMD), Hedges’ g, with studies weighted using the inverse variance method [ 81 ]. Risk ratios were calculated for dichotomous outcomes, and studies combined again using the inverse variance method. All pooled effect sizes are reported with 95% confidence intervals calculated using random-effects models. We used intention to treat data in all analyses.
Statistical heterogeneity was assessed through the I 2 statistic which describes the percentage of the variability in effect estimates that is due to heterogeneity rather than chance and the p -value of the χ 2 test (Q) for heterogeneity. A p-value < 0.10 and an I 2 > 50% suggests substantial heterogeneity. Where substantial heterogeneity of effect sizes across trials is observed, subgroup analyses were conducted, comparing studies where:
peer support was provided as an adjunctive intervention, against those studies where peer workers were working in a substitute role;
a higher level of organisational support for peer support were reported, against those studies where a lower level was reported.
Differences between subgroups of studies were tested using the Qint test for heterogeneity, testing if effect sizes differ across subgroups. Review Manager (RevMan 5.2 for Windows) software [ 82 ] was used to conduct the meta-analyses.
A total of 6502 records were identified in the updated search. Of these, 311 studies were potentially eligible and, after further review (as described above) 23 eligible papers were identified, reporting on 19 trials. One trial was reported across four papers [ 23 , 83 , 84 , 85 ] and another trial reported across two papers [ 45 , 86 ]. See Fig. 1 below.
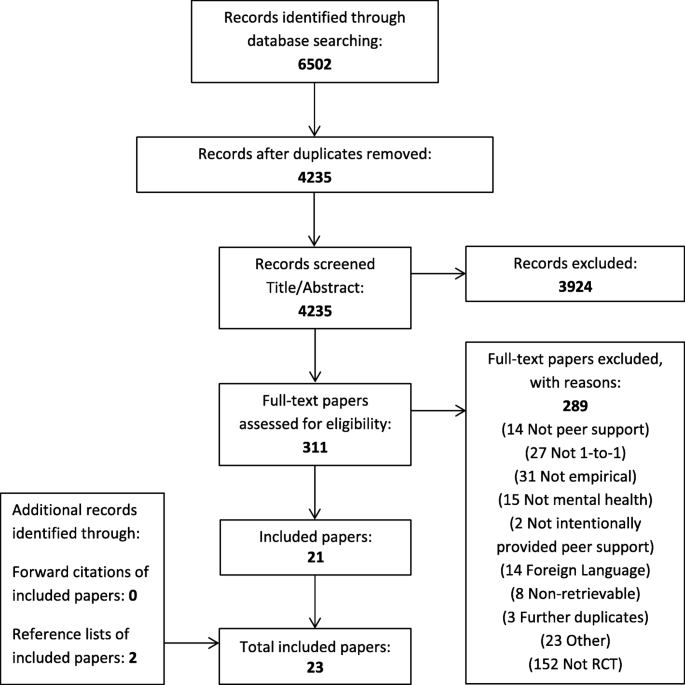
Flowchart of inclusion of studies
Study characteristics
Twelve studies were conducted in the USA [ 23 , 28 , 30 , 31 , 39 , 42 , 44 , 45 , 54 , 63 , 66 , 68 ], three were conducted in the UK [ 35 , 59 , 76 ], one in Canada [ 62 ], one in Australia [ 50 ], one in Germany [ 71 ], and one in Japan [ 74 ]. Eighteen trials were individually randomised and one was a cluster randomised trial [ 54 ]. Six studies described themselves as pilot trials [ 28 , 35 , 45 , 59 , 62 , 68 ], four studies were three-arm trials [ 30 , 31 , 42 , 50 ], and one study used a waitlist control [ 68 ].
Fifteen studies fell into the ‘adjunctive’ peer support group, with eleven of those comparing peer support as an adjunctive intervention to care as usual [ 28 , 31 , 35 , 42 , 45 , 54 , 59 , 66 , 71 , 74 , 76 ]. Two of the eleven [ 31 , 42 ] were three arm trials comparing care as usual, an adjunctive intervention, and the intervention plus an additional peer support component. Another three-arm trial [ 50 ] compared an attention control, intervention, and the intervention plus an additional peer support component. Two papers reported two arm trials of an intervention, with and without adjunctive peer support [ 44 , 63 ], and one study compared the peer support intervention with a waitlist condition (i.e. no-comparator intervention) [ 68 ]. Four studies compared peer workers working in a substitute capacity compared with other mental health workers performing a similar role [ 23 , 30 , 39 , 62 ]. One of these studies was also a three-arm trial [ 30 ], with care as usual as the third arm. Further details about study characteristics can be seen in Table 1 below, with indication given of which comparators were used in the subsequent meta-analysis.
Participants in all studies were adults, although in one study participants were aged 55 or older [ 68 ]. In the majority of studies – twelve – participants were using community mental health services [ 23 , 28 , 30 , 35 , 39 , 44 , 50 , 54 , 62 , 63 , 66 , 76 ]. In three studies participants were recruited as inpatients [ 42 , 45 , 59 ], and in two studies participants were recruited as either inpatients or outpatients [ 71 , 74 ]. In two studies participants were recruited directly from depression clinics [ 31 , 68 ]. Most studies indicated diagnostic inclusion criteria, with seven studies specifying that participants would have diagnoses of either psychotic, or major depressive or mood disorders [ 23 , 30 , 39 , 42 , 45 , 54 , 66 ]. Two studies specified a diagnosis of bipolar disorder [ 44 , 50 ], one of major depressive disorder [ 31 ], one of mild to moderate depression and anxiety [ 68 ], one of either psychotic or personality disorders [ 71 ], and one of dual mental health, and drug or alcohol disorder [ 28 ]. Two studies defined eligibility by duration of mental illness with one specifying at least two years [ 71 ], and the other indicating that mental illness should be persistent [ 62 ]. A number of studies defined the population by service use history. In three studies eligibility criteria were defined by a minimum number of previous, recent psychiatric hospital admissions [ 42 , 45 , 54 ]. One study recruited participants as they approached hospital discharge [ 59 ], one study recruited participants who had been referred to specialist crisis and home treatment teams [ 76 ], and another study recruited participants who were under a court order mandating community mental health treatment [ 63 ].
Sample sizes
Samples sizes in the studies ranged from 21 [ 62 ] to 468 [ 54 ], with a total of 3329 participants in the 19 trials.
Interventions
While descriptions of peer support interventions remains thin in some studies published since the last review [ 8 ], a number of more recent studies do provide detailed descriptions of peer worker roles and what constitutes peer support. Peer workers were reported as delivering a range of different interventions. Five studies reported peer workers working in case management roles [ 23 , 30 , 39 , 42 , 54 ]. Typically, peer workers were expected to fulfil a similar, brokerage-type case management function to other mental health workers, and in addition, to role model their own strengths and experiences of recovery [ 39 ], or to provide social support by arranging social activities [ 42 ]. Three studies reported peer workers working in mentoring or coaching roles [ 44 , 45 , 50 ]. Mentoring and coaching roles varied considerably from offering a very loosely described partnership relationship that aimed to be different to a clinician-patient relationship [ 45 ], to structured online coaching to support participants in producing a detailed, behaviourally-informed recovery plan [ 44 ]. Three studies described peer workers providing support for self-management [ 31 , 62 , 76 ]; for example, in one study peer workers provided one-to-one assistance with rehabilitation goals set by occupational therapists [ 62 ], while in another peer workers supported participants to complete a structured recovery workbook [ 76 ]. Another three studies describing peer workers offering support for recovery [ 59 , 63 , 71 ]. What support for recovery entailed was generally poorly defined, with the exception of Mahlke and colleagues [ 71 ], describing in some detail how peer workers were trained and supported to reflect on and make use of their own experiences as a resource in supporting others with their recovery, but also reported that the intervention was not further manualised, and that peer workers had flexibility in the role, with an emphasis on enhancing the sense of control over their lives that people experienced. Two studies reported peer workers providing support for living independently in the community [ 28 , 66 ]. Peer support in both studies had a strong social focus and in the case of the latter [ 66 ], support was highly individualised and self-directed, involving the peer worker helping the individual to access social support that they identified themselves. Other studies described peer workers providing support for shared decision making in clinical consultations, again with a strong focus on a structured self-management approach [ 74 ], delivering a cognitive behavioural intervention using a structured workbook [ 68 ], and working in a healthcare assistant role [ 35 ].
Most peer support was provided face-to-face but in one study peer support was provided either face to face or by telephone [ 31 ], and in two studies peer support was provided online [ 44 , 50 ]. We note that in three studies peer workers were employed by peer-led organisations or agencies [ 23 , 63 , 66 ]. As noted above, four studies evaluated peer workers as a substitute for other mental health workers working in a similar role, three of those in a case management capacity [ 23 , 30 , 39 ], and in the fourth, providing support for self-management [ 62 ]. In all other studies peer support was adjunctive to care as usual or evaluated as an enhancement to another intervention.
Level of support for peer support interventions
The majority of studies – fourteen and thirteen respectively – described the support and/ or supervision provided to peer workers to deliver the peer support intervention [ 23 , 28 , 35 , 42 , 44 , 45 , 54 , 59 , 62 , 63 , 66 , 68 , 71 , 76 ], and the peer support-specific training provided to peer workers [ 31 , 35 , 39 , 44 , 45 , 54 , 59 , 62 , 63 , 66 , 71 , 76 , 85 ]. In contrast, only five studies explicitly described the theory, processes or understandings of peer support that underpinned the intervention evaluated [ 23 , 28 , 35 , 54 , 71 ].
There was variation in the degree of reporting of support given to peer workers. Reporting of training provided varied from noting that peer workers had received accredited peer specialist training prior to delivering the intervention [ 44 ], to a more detailed description of an extended, structured training program describing module content and mode of delivery [ 71 ]. Description of the support and supervision provided for peer workers also varied, from studies that simply reported that peer workers were provided with support and supervision for the duration of the study [ 59 ], to one which described in some detail the areas covered during weekly, 90 min group supervision sessions for peer workers [ 45 ]. One study said that supervision was provided by a peer support coordinator, with preference being given to employing someone with lived experience of mental illness in that role [ 62 ], while another stated that the director of the consumer case manager team was a consumer [ 23 ]. However no studies clearly stated that supervision for peer workers was provided by someone who was themselves employed to use their personal experiences of mental distress or of having used mental health services in the role. Theory, processes and understanding of peer support also varied in description, with one study [ 71 ] describing a specific peer support change model that underpinned the intervention, while others gave a more general description of the processes that characterise peer support as distinctive from other forms of mental health support [ 35 ].
Three studies did not report any of these organisational support components (dedicated peer support training; underlying theory; support for peer support) [ 30 , 50 , 74 ], and four reported just one component [ 31 , 39 , 42 , 68 ]. In contrast, four studies reported all three components [ 23 , 35 , 54 , 71 ], and eight reported two out of three [ 28 , 44 , 45 , 59 , 62 , 63 , 66 , 76 ].
Studies reported measuring thirteen of the eighteen outcomes of interest, with no studies of one-to-one peer support providing usable data assessing employment, symptoms of psychosis, self-stigma or experienced stigma, or emergency service use. Studies most often measured were hospitalisation [ 23 , 28 , 30 , 35 , 42 , 45 , 59 , 71 , 76 ] and quality of life [ 23 , 28 , 42 , 54 , 59 , 62 , 63 , 66 , 71 ], both measured in nine studies. We note that hospitalisation was variously measured as days in hospital, number of admissions or re-admissions, and community tenure (days spent living in the community, post-intervention, before hospital admission). Overall psychiatric symptoms were measured eight times [ 23 , 42 , 45 , 54 , 63 , 71 , 74 , 76 ], and both of social functioning [ 28 , 31 , 35 , 45 , 50 , 71 , 74 ] and social network support [ 23 , 28 , 35 , 42 , 45 , 63 , 76 ], seven times. Given that many studies used a more general measure of functioning - i.e. the Global Assessment of Function scale [ 29 ] – we subsequently report this outcome as General and Social Functioning. Satisfaction with services [ 31 , 35 , 42 , 45 , 76 ], empowerment [ 50 , 54 , 66 , 71 , 74 ] and working alliance [ 23 , 39 , 66 , 68 , 74 ] were all measured five times. We note that some studies reported both a participant rating of working alliance with staff and a staff rating of working alliance with the participant [ 23 , 74 ], while others only reported a participant rating of staff [ 39 ]. Self-rated recovery was measured in four studies [ 54 , 63 , 66 , 76 ], with wellbeing [ 28 , 42 , 45 ] and engagement with services [ 35 , 39 , 66 ] both measured in three studies. We grouped measures of physical health (e.g. two studies separately reported scores on the physical health subscale of the Lehman Quality of Life Scale) [ 26 ] with a more general measures of wellbeing (Life Skills Profile) [ 36 ], and so we report wellbeing as Physical Health and Wellbeing going forward. Depression and anxiety were also measured in three studies, with only Seeley and colleagues [ 68 ] using a separate measure for each, Proudfoot and colleagues [ 50 ] using a generalised measure for both, and Hunkeler and colleagues [ 31 ] measuring depression only. As a result we retain Depression and Anxiety as a single outcome for the purposes of this review. Finally, hope was measured in two studies [ 44 , 45 ]. Details of the specific tools used to measure these outcomes in each study can be found in Table 1 and are discussed further in the context of the meta-analysis reported below.
Risk of bias
The Risk of Bias ratings are displayed in Fig. 2 . Sequence generation was not sufficiently described in 7 of the 19 trials and was at high risk of bias in one trial. Concealment of the allocation sequence was not sufficiently described in 11 trials, and again at high risk of bias in one trial. Lack of blinding of assessors created a high risk of bias in 3 studies, and in 8 further trials it was unclear if assessors were blind. At the trial level, 3 were at high risk of bias for missing data (i.e. attrition bias) and 6 were unclear. Included studies may have measured but not reported outcomes that are included in this review; 10 with unclear description and 4 with high risk of reporting bias. Seven of the 19 studies [ 44 , 50 , 59 , 63 , 68 , 71 , 76 ] were at low risk of bias on at least three of the five bias categories and not high risk of bias for any category (i.e. might be described as being of low to moderate risk of bias overall), with the majority of those studies having been published since previous reviews. However on balance, overall quality of trials, when compared to previous reviews, remains low to moderate.
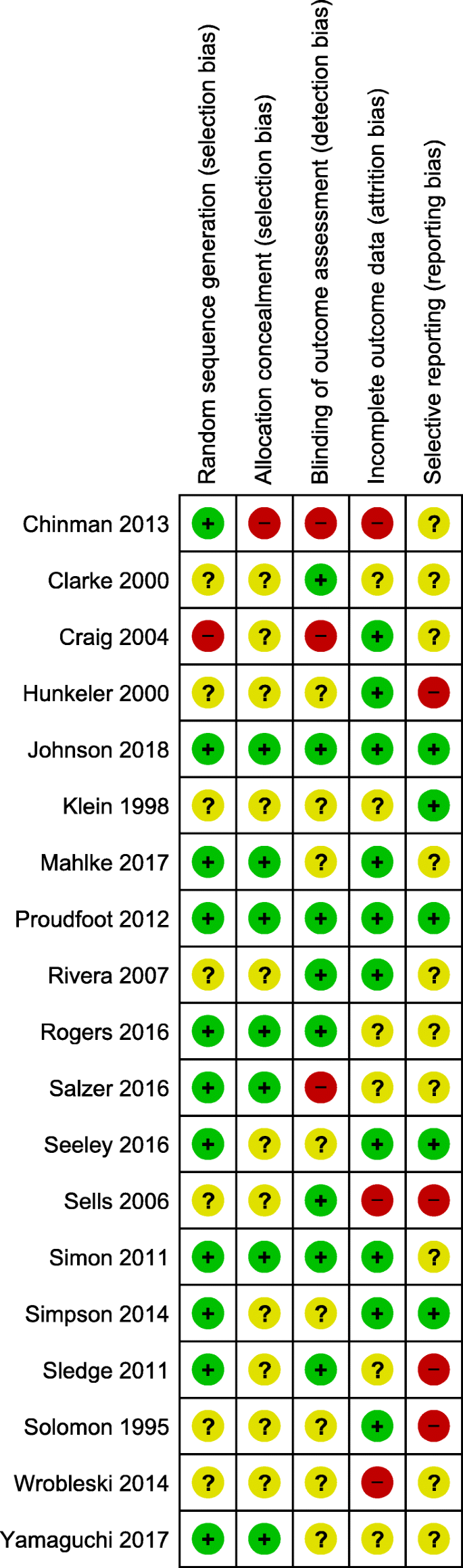
Summary of risk of bias of included studies
Quantitative synthesis
Data were available for the meta-analysis from fourteen of the nineteen trials included in the review (sixteen papers), with two or more trials contributing to meta-analyses of nine of our original outcomes. Because of the way data were reported in the studies, we analyse these as eleven outcomes, analysing days in hospital and hospitalised as two discrete outcomes in place of hospitalisation, and separating working alliance into staff-rated and client-rated outcomes. This analysis includes data obtained from one study after contacting study authors [ 74 ]. The number of studies contributing data to each outcome included in the analyses can be seen in Table 2 below. Median length of follow-up was 12 months post randomisation, ranging from 2.5 to 24 months. In the following analyses a positive standardised mean difference (SMD) for the following outcomes - quality of life, social network support, empowerment, recovery, service satisfaction, working alliance (client and staff rated) - indicates the peer support intervention being more effective than the control condition, the opposite being the case for the following; general psychiatric symptoms, depression and anxiety, days in hospital and hospitalised.
Five trials reported the dichotomous outcome of whether hospitalised during follow-up period or not. Follow-up ranged from 3 to 24 months with data on a total of 497 participants. The risk of being hospitalised was reduced by 14% for those receiving peer support (RR = 0.86: 95% CI 0.66, 1.13). Moderate heterogeneity (I 2 = 38%) was found across trials for this outcome. A similar result of a non-significant effect of peer support (SMD = -0.10: 95% CI -0.34, 0.14) and moderate heterogeneity (I 2 = 39%) was found for the days in hospital outcome. The five trials in this meta-analysis had follow-up ranging from 9 to 24 months and a total sample size of 453.
Six trials reported overall psychiatric symptoms with follow-up ranging from 6 to 24 months. Total sample size was 857. There was no evidence of the effect of peer support on symptoms; pooled standardised mean difference was − 0.01 (95% CI -0.21, 0.20). There was a high level of heterogeneity across trials, I 2 = 53%, χ 2 test of heterogeneity. Q = 10.7, p = 0.057.
Quality of life
A total of 688 participants had quality of life data reported from five trials with follow-up ranging from 12 to 24 months. No effect of peer support was found on quality of life, SMD = 0.08 (95% CI -0.11, 0.26) with moderate heterogeneity across trials, I 2 = 32%.
Three trials reported appropriate recovery data with follow-up ranging from 12 to 18 months and a total sample size of 593. Peer support is shown to have a small but statistically significant benefit on recovery (SMD = 0.22: 95% CI 0.01, 0.42: p = 0.042) (Fig. 3 ). Only moderate heterogeneity is indicated, I 2 = 38%.
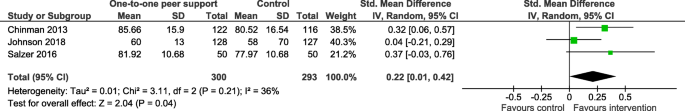
Forest plot for recovery outcome
Four trials with a total sample size of 519 participants and follow-up ranging from 6 to 12 months reported empowerment related outcomes. Empowerment was significantly higher in those receiving peer support, a small effect size, SMD = 0.23 (95% CI 0.04, 0.42: p = 0.020) (Fig. 4 ). Heterogeneity was low, I 2 = 14%.
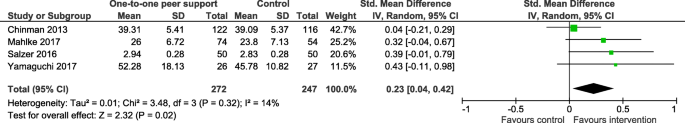
Forest plot for empowerment outcome
Satisfaction with services outcome data was available from two trials and a total of 286 participants. Follow-up in the two trials ranged from 12 to 18 months. No effect of peer support was found (SMD = 0.19: 95% CI − 0.05, 0.42) with no heterogeneity, I 2 = 0%.
General and social functioning
Three trials provided data for the general and social functioning outcome on a total sample size of 181. Follow-up in the two trials ranged from 6 to 12 months. No effect of peer support was found (SMD = 0.01: 95% CI -0.32, 0.35) with little heterogeneity, I 2 = 21%.
Four trials reported social network support outcome data with follow-up ranging from 12 to 24 months and a total sample size of 512 participants. While the pooled SMD = 0.09 (95% CI -0.25, 0.42) indicated no effect of peer support on social network support, there is significant heterogeneity across the trials, I 2 = 67%, χ 2 test of heterogeneity. Q = 9.2, p = 0.027.
Working alliance
Client rated working alliance about staff was reported in three trials and by a total of 213 participants. Follow-up ranged from 6 to 24 months. No heterogeneity was found across trials, I 2 = 0%, but the SMD = 0.24 (95% CI -0,03, 0.51: p = 0.080) indicates a potentially positive outcome for peer support. The SMD = 0.15 (95% CI -0.18, 0.48) was lower for staff ratings of the working alliance, again with no heterogeneity, I 2 = 0%. This outcome was only rated in 2 trials, a total of 139 participants.
Subgroup analyses
Only two outcomes – overall psychiatric symptoms and social network support – satisfied our condition of sufficient heterogeneity in the data to warrant undertaking subgroups analyses (see Table 3 below). We conducted subgroups analyses of those outcomes as defined earlier: adjunctive peer support interventions compared to those where peer workers were working in a similar or substitute role to other mental health workers; studies reporting a higher level of organisational support for peer support compared to those studies reporting a lower level of organisational support for peer support. These analyses did not explain heterogeneity with respect to overall psychiatric symptoms. A single study [ 42 ], reporting a lower level of organisation support for peer support, found a moderate, significant increase in social network support for people in the peer support arm of the trial (SMD = 0.50: 95% CI 0.14, 0.87), compared to three other studies with a higher level of organisational support for peer support where no significant difference in social network support was found (SMD = -0.04: 95% CI -0.37, 0.28) (Fig. 5 ). It can also be seen in Table 3 that there is evidence that whether peer support is being provided as adjunctive to usual care or as a substitute role impacts the effectiveness of peer support in increasing social network support, Qint = 4.27, p = 0.039. The effect of peer support is significantly greater when it is delivered as an adjunctive, SMD = 0.23, as opposed to substitute intervention, SMD = -0.30, a difference of 0.53 (Fig. 6 ).
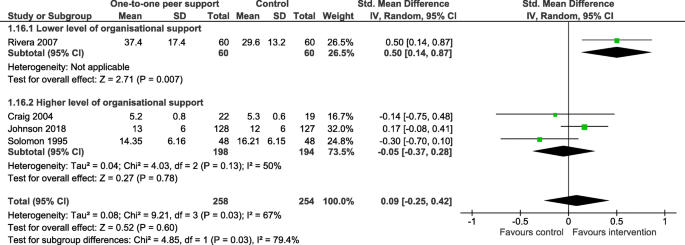
Sub group analysis; social network support by level of organisational support
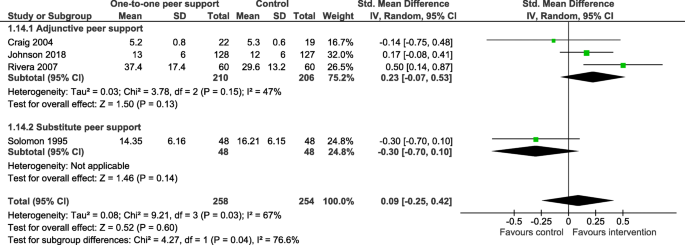
Subgroup analysis; social network support by type of peer support
Our review has indicated that a number of additional studies of one-to-one peer support have been published in the years following previous systematic reviews, suggesting that it has become viable to consider different modalities of peer support – e.g. group, one-to-one, peer-led services – in separate reviews. Studies remain predominantly conducted in the US, but with a gradual increase in studies being conducted in Europe and beyond. With health systems operating differently in different countries, caution does need to be taken when considering any results in the round.
While this review is focused on one-to-one peer support, we still see the heterogeneity of intervention observed by Pitt [ 7 ] and Lloyd Evans [ 8 ] across modalities of peer support. However it is interesting to note that most studies of peer workers in paraclinical roles, including case-management [ 23 , 30 , 39 , 42 ] and healthcare assistant roles [ 35 ], are now well over 10 years old, as are the majority of studies that compare peer workers to other mental health workers performing a similar role (‘substitute’ peer support) [ 23 , 30 , 39 ]. It is also worth noting that none of those studies of peer workers in paraclinical roles, or of peer workers in substitute roles, contributed data to analyses of those outcomes where a significant positive effect of peer support was found (recovery and empowerment).
Peer support interventions evaluated in more recent studies, in contrast, are almost exclusively evaluating adjunctive peer support, and tend to have either a structured, behavioural focus [ 44 , 62 , 68 , 74 , 76 ], or a more social focus, with peer workers providing a less structured, more peer-led support for recovery [ 45 , 59 , 63 , 66 , 71 ]. We suggest that there is potential, as more trials are published, of conducting focused reviews of specific groups or families of similar one-to-one peer support interventions.
We observe that a wide range of outcomes continue to be used. Of the original list of outcomes considered by Lloyd Evans and colleagues [ 8 ], we found that neither employment nor symptoms of psychosis were measured in the nineteen trials of one-to-one peer support that we reviewed. While Pitt and colleagues [ 7 ] found a small reduction in emergency service use for people receiving peer support we did not include data on emergency service use in our review as we excluded self-reported service use data from our analysis; Pitt and colleagues [ 7 ] themselves had suggested that recall bias and selective reporting of this outcome undermined the reliability of this particular finding.
While measures of general psychiatric symptoms were used in nearly half of all trials, measures of specific symptoms – of depression – were only used in those studies which exclusively recruited from a population diagnosed with depression [ 31 , 50 , 68 ]. Of our additional set of, largely, more socially-focused outcomes, neither internalised nor experienced stigma have been measured to date, although social functioning, social network support and working alliance were all measured in multiple studies, including in older trials [ 23 , 35 ]. If we consider just those outcomes used in multiple studies (outcomes included in our meta-analysis), we see a more focused outcomes-set emerging, balancing clinically-orientated outcomes of general severity of symptoms, functioning and hospitalisation with a set of self-reported, psychosocial outcomes including empowerment, recovery, working alliance and social network support.
As with previous reviews, once data from multiple studies were pooled, we found no difference between peer support and control across the majority of outcomes we considered. This included hope, where Lloyd Evans and colleagues [ 8 ] found a moderate positive impact of peer support, but we note again that their review included peer support provided to groups while we found insufficient studies of one-to-one peer support reporting measurement of hope as an outcome. However, our review does suggest that trial participants offered one-to-one peer support in mental health services experience modest but significant improvement in empowerment and self-reported recovery compared to control group participants, the latter reflecting similar findings by Lloyd Evans and colleagues [ 8 ].
Studies reporting empowerment were for the most part were published since the 2013 [ 7 ] and 2014 [ 8 ] reviews, reflecting the suggestion made by Bellamy and colleagues [ 87 ] that more recent studies indicate that new peer support initiatives might usefully be directed to interventions that, broadly speaking, support individual empowerment. We grouped assessments of empowerment and related constructs together for the purposes of this review, and the studies in the analysis variously used the Patient Activation Measure [ 57 ], the General Self-Efficacy Scale [ 73 ], and the Empowerment Scale [ 67 ]. As a construct, patient activation has a clear focus on the extent to which the individual is able to access the healthcare they need, and is a good fit for interventions that specifically address the way in which the individual engages with their mental health care [ 54 , 74 ]. Self-efficacy taps into the individual’s ability to make use of a wider range of support and care, while the Empowerment Scale has been shown to weight heavily on hope as a factor [ 67 ]. Again, these measures would seem appropriate for interventions focused on supporting recovery [ 63 ] and independence [ 66 ] respectively.
Studies reporting recovery as an outcome again used a range of measures. Salzer and colleagues [ 66 ] use the Recovery Assessment Scale [ 65 ], which measures recovery across five domains of personal confidence, hope, willingness to ask for assistance, goal and success orientation, and coping, and as such would seem particularly attuned to an intervention designed to support independent living. Johnson and colleagues [ 76 ] use the Questionnaire about the Process of Recovery [ 78 ], which comprises an ‘intrapersonal’ subscale that relates to “intrapersonal tasks that an individual is responsible for carrying out and that they complete in order to rebuild their life”, and an ‘interpersonal’ subscale relating to “individuals’ ability to reflect on their value in the external world and on how recovery is facilitated by external processes and interpersonal relationships with others”. Seventeen of the 22 items that comprise the measure load onto the ‘intrapersonal’ subscale, as would seem apposite for the evaluation of a self-management intervention. Chinman and colleagues [ 54 ] use the Mental Health Recovery Measure [ 55 ], measuring recovery in the seven domains of Overcoming Stuckness, Self-Empowerment, Learning and Self-Re-definition, Basic Functioning, Overall Well-Being, New Potentials, and Advocacy/Enrichment. This balance between functioning and wellbeing, and then moving on and realising potential seems well-suited to the case management function of the intervention.
These findings indicate what would seem to be an important relationship between positive impact on outcome, the assessment tool used and the intervention. As such we would suggest that trials exploring these, or indeed other outcomes, in the future should be cognisant of the constructs informing specific assessment tools (e.g. domains, subscales), and ensure that these relate closely to the mechanisms underpinning particular peer worker interventions. We reiterate calls in previous reviews [ 7 ] for a clearer understanding of the mechanisms of peer support, and the theory driven selection of outcomes that relate specifically to what peer workers do.
We note that one further outcome, client-rated working alliance, while not quite significant, demonstrated a similar effect size to the other positive outcomes. In two studies [ 23 , 39 ] participants rated working alliance with peer workers in the intervention arm of the trial, compared to working alliance with mental health professional in the control arm, while in the third study [ 74 ] working alliance with a mental health professional was rated in both arms of the trial, with and without additional peer support. Once data were pooled there was a relatively small sample size for this outcome; more data would produce a more precise estimate of the effect size. This finding suggests that there is merit in exploring working alliance in future studies of one-to-one peer support, especially given other research indicating a potential mechanism for peer support in bridging and enabling connection between service users and mental health professionals [ 21 ].
We note that while both measures of hospitalisation analysed were in a positive direction (i.e. a reduction in days in hospital and risk of hospitalisation), neither were significant. The lack of positive association between the offer of peer support and reduction in psychiatric symptoms also suggests that, while studies are using a balance of clinical and more psycho-socially focused outcomes, one-to-one peer support in mental health services is unlikely to impact on clinical outcomes.
There was significant heterogeneity of data for two outcomes (overall psychiatric symptoms and social network support). While our subgroup analyses did not explain heterogeneity with respect to overall psychiatric symptoms, analyses did offer insight into the relationship between peer support and social network support. Finding that a single study [ 42 ], reporting a lower level of organisation support for peer support, indicated a moderate, significant increase in social contacts, while studies reporting a higher level of support for peer support did not, appears counter-intuitive. Looking closely, authors note that the increase in positive outcome was accounted for by additional contacts with peer workers and professional staff, rather than any increase in contacts with family or friends [ 42 ].
Furthermore, peer support that was provided in addition to care as usual was significantly more likely to increase social network support than peer support provided by peer workers employed in a substitute role. At the least, these findings suggest that it is worth considering measuring social network support in future studies, while giving consideration to how the peer support intervention might be functioning to increase social contacts. In addition, we would suggest that we have demonstrated that our approach to operationalising an analysis of organisational support for peer support is feasible and might be pursued in future reviews, subject to the availability of suitable data. Continued improvement in reporting peer support interventions might usefully include good description of the organisational support provided for peer workers [ 88 ].
While cost was not one of our outcomes of interest we note that claims have been made about the potential contribution to reducing the cost of mental healthcare that peer support might make [ 5 ]. Only one of the nineteen trials included in our review considered cost, but was not sufficiently powered to draw any conclusions [ 59 ]. As such, analysis of the cost-effectiveness of one-to-one peer support in mental health services is largely absent from the evidence base to date.
Limitations
Overall quality of trials, when compared to previous reviews, remains low to moderate, although we note that, in our set of trials of one-to-one peer support, more recent trials appear less likely to have serious risk of bias and more likely to have low risk of bias on a majority of assessments, and so we tentatively suggest that the quality of studies is improving. Reporting bias, due to incomplete reporting of outcomes data, remains an issue and, as such, this downgrading of the quality of the overall evidence base does limit the strength of findings of this review. We note that for our two main positive outcomes, self-reported recovery and empowerment, all but one of the studies that reported measuring these outcomes included usable data in trial papers. However completeness of reporting of outcomes is essential to inform good quality evidence with respect to peer support in mental health services going forward.
In focusing on one-to-one peer support we have produced a more focused review than previous studies. However we acknowledge that studies remain heterogenous, especially with respect to clinical population (for example, only one study [ 71 ] specified chronicity of diagnosis). In addition, we note the range of terms used to describe peer support roles and acknowledge that our search might not have been wholly inclusive. Like all reviews, the validity of our study is defined by the strategy we describe above.
One-to-one peer support in adult mental health services has a modest, positive effect on empowerment and self-reported recovery, and might potentially also impact on measures of working alliance between service users and mental health workers, and social network support. It seems unlikely that one-to-one peer support has a positive impact on clinical outcomes such as symptoms or hospitalisation, given data available for this review, suggesting that the benefits of peer support are largely psychosocial, operating at both individual (interpersonal) and relational (intrapersonal) levels. The quality of reporting, both of trial methods and design of peer support interventions, has improved somewhat but needs to continue to do so - especially with respect to complete reporting of outcome measurements - in order to maximise the usefulness of the evidence base for service providers and policymakers. Future trials should also consider appropriate assessment of cost-effectiveness of peer support in mental health services.
While some older trials of one-to-one peer support evaluated peer workers working in paraclinical roles, and/ or in substitute roles, newer studies focus on peer workers providing adjunctive interventions; either structured, behavioural interventions, or more socially focused, self-directed, flexible support for recovery. This review suggests that future trials of one-to-one peer support in mental health services should focus on peer workers providing interventions that are additional to usual care; outcomes for peer support are no better than control where peer workers are compared to other mental health workers doing similar work, and might be worse for outcomes such as social network support, possibly because such roles do not enable peer workers to enact a more distinctive way of working.
We suggest that studies should carefully consider the specific mechanisms of action of peer support, with trials designed so that choice of assessment tools (the constructs that are measured) reflect the specific function of the peer support intervention and the distinctive way in which peers work compared to other mental health workers. If and where peer support is having a beneficial effect, there will be a greater likelihood of observing this in a more carefully designed trial. Furthermore, as the evidence base for peer support grows it would be methodologically desirable to conduct more focused reviews of groups of similar interventions (rather than continuing to review a heterogenous group of interventions as a whole). Finally, this review demonstrated the potential to explore heterogeneity in peer support, in relation to outcome, in terms of the quality of organisational support provided to peer workers.
It is of interest to compare our findings with the concurrent review of group peer support conducted by Lyons and colleagues. We similarly identified that heterogeneity of intervention remains a feature of the evidence base while noting that a small number of types or functions of peer support are emerging (with a number of trials of peer-supported self-management identified by both reviews). Both reviews are also indicative of a modest, positive effect of peer support on self-reported recovery and an absence of effect, in the evidence to date, on clinical outcomes. Again, both reviews indicate that reporting bias – incomplete reporting of outcomes – continues to undermine the quality of the evidence base as whole.
Availability of data and materials
The data that support the findings of this study are available from the corresponding author upon reasonable request.
Abbreviations
Confidence Interval
Diagnostic and Statistical Manual
Standard Mean Difference
Council of Australian Governments Health Council. The Fifth National Mental Health and Suicide Prevention Plan. 2017. http://www.coaghealthcouncil.gov.au/Portals/0/Fifth%20National%20Mental%20Health%20and%20Suicide%20Prevention%20Plan.pdf Accessed 17 June 2020.
Google Scholar
Health Education England. Stepping forward to 2020/21: The mental health workforce plan for England. 2017. https://www.basw.co.uk/system/files/resources/basw_62959-3_0.pdf Accessed 17 June 2020.
Ferri M, Amato L, Davoli M. Alcoholics anonymous and other 12-step programmes for alcohol dependence. Cochrane Database Syst Rev. 2006;19:005–32.
Dillon J. Hearing voices groups: creating safespaces to share taboo experiences. In: Romme M, Escher S, editors. Psychosis as a personal crisis: an experience-based approach. New York: Routledge; 2011.
Trachtenberg M, Parsonage M, Shepherd G. Peer support in mental health care: is it good value for money? London: Centre for Mental Health; 2013.
Repper J, Carter T. A review of the literature on peer support in mental health services. J Ment Health. 2011;20(4):392–411.
Article PubMed Google Scholar
Pitt V, Lowe D, Hill S, Prictor M, Hetrick SE, Ryan R, et al. Consumer-providers of care for adult clients of statutory mental health services. Cochrane Database Syst Rev. 2013;3:CD004807.
Lloyd-Evans B, Mayo-Wilson E, Harrison B, Istead H, Brown E, Pilling S, et al. A systematic review and meta-analysis of randomised controlled trials of peer support for people with severe mental illness. BMC Psychiatry. 2014;14:39.
Article PubMed PubMed Central Google Scholar
Pfeiffer PN, Heisler M, Piette JD, Rogers MA, Valenstein M. Efficacy of peer support interventions for depression: a meta-analysis. Gen Hosp Psychiatry. 2011;33(1):29–36.
Burke E, Pyle M, Machin K, Varese F, Morrison AP. The effects of peer support on empowerment, self-efficacy, and internalized stigma: a narrative synthesis and meta-analysis. Stigma Health. 2019;4(3):337–56.
Article Google Scholar
King AJ, Simmons MB. A systematic review of the attributes and outcomes of peer work and guidelines for reporting studies of peer interventions. Psychiatr Serv. 2018;69(9):961–77.
Gillard S, Foster R, Gibson S, Goldsmith L, Marks J, White S. Describing a principles-based approach to developing and evaluating peer worker roles as peer support moves into mainstream mental health services. Ment Health Soc Incl. 2017;21(3):133–43.
Oborn E, Barrett M, Gibson S, Gillard S. Knowledge and expertise in care practices: the role of the peer worker in mental health teams. Sociol Health Illn. 2019;41(7):1305–22.
Mead S, Filson B. Mutuality and shared power as an alternative to coercion and force. Ment Health Soc Incl. 2017;21(3):144–52.
Stewart S, Watson S, Montague R, Stevenson C. Set up to fail? Consumer participation in the mental health service system. Australas Psychiatry. 2008;16(5):348–53.
Faulkner A, Kalathil J. The freedom to be, the chance to dream: preserving used-led peer support in mental health. London: Together for Mental Wellbeing; 2012.
Gillard S, Edwards C, Gibson S, Owen K, Wright C. Introducing peer worker roles into UK mental health service teams: a qualitative analysis of the organisational benefits and challenges. BMC Health Serv Res. 2013;13:188.
Tse S, Tsoi EW, Wong S, Kan A, Kwok CF. Training of mental health peer support workers in a non-western high-income city: preliminary evaluation and experience. Int J Soc Psychiatry. 2014;60(3):211–8.
Cabral L, Strother H, Muhr K, Sefton L, Savageau J. Clarifying the role of the mental health peer specialists in Massachusetts USA insights from peer specialists supervisors and clients. Health Soc Care Community. 2014;22(1):104–12.
Stratford AC, Halpin M, Phillips K, Skerritt F, Beales A, Cheng V, et al. The growth of peer support: an international charter. J Ment Health. 2019;28(6):627–32.
Gillard S, Gibson S, Holley J, Lucock M. Developing a change model for peer worker interventions in mental health services: a qualitative research study. Epidemiol Psychiatr Sci. 2015;24(5):435–45.
Article CAS PubMed Google Scholar
American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 5th ed. Washington, DC: American Psychiatric Association Publishing; 2013.
Book Google Scholar
Solomon P, Draine J. One-year outcomes of a randomized trial of consumer case management. Eval Program Plan. 1995;18(2):345–57.
Overall J, Gorham D. The brief psychiatric rating scale. Psychol Rep. 1962;10:799–812.
Pattison EM. A theoretical-empirical base for social system therapy. In: Foulks EF, Wintrob RN, Westermyer J, et al., editors. Current perspectives in cultural psychiatry. New York: Spectrum; 1977.
Lehman AF. A quality of life interview for the chronically mentally ill. Evaluation and Program Planning. 1988;11:51–62.
Horvath AO, Greenberg LS. Development and validation of the working Alliance inventory. J Couns Psychol. 1989;36(2):223–33.
Klein AR, Cnaan RA, Whitecraft J. Significance of peer social support with dually diagnosed clients: findings from a pilot study. Res Soc Work Pract. 1998;8(5):529–51.
Hall RCW. Global assessment of functioning. Psychosomatics. 1995;36(3):267–75.
Clarke GN, Herinckx HA, Kinney RF, Paulson RI, Cutler DL, Lewis K, Oxman E. Psychiatric hospitalizations, arrests, emergency room visits, and homelessness of clients with serious and persistent mental illness: findings from a randomized trial of two ACT programs vs. usual care. Ment Health Serv Res. 2000;2(3):155–64.
Hunkeler EM, Meresman JF, Hargreaves WA, Fireman B, Berman WH, Kirsch AJ, et al. Efficacy of nurse telehealth care and peer support in augmenting treatment of depression in primary care. Arch Fam Med. 2000;9(8):700–8.
Reynolds WM, Kobak KA. Hamilton depression inventory: a self- report version of the Hamilton depression rating scale (HSRS): professional manual. Odessa: Psychological Assessment Resources Inc.; 1995.
Beck AT, Steer RA, Brown GK. Beck depression inventory II manual. San Antonio: Psychological Corporation; 1996.
Ware JE, Snow KK, Kosinski M, Gandek B. SF-36 health survey: manual and interpretation guide. Boston: The Health Institute, New England Medical Center; 1993.
Craig T, Doherty I, Jamieson-Craig R, Boocock A, Attafua G. The consumer-employee as a member of a mental health assertive outreach team. I. Clinical and social outcomes. J Ment Health. 2004;13(1):59–69.
Rosen A, Hadzi-Pavlovic D, Parker G. The life skills profile: a measure assessing function and disability in schizophrenia. Schizophr Bull. 1989;15(2):325–37.
Power MJ, Champion LA, Aris SJ. The development of a measure of social support: the significant others (SOS) scale. Br J Clin Psychol. 1988;27:349–58.
Ruggeri M, Lasalvia A, Dall'Agnolla R, van Wijngaarden B, Knudsen HC, Leese M, et al. Development and use of the Verona expectations for care scale (VECS) and the Verona service satisfaction scale (VSSS) for measuring expectations and satisfaction with community-based psychiatric services in patients, relatives and professionals. Psychol Med. 1993;23:511–23.
Sells D, Davidson L, Jewell C, Falzer P, Rowe M. The treatment relationship in peer-based and regular case management for clients with severe mental illness. Psychiatr Serv. 2006;57(8):1179–84.
Barrett-Lennard GT. Dimensions of therapist response as causal factors in therapeutic change. Psychol Monogr Gen Appl. 1962;76(43):1–36.
American Association of Community Psychiatrists. Level of care utilization system for psychiatric and addiction services, adult version. Pittsburgh: American Association of Community Psychiatrists; 2000.
Rivera JJ, Sullivan AM, Valenti SS. Adding consumer-providers to intensive case management: does it improve outcome? Psychiatr Serv. 2007;58(6):802–9.
Derogatis LR, Melisaratos N. The brief symptom inventory: an introductory report. Psychol Med. 1983;13:595–605.
Simon GE, Ludman EJ, Goodale LC, Dykstra DM, Stone E, Cutsogeorge D, et al. An online recovery plan program: can peer coaching increase participation? Psychiatr Serv. 2011;62(6):666–9.
Sledge WH, Lawless M, Sells D, Wieland M, O'Connell MJ, Davidson L, et al. Effectiveness of peer support in reducing readmissions of persons with multiple psychiatric hospitalizations. Psychiatr Serv. 2011;62(5):541–4.
Birchwood M, Smith J, Cochrane R, Wetton S, Copestake S. The social functioning scale: the development and validation of a new scale of social adjustment for use in family intervention programmes with schizophrenic patients. Br J Psychiatry. 1990;157:853–9.
Brouwer D, Meijer RR, Weekers AM, Baneke JJ. On the dimensionality of the dispositional Hope scale. Psychol Assess. 2008;20(3):310–5.
Ganju V. The MHSIP Consumer Survey. Arlington: Research Institute, National Association of State Mental Health Program Directors; 1999.
McMillan DW, Chavis DM. Sense of community: a definition and theory. J Community Psychol. 1986;14:6–23.
Proudfoot J, Parker G, Manicavasagar V, Hadzi-Pavlovic D, Whitton A, Nicholas J, et al. Effects of adjunctive peer support on perceptions of illness control and understanding in an online psychoeducation program for bipolar disorder: a randomised controlled trial. J Affect Disord. 2012;142(1–3):98–105.
Goldberg D, Bridges K, Duncan-Jones P, Grayson D. Detecting anxiety and depression in general medical settings. BMJ. 1988;297:897–9.
Article CAS PubMed PubMed Central Google Scholar
Marks IM. Behavioural psychotherapy: Maudsley pocket book of clinical management. Bristol: Wright; 1986.
Wallston BS, Wallston KA, Kaplan G, Maides S. Development and validation of the health locus of control (HLC) scale. J Consult Clin Psychol. 1976;44(4):580–5.
Chinman M, Oberman RS, Hanusa BH, Cohen AN, Salyers MP, Twamley EW, et al. A cluster randomized trial of adding peer specialists to intensive case management teams in the veterans health administration. J Behav Health Serv Res. 2013;42(1):109–21.
Bullock WA, Young SL. The mental health recovery measure (MHRM). In: Campbell-Orde T, Chamberlin J, Carpenter J, Leff HS, editors. Measuring the promise: a compendium of recovery measures. Cambridge: Human Services Research Institute; 2005.
Mueser K, Gingerich S, Salyers MP, McGuire AB, Reyes RU, Cunningham H. Illness management and recovery (IMR) scales (client and clinician versions). Concord: Psychiatric Research Center; 2004.
Hibbard JH, Stockard J, Mahoney ER, Tusler M. Development of the patient activation measure (PAM): conceptualizing and measuring activation in patients and consumers. Health Serv Res. 2004;39(4):1005–26.
Eisen S, Normand SL, Belanger AJ, Spiro A, Esch D. The revised behavior and symptom identification scale (BASIS-R): reliability and validity. Med Care. 2004;42(12):1230–41.
Simpson A, Flood C, Rowe J, Quigley J, Henry S, Hall C, et al. Results of a pilot randomised controlled trial to measure the clinical and cost effectiveness of peer support in increasing hope and quality of life in mental health patients discharged from hospital in the UK. BMC Psychiatry. 2014;14(1):30.
Beck AT, Steer RA. Manual for the Beck hopelessness scale. San Antonio: Psychological Corporation; 1988.
Euroqol Group. EuroQol - a new facility for the measurement of health-related quality of life. Health Policy. 1990;16:199–208.
Wrobleski T, Walker G, Jarus-Hakak A, Suto MJ. Peer support as a catalyst for recovery: a mixed-methods study. Can J Occup Ther. 2015;82(1):64–73.
Rogers ES, Maru M, Johnson G, Cohee J, Hinkel J, Hashemi L. A randomized trial of individual peer support for adults with psychiatric disabilities undergoing civil commitment. Psychiatr Rehabil J. 2016;39(3):248–55.
Cohen S, Mermelstein R, Kamarck T, Hoberman H. Measuring the functional components of social support. In: Sarason IG, editor. Social support: theory, research and applications. Dordrecht: Martinus Nijhoff Publishers; 1985.
Salzer M, Brusilovskiy E. Advancing recovery science. Reliability and validity properties of the recovery assessment scale. Psychiatr Serv. 2014;65(4):442–53.
Salzer MS, Rogers J, Salandra N, O’Callaghan C, Fulton F, Balletta AA, et al. Effectiveness of peer-delivered Center for Independent Living supports for individuals with psychiatric disabilities: a randomized, controlled trial. Psychiatr Rehabil J. 2016;39(3):239–47.
Rogers ES, Chamberlin J, Ellison ML, Crean T. A consumer constructed scale to measure empowerment among users of mental health services. Psychiatr Serv. 1997;48(8):1042–7.
Seeley JR, Manitsas T, Gau JM. Feasibility study of a peer-facilitated low intensity cognitive-behavioural intervention for mild to moderate depression and anxiety in older adults. Aging Ment Health. 2016. https://doi.org/10.1080/13607863.2016.1186152 .
Kroenke K, Spitzer RL, Williams JBW. The PHQ-9: validity of a brief depression severity measure. J Gen Intern Med. 2001;16:606–13.
Spitzer RL, Kroenke K, Williams JBW, Lowe B. A brief measure for assessing generalized anxiety disorder: the GAD 7. Arch Intern Med. 2006;166:1092–7.
Mahlke CI, Priebe S, Heumann K, Daubmann A, Wegscheider K, Bock T. Effectiveness of one-to-one peer support for patients with severe mental illness - a randomised controlled trial. Eur Psychiatry. 2016;42:103–10.
Guy W. Clinical Global Impressions. In: Guy W, editor. ECDEU assessment manual for psychopharmacology. Rockville: National Institute of Mental Health; 1976. p. 218–22.
Schwarzer R, Jerusalem M. Generalized self-efficacy scale. In: Weinman J, Wright S, Johnston M, editors. Measures in health psychology: a user’s portfolio. Windsor: NFER-Nelson; 1995. p. 35–7.
Yamaguchi S, Taneda A, Matsunaga A, Sasaki N, Mizuno M, Sawada Y, et al. Efficacy of a peer-led, recovery-oriented shared decision-making system: a pilot randomized controlled trial. Psychiatr Serv. 2017;68(12):1307–11.
McGuire-Snieckus R, McCabe R, Catty J, Hansson L, Priebe S. A new scale to assess the therapeutic relationship in community mental health care: STAR. Psychol Med. 2007;37(1):85–95.
Johnson S, Lamb D, Marston L, Osborn D, Mason O, Henderson C, et al. Peer-supported self-management for people discharged from a mental health crisis team: a randomised controlled trial. Lancet. 2018;392(10145):409–18.
Lubben J, Blozik E, Gillmann G, Iliffe S, von Renteln KW, Beck JC, Stuck AE. Performance of an abbreviated version of the Lubben social network scale among three European community-dwelling older adult populations. Gerontology. 2006;46:503–13.
Neil ST, Kilbride M, Pitt L, Nothard S, Welford M, Sellwood W, et al. The questionnaire about the process of recovery (QPR): a measurement tool developed in collaboration with service users. Psychosis. 2009;1(2):145–55.
Attkisson C, Zwick R. The client satisfaction questionnaire. Psychometric properties and correlations with service utilisation and psychotherapy outcome. Eval Program Plan. 1982;5:233–7.
Article CAS Google Scholar
Higgins JPT, Altman DG, Gotzsche PC, Juni P, Moher D, Oxman AD, et al. The Cochrane Collaboration’s tool for assessing risk of bias in randomised trials. BMJ. 2011;343:d5928.
Deeks J, Higgins JPT, Altman DG. Analysing data and undertaking meta-analyses. In: Higgins JPT, green S, editors. Cochrane handbook of systematic reviews of interventions version 5.1.0. London: Cochrane Collaborations; 2011.
Review Manager (RevMan) [Computer program]. Version 5.3. Copenhagen: The Nordic Cochrane Centre, The Cochrane Collaboration; 2014.
Solomon P, Draine J. The efficacy of a consumer case management team: 2-year outcomes of a randomized trial. J Ment Health Adm. 1995;22(2):135–46.
Solomon P, Draine J, Delaney MA. The working alliance and consumer case management. J Mental Health Adm. 1995;22(2):126–34.
Solomon P, Draine J. Service delivery differences between consumer and nonconsumer case managers in mental health. Res Soc Work Pract. 1996;6(2):193–207.
O'Connell MJ, Sledge WH, Staeheli M, Sells D, Costa M, Wieland M, et al. Outcomes of a peer Mentor intervention for persons with recurrent psychiatric hospitalization. Psychiatr Serv. 2018;69(7):760–7.
Bellamy C, Schmutte T, Davidson L. An update on the growing evidence base for peer support. Ment Health Soc Incl. 2017;21(3):161–7.
Charles A, Thompson D, Nixdorf R, Ryan G, Shamba D, Kalha J, et al. Typology of modifications to peer support work for adults with mental health problems: systematic review. Br J Psychiatry. 2020;216(6):301–7.
Download references
Acknowledgements
Not applicable.
This work was supported by the UK National Institute for Health Research, Programme Grants for Applied Research funding programme (grant number RP-PG-1212-20019). This paper presents independent research funded by the National Institute for Health Research (NIHR). The views expressed are those of the authors and not necessarily those of the NHS, the NIHR or the Department of Health and Social Care. The funder played no roll in the design of the study, the collection, analysis, and interpretation of data, or in writing the manuscript.
Author information
Authors and affiliations.
Population Health Research Institute, St George’s, University of London, Cranmer Terrace, London, SW17 0RE, UK
Sarah White, Rhiannon Foster, Jacqueline Marks, Rosaleen Morshead, Lucy Goldsmith, Jacqueline Sin & Steve Gillard
School of Health Sciences, City, University of London, London, EC1V 0HB, UK
Sally Barlow
You can also search for this author in PubMed Google Scholar
Contributions
SW and SG contributed to formulating the research question, designing the study, carrying it out, analysing the data and writing the article; RF, JM and RM contributed to designing the study, carrying it out, analysing the data and writing the article; LG, SB and JS contributed to designing the study and writing the article. The author(s) read and approved the final manuscript.
Corresponding author
Correspondence to Steve Gillard .
Ethics declarations
Ethics approval and consent to participate, consent for publication, competing interests.
The authors declare that they have no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1..
Search strategy for MEDLINE, EMBASE and PsychINFO using the OVID interface.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
White, S., Foster, R., Marks, J. et al. The effectiveness of one-to-one peer support in mental health services: a systematic review and meta-analysis. BMC Psychiatry 20 , 534 (2020). https://doi.org/10.1186/s12888-020-02923-3
Download citation
Received : 24 June 2020
Accepted : 18 October 2020
Published : 11 November 2020
DOI : https://doi.org/10.1186/s12888-020-02923-3
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Peer support
- Peer worker
- Mental health services
- Randomised clinical trial
- Systematic review
- Meta-analysis
- Empowerment, recovery
- Social network
BMC Psychiatry
ISSN: 1471-244X
- General enquiries: [email protected]
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Subst Abuse Rehabil
Benefits of peer support groups in the treatment of addiction
Kathlene tracy.
1 Community Research and Recovery Program (CRRP), Department of Psychiatry, New York University School of Medicine
2 New York Harbor Healthcare System (NYHHS), New York
Samantha P Wallace
3 Department of Community Health Sciences, State University of New York Downstate School of Public Health, Brooklyn, NY, USA
Peer support can be defined as the process of giving and receiving nonprofessional, nonclinical assistance from individuals with similar conditions or circumstances to achieve long-term recovery from psychiatric, alcohol, and/or other drug-related problems. Recently, there has been a dramatic rise in the adoption of alternative forms of peer support services to assist recovery from substance use disorders; however, often peer support has not been separated out as a formalized intervention component and rigorously empirically tested, making it difficult to determine its effects. This article reports the results of a literature review that was undertaken to assess the effects of peer support groups, one aspect of peer support services, in the treatment of addiction.
The authors of this article searched electronic databases of relevant peer-reviewed research literature including PubMed and MedLINE.
Ten studies met our minimum inclusion criteria, including randomized controlled trials or pre-/post-data studies, adult participants, inclusion of group format, substance use-related, and US-conducted studies published in 1999 or later. Studies demonstrated associated benefits in the following areas: 1) substance use, 2) treatment engagement, 3) human immunodeficiency virus/hepatitis C virus risk behaviors, and 4) secondary substance-related behaviors such as craving and self-efficacy. Limitations were noted on the relative lack of rigorously tested empirical studies within the literature and inability to disentangle the effects of the group treatment that is often included as a component of other services.
Peer support groups included in addiction treatment shows much promise; however, the limited data relevant to this topic diminish the ability to draw definitive conclusions. More rigorous research is needed in this area to further expand on this important line of research.
Introduction
Peer support can be defined as the process of giving and receiving nonprofessional, nonclinical assistance from individuals with similar conditions or circumstances to achieve long-term recovery from psychiatric, alcohol, and/or other drug-related problems. Historically, peer support has been shown to be a key component of many existing addiction treatment and recovery approaches such as the community reinforcement approach, 1 – 11 therapeutic communities, 12 , 13 and 12-step programs; 14 , 15 the community reinforcement approach has demonstrated the importance of valued social roles in maintaining abstinence, which is the foundation of the peer support relationship. 16 – 18
Varying approaches that include a mixture of services such as peer support groups, individual counseling, and case management have emerged as a highly effective and empowering method to manage the social context of health issues and are particularly popular in the substance abuse and mental health fields. 19 As it relates to substance abuse recovery for individuals and families, addiction peer support services have emerged across time due to the shift from a biopsychosocial approach to a sustained recovery management approach to treat addictions. 20 While in many cases, peer support groups do not replace the need for formal treatments or supervisory clinical guidance due to peers not having sufficient training to manage psychiatric conditions or high-risk situations, they still offer an augmentation to treatment that provides many benefits to individuals with substance use disorders. 21
Terminology
Various terminologies are used interchangeably within the literature to describe peer-related support and contexts. For the purposes of this article, we attempted to utilize consistent language wherever possible. However, in certain instances, a term may be part of a broader term such as mentorship is a type of peer support, but mentorship is specific to an individual in later recovery providing peer support to someone in earlier recovery, which requires additional specification. 21 We adapted and built upon White’s 20 definition of peer support to include individuals with similar conditions or circumstances and inclusion of recovery from psychiatric problems in addition to substance use disorders. We also included this broadened scope in our definition of peer mentorship. Table 1 provides key peer support terms used throughout this review article and definitions. 22 – 24
Key terms and definitions related to peer support
| Terms | Definitions |
|---|---|
| Peer support | The process of giving and receiving nonprofessional, nonclinical assistance from individuals with similar conditions or circumstances to achieve long-term recovery from psychiatric, alcohol, and/or other drug-related problems |
| Recovery | A process of change through which individuals improve their health and wellness, live self-directed lives, and strive to reach their full potential |
| Peer support group | Where people in recovery voluntarily gather together to receive support and provide support by sharing knowledge, experiences, coping strategies, and offering understanding |
| Peer provider (eg, certified peer specialist, peer support specialist, mentor, and recovery coach) | A person who uses his or her lived experience of recovery from mental illness and/or addiction, plus skills learned in formal training, to deliver services in behavioral health settings to promote mind–body recovery and resiliency |
| Peer mentorship | Where individuals in later recovery provide nonprofessional, nonclinical assistance to individuals in earlier recovery with similar conditions or circumstances to achieve long-term recovery from psychiatric, alcohol, and/or other drug-related problems |
Residential and sober living
Since the 1960s, a variety of residential options have emerged to help people with alcohol and drug addictions. These programs based on the social model of recovery provide support for people in recovery from alcohol addiction in a residential environment that focuses on Alcoholics Anonymous (AA) philosophy and practices. 25 AA practice follows the 12-step guidelines based on spiritual principles and the assumption that addiction is a disease. 26 Prior work utilizing social model programs can be found as early as the 1940s. 27 – 29 The types of social model programs available include social setting detoxification, residential social model recovery programs, neighborhood recovery centers, and sober living houses. 27
Sober living houses are alcohol- and drug-free living environments for a group of peers in recovery. Utilizing a peer-oriented social model modality, sober living houses rely on mutual sobriety support, self-efficacy, and resident participation. California Sober Living Houses and Oxford Houses are two variations of sober living houses. 30 – 32 Previous studies have shown sober living houses to be beneficial 33 and effective 34 , 35 in assisting in the reduction of substance use. For example, Jason et al 35 conducted a randomized study to test the efficacy of an Oxford House intervention compared to usual care (ie, outpatient treatment or self-help groups) following discharge from inpatient substance abuse treatment. Results demonstrated a significant increase in monthly income with a significant decrease in substance use and incarceration rates among those in the Oxford House condition compared with the usual-care condition.
Some of the most popular peer support groups held outside the formal treatment settings for addiction nationwide include 12-step programs such as AA, Narcotics Anonymous, and Cocaine Anonymous. Twelve-step is an intervention for drug abuse and addiction and can include dual recovery from substance abuse problems and co-occurring mental health disorders. Humphreys 36 found 12-step groups to be the most referred adjunct support for professionally treated substance abuse patients. Other studies have demonstrated the effectiveness of 12-step groups for the treatment of substance abuse following treatment, 37 – 39 and prior research of 12-step groups has shown reductions in alcohol and drug use. 40 – 42
AA has been shown to be a highly utilized intervention for individuals with alcohol problems. 43 – 45 Positive outcomes such as self-efficacy and healthy coping have been associated with AA affiliation, which has been linked to better outcomes. 37 , 46 For those with drinking problems seen in treatment, certain AA activities such as having a sponsor and doing service might be key components of abstinence. 47
In a focused review of the literature on AA effectiveness, six criteria were required for establishing causation: 1) magnitude of effect; 2) dose–response effect; 3) consistent effect; 4) temporally accurate effects; 5) specific effects, and 6) plausibility. The evidence for all criteria except specific effects was very strong. For magnitude, rates of abstinence within AA were approximately twice as high. For dose–response, higher rates of abstinence were related to higher levels of attendance. For consistency, the effects were found for different follow-up periods and different samples. For temporal, prior AA attendance is predictive of subsequent abstinence. For plausibility, mechanisms of action predicted by behavioral change theories were present in AA. However, for specificity of an effect for 12-step facilitation or AA, experimental evidence was mixed, with evidence for both positive and negative effects in addition to no effect. 48
Although the peer support groups within 12-step approaches have provided benefits to select populations, some individuals with substance use disorders find the religious nature of 12-step approaches and often lack of integration in the treatment setting to be a deterrent. 49 – 51 Alternatives to 12-step approaches are needed to more closely integrate peer support services within treatment and to provide more options to benefit from peer support groups.
Treatment and community settings
Recently, there has been a dramatic rise in the adoption of alternative forms of peer support services within treatment and community settings to assist recovery from substance use disorders, because of the potential benefits offered to patients. 52 However, often peer support has not been separated out as a formalized intervention component and rigorously empirically tested, making it difficult to determine its effects. 53
Peer support is delivered in a variety of modalities, including, but not limited to, in-person self-help groups, Internet support groups, peer run or operated services, peer partnerships, peers in health care settings who serve as peer advocates, peer specialists, and peer case managers. 54 Among peer support services available today, peer support groups are considered an important aspect of the addiction recovery process. 55 – 58
Previous studies have shown positive outcomes from participating in peer support groups. Active engagement in peer support groups has shown to be a key predictor of recovery, 56 , 59 , 60 and sustaining recovery. 61 – 63 In addition, evidence demonstrates that one’s belief in their own ability can increase and influence one’s behavior by watching other peoples’ behaviors (ie, performing activities). 64 There is a mutual benefit between the members and facilitators of peer support groups. Oftentimes, peer support groups are facilitated by peer workers who themselves are in recovery and benefit positively from peer support groups. 21 Benefits for the peer worker include increased self-esteem, confidence, positive feelings of accomplishment, and an increase in their own ability to cope with their challenges.
Existing systematic peer support reviews
Bassuk et al 65 conducted a systematic review of the evidence on the effectiveness of peer support services for people in recovery from alcohol and drug addiction, which resulted in nine studies meeting the criteria for inclusion in the review. Despite methodological limitations found in the studies, the body of evidence suggested beneficial effects on participants. In another systematic review, Reif et al 66 evaluated peer support services for individuals with substance use disorders resulting in ten studies. The studies demonstrated increased treatment retention, improved relationships with treatment providers and social supports, increased satisfaction, and reduced relapse rates. Similar to the other reviews, there were methodological limitations that included inability to distinguish the effects of peer recovery support from other recovery support activities, small sample sizes and heterogeneous populations, unclear or inconsistent outcomes, and lack of any or appropriate comparison groups. Both of these reviews included peer support services in general without a specific focus on peer support groups and excluded studies with substance-using populations with a primary focus on human immunodeficiency virus (HIV)/hepatitis C virus (HCV) risk behavior outcomes. In addition, 12-step peer support studies were excluded.
This article reports the results of a literature review that was undertaken to assess the use of peer support groups, one aspect of peer recovery support services, in the treatment of addiction. In reporting the outcomes related to this review, the authors intend to: 1) encourage the field to generate further research to more rigorously investigate the effectiveness of peer support groups and explore the multitude of other specific types of peer recovery support services and 2) provide greater awareness to the advantages of peer support integration within the substance use treatment continuum for adults with addiction problems.
To effectively complete the review, the authors used a combination of searches on electronic scientific databases and screening results cross-checking the eligibility criteria to reduce the number of studies included in this article. At certain points, the authors independently cross-checked the results. If there was a discrepancy, further information was gathered to make an accurate determination of how to proceed. The process is described later and summarized in Figure 1 .

Flow diagram of study selection.
Study identification and screening: Phase I
The authors of this article searched the electronic databases of relevant peer-reviewed research literature including PubMed and MedLINE. Because addiction is a broad term that can be applied to varying types of addiction beyond alcohol- and nonalcohol-related substances (eg, gambling, Internet, sex, and eating) that are unrelated to the scope of this article, “substance use disorders” was the primary terminology used in searches to yield records pertaining to alcohol and drug problems. The initial database search used keywords “substance use disorders and peer support”. We also cross-checked our inclusion list by running similar searches containing specific substance names as keywords (eg, cocaine, alcohol, and heroin) to ensure comprehensiveness. This resulted in 2,291 records.
Study identification and screening: Phase II
The following keywords were used to identify all articles associated with several domains: substance use disorders, peer support or peer mentorship, and intervention. Including the keyword “intervention” allowed for higher yielding of treatment studies. While critiquing and critically reviewing results within an article that included a systematic review of studies, 66 we found three additional studies that met our inclusion criteria, which were included. 67 – 69 Using the keywords “substance use disorders and peer support and intervention”, 461 records were found. Using the keyword “substance use disorder and peer mentorship”, 24 records were found. Including three studies previously mentioned, a total of 488 articles were screened for eligibility.
Initial eligibility
By design, this discussion is limited to studies that included a peer support group component that: 1) had adult participants; 2) focused on addiction-related substance use (ie, alcohol, tobacco, legal/illicit drugs, and prescription drugs); 3) held in any group format; 4) included randomized controlled trials (RCTs) or studies with pre- and post-data results, and 5) US-conducted studies published in 1999 or later. Since certain groups (eg, HIV, HCV, and mental health) are at greater risk of having a substance use disorder, we did not exclude these populations.
As previously noted, the authors used keywords peer support or mentorship and substance use disorders to generate articles on the use of peer support groups within substance use disorder treatment to generate the initial pool of articles. We further narrowed our initial results in the current article to include only studies that focused on peer support group treatments. However, initially, we found that empirical studies assessing peer support groups solely were very limited and that our literature search would be much improved if we included not only peer support groups independently but also studies that integrated peer support groups as a component of a larger spectrum of peer services offered. We also included traditional forms of peer support services such as 12-step in addition to including any recent advancements within the field.
All study types that were not RCTs or quasi-experiments were excluded, including case reports, case series, cross-sectional surveys, and other qualitative studies. Adolescents-focused studies were excluded, because they focused generally on social support and social norms and peers may not have self-identified as having substance use problems. Cost-effectiveness studies were excluded. Article types such as books, editorials, guidelines, commentaries, dissertations, discussions, policy analyses, and newspaper or magazine articles were excluded. Of the 488 records that underwent review to meet the authors’ inclusion/exclusion criteria noted earlier, 16 articles met the initial eligibility.
Final selection
Of the 16 records, ten articles were selected to be included in the article. Of the six excluded, three studies had a primary focus of peer support groups to train the peer support staff, two studies did not have consistent or adequately structured peer support groups in the design, and one study’s substance use inclusion criteria were too minimal.
The literature search revealed articles that support the use of peer support services that include peer support groups within addiction treatment to address: 1) substance use, 2) treatment engagement, 3) HIV/HCV risk behaviors, and 4) secondary substance-related behaviors. It should be noted, however, that data were limited in finding peer support groups that were a standalone treatment as these groups were largely incorporated into a full array of peer support services being delivered, thereby posing challenges in disentangling the effects. Table 2 provides summaries of each study selected.
Included studies utilizing peer support groups
| Authors | Design | N | Population | Findings |
|---|---|---|---|---|
| Armitage et al | Pre/posttest | 152 | Individuals in recovery from addiction and their families | 86% of participants indicated no use of alcohol or drugs in the past 30 days at the 6-month follow-up 95% of participants reported strong willingness to recommend the program to others, 89% found services helpful, and 92% found materials helpful |
| Boisvert et al | Pre-/posttest | 18 | Individuals in addiction recovery living in permanent supportive housing | Substance use relapse rate reduced (24%–7%) for participants in the peer support community Pretest relapse rate was 85%; posttest rate was 33% for tenants returning to homelessness No differences in pre- and post-QOLR The MOS–SSS subscales revealed significant differences and moderate-to-large effect sizes ( ) on the MOS–SSS subscales: emotional/informational support ( =0.005; =0.628), tangible support ( =0.028; =0.493), and affectionate support ( =0.027; =0.494) |
| Tracy et al | Pre-/posttest | 40 | Individuals with substance use disorders in an addiction treatment program | Feasibility and acceptance data in the domains of patient interest, safety, and satisfaction were promising In addition, mentees significantly reduced their alcohol use ( <0.01) and drug use ( <0.01) from baseline to termination The majority of mentors sustained abstinence Fidelity measures indicated that mentors adhered to the delivery of treatment |
| Tracy et al | RCT comparing TAU + MAP-engage vs TAU + DRT + MAP-engage vs TAU | 96 | High recidivism veterans (mostly males) with substance use disorders initially recruited from an inpatient clinic | TAU + MAP-engage alone and TAU + DRT + MAP-engage were associated with increased adherence to post-discharge outpatient appointments for substance use treatment ( <0.05) when compared with TAU only As well as for substance use treatment, general medical, and mental health services ( <0.05 for all appointments combined) when compared with TAU only |
| Mangrum | Quasi-experimental design comparing ATR and substance use treatment vs substance use treatment | 4,420 | Consumers with substance use disorders referred from drug courts, probation, or child protective services | Individuals who completed the program were significantly more likely to have received recovery support groups ( (1)=65.75, <0.0001) |
| Purcell et al | RCT study of peer-mentoring intervention INSPIRE vs a video discussion control group | 966 | HIV-positive IDU participants | Adherence rates measured at 87%, 83%, and 85% at 3 months, 6 months, and 12 months, respectively Risk behaviors decreased among randomized participants although no significant differences in conditions |
| Latka et al | RCT study of peer-mentoring intervention vs a time-equivalent attention-control group | 418 | Individuals who are HCV-positive and IDUs | Compared with the controls, participants in the intervention group were less likely to report distributive risk behaviors at 3 months (OR =0.46; 95% CI =0.27, 0.79) and 6 months (OR =0.51; 95% CI =0.31, 0.83), a 26% relative risk reduction Peer mentoring and self-efficacy were significantly increased in the intervention group, and intervention effects were mediated through improved self-efficacy |
| Velasquez et al | RCT study of both individual counseling vs peer group education/support | 253 | HIV-positive men who have sex with men with alcohol use disorders | Treatment effect was demonstrated over each 30-day period with regard to number of drinks consumed (OR =1.38; 95% CI =1.02, 1.86) As well as the number of heavy drinking days (OR =1.5; 95% CI =1.08, 2.10) over each 30-day period Main effect was found in the number of days in which both heavy drinking and unprotected sex occurred over each 30-day period |
| Marlow et al | Pre-/posttest | 13 | Formerly incarcerated men on parole released from prison within the past 30 days | Findings from the assessment of psychosocial variables demonstrated significant improvement on two abstinence self-efficacy subscales, negative affect ( =0.01), and habitual craving ( =0.003) No significant differences in total scores for abstinence self-efficacy or the other measures from baseline to follow-up for the 13 participants who completed the study No significant differences in 12-step participation with regard to attendance, sponsor contact, or belief in 12-step framework |
| Andreas et al | Pre-/posttest | 509 | Men and women in recovery from addiction who had been incarcerated, and their families and significant others | Increased self-efficacy and increased family and friend support, quality of life, and feelings of guilt and shame were demonstrated at 12 months from baseline (no data were shown) Peer and staff accessibility were valued |
Abbreviations: ATR, access to recovery; CI, confidence interval; DRT, dual recovery treatment; HCV, hepatitis C virus; HIV, human immunodeficiency virus; IDU, injection drug user; INSPIRE, Intervention for Seropositive Injectors–Research and Evaluation; MAP, Mentorship for Alcohol Problem; MAP-engage, Mentorship for Addiction Problems to enhance engagement to treatment; MOS, Medical Outcomes Study; OR, odds ratio; QOLR, Quality of Life Rating; RCT, randomized controlled trial; SSS, Social Support Survey; TAU, treatment as usual.
Substance use
Armitage et al 67 discussed and evaluated Recovery Association Project’s (RAP) Recovery Community Services Program, a funded peer recovery service from 2003 to 2007. Recovery Community Services Program provided a wide range of peer recovery services, which included numerous self-help meetings at the RAP center that became a popular location for self-help meetings (eg, AA, Narcotics Anonymous, Cocaine Anonymous, and Smart Recovery) with several scheduled meetings daily. The outcomes measured were substance use, consumer satisfaction, and progress toward RAP’s goals. RAP received participant feedback from the Government Performance Reporting Act survey and a satisfaction questionnaire. There were 152 survey participants included in this outcome evaluation. At 6-month follow-up, most (86%) participants receiving RAP services indicated on the Government Performance Reporting Act survey abstinence from using alcohol or drugs in the past 30 days, which is much higher than typically noted abstinence levels in this population. These results help to demonstrate that RAP services are associated with sustained recovery from substance use. Data from the satisfaction questions administered at 6 months were also high, indicating RAP’s services are effectively meeting the needs of participants.
Boisvert et al 70 established and evaluated the effectiveness of a peer support community program. The primary purpose was to determine whether rates of relapse would decrease among addicts in recovery living in permanent supportive housing and increase their perceptions of community affiliation, supportive behaviors, self-determination (ie, proactive steps self-initiated to recovery), and quality of life. The peer support program was implemented by an occupational therapist and addiction professional following SAMHSA (Substance Abuse and Mental Health Services Administration) recovery community model. The staff person facilitated the first 10 weeks and then withdrew to a supportive background as the community became self-facilitating. Meetings involved discussions on principles of a peer support recovery or peer-driven community between the therapist and residents. Documents such as handouts and readings were provided to the community members who had interest in being a leader within the community, and supportive meetings were scheduled. The peer support group focused on training in leadership, group communication, and group facilitation with community-elected officers and conducted biweekly meetings and social events, all being organized by members.
Using previous year relapse data to provide a comparison rate, Boisvert et al 70 found significant reductions in relapse rates among participants in the peer support community programs. In addition, return to homelessness was dramatically reduced by assisting participants in managing their recovery. These results imply that peer and community support groups are important in the process of relapse reduction, in particular, groups that focus on self-determination, as it can have a positive impact on recovery from substance abuse and homelessness. As for the main objectives, quantitative findings showed that three subscales (ie, emotional support, tangible support, and affectionate support) on the Medical Outcomes Study–Social Support Survey demonstrated significant differences, although there were no significant differences regarding quality of life from the Quality of Life Rating. 70 In addition, qualitative findings showed that residents’ perceptions of community affiliation and supportive behaviors improved.
Another study conducted by Tracy et al 21 investigated a new intervention, mentorship for alcohol problems (MAPs), that included peer support groups and one-to-one mentorship services for individuals with alcohol-use disorders in community-treatment programs. Mentors participated for 6 months until multiple mentees received MAP for 12 weeks. Behavioral and biological measures were conducted in addition to fidelity measures. Feasibility and acceptance data in the domains of patient interest, safety, and satisfaction were promising. In addition, mentees significantly reduced their alcohol and drug use from baseline to termination and the majority of mentors sustained abstinence. Fidelity measures indicated that mentors adhered to the delivery of treatment.
Velasquez et al 71 evaluated the efficacy of a theory-based behavioral intervention that included both individual counseling and peer group education/support to reduce alcohol use among HIV-positive men who have sex with men when compared to a control condition where participants received resource materials. Reported treatment effects occurred in reduction in the number of drinks per 30-day period and number of days drank heavily per 30-day period.
Engagement to treatment
Beyond associated reductions in alcohol and drug use, services that have included peer support groups have been utilized to engage substance-using populations in treatment. Often high recidivism substance-using patients have difficulty connecting to outpatient treatment, contributing to greater functioning disturbances. 72 Approaches to address this problem frequently are staff extensive. Tracy et al 72 evaluated the impact of peer mentorship, which included, in addition to other peer support services, peer support groups and/or enhanced dual recovery treatment (DRT) on individuals who were inpatients, substance abusing, and had a history of high recidivism. The primary outcome was post-discharge treatment attendance. Within an inpatient Veterans Administration hospital setting, 96 patients with a history of high recidivism and current and/or past diagnosis of substance use disorders were randomized to either: 1) treatment as usual (TAU), 2) TAU + DRT + mentorship for addiction problems to enhance engagement to treatment (MAP-engage), or 3) TAU + MAP-engage. The investigators found that overall MAP-engage was comparable to the DRT + MAP-engage, and both of these conditions were significantly better than TAU alone at increasing adherence to post-discharge substance abuse, and medical and mental health outpatient appointments with participants in MAP-engage being three times as likely to attend their outpatient substance abuse treatment appointments than those in TAU 1 year post discharge. MAP-engage that included peer support groups offered an alternative approach to address lack of attendance to outpatient treatment appointments post discharge that is relatively low in staff reliance.
Similarly, in a large study, Mangrum 68 compared access to recovery + substance use treatment to substance use treatment alone for consumers involved in the criminal justice system who had substance use disorders and were referred from drug courts, probation, or child protective services. Individuals who completed the program were significantly more likely to have received recovery support groups. However, it should be noted that only a relatively small portion of the sample within the completers group, 12%, utilized the support groups as there were multiple treatment options, but this was still over twice as much as in the non-completers group, 5%.
HIV/HCV risk behavior
Intervention for Seropositive Injectors–Research and Evaluation study, an RCT of a peer support intervention designed to assess the reduction in sexual and injecting-related risk behaviors, increased use of HIV care, and increased HIV medication adherence as primary outcomes, was discussed by Purcell et al. 73 The peer support intervention was ten sessions over a 12-month time period, with seven sessions being specifically devoted to peer support groups. The control condition was eight sessions of a video intervention. One out of the ten sessions was a peer volunteer activity during which participants went to a local service organization for 2–4 hours to observe, participate, and practice peer support skills. The topics from the group sessions included setting group rules and the power of peer mentoring, utilization of HIV primary care and adherence, and sex and drug risk behaviors.
Of the participants randomized, 486 were assigned to the peer support condition and 480 were assigned to the video discussion condition, totaling a sample of 966 HIV injection drug users (IDUs). Purcell et al 73 found that randomized participants in both conditions had retention rates of 87%, 83%, and 85% at 3 months, 6 months, and 12 months, respectively. Significant reductions were noted in both groups for reductions from baseline in injection and sexual transmission risk behaviors, but there were no significant differences between conditions. Participants in both conditions reported no change in medical care and adherence. 73
An RCT with a time-equivalent attention-control group was conducted by Latka et al 74 among 418 HCV IDUs to examine a peer-mentoring behavioral intervention to reduce the distribution of injection practices and equipment among HCV IDUs. Each intervention consisted of six sessions, 2 hours each twice a week. For the peer-mentoring group intervention, participants received information regarding HCV and learned risk reduction skills. By the fifth session, training participants were involved in outreach and delivered information about reducing HCV transmission risk. The control group watched a docudrama TV series about IDUs and participated in a facilitated group discussion focusing on family, education, self-respect, relationships, violence, parenting, and employment. Compared to the control group, participants in the peer support condition had significantly greater reductions in injection practices that could transmit HCV to other IDUs. Self-efficacy was significantly increased in the experimental condition, and post-intervention self-efficacy was a positive mediator between the intervention and distributive risk behaviors.
In the study previously discussed in the substance use section, Velasquez et al 71 also found a reduction in the number of days on which both heavy drinking and unprotected sex occurred among HIV-positive men who have sex with men.
Secondary substance-related outcomes
Craving has been associated with use of substances. 75 – 78 The authors’ search also revealed a recently published pilot study that evaluated a peer support program for formerly incarcerated adults who transitioned back into the community that included investigations of craving among other varriables. 79 This population experiences high rates of substance use. One of the main objectives of this study was to assess program feasibility using a community-based participatory research approach. Participants were 20 men on parole who were released from prison within the past 30 days, with only 13 completing the 60-day peer mentor intervention. Marlow et al 78 measured 12-step meeting participation using a 13-item questionnaire that assessed participation in 12-step programs, belief in the 12-step framework, and investigated relationships with craving and negative affect. Questions assessing belief in 12-step framework included: I am powerless over my drug and alcohol problem, I believe a higher power plays a role in my recovery, I am not alone with my drug and alcohol problem, I believe in the 12-step faith and spirituality, and I am member of 12-step. Twelve-step meetings were attended by participants on an average of 17 days out of 30 days and participants contacted their sponsor on average ten times. All participants’ belief in the 12-step framework was high. Pre- and posttest results on two abstinence subscales, negative affect and habitual craving, showed significant improvement, indicating an improved confidence level in the ability to abstain from substance use.
Andreas et al 69 sought to examine Peers Reach Out Supporting Peers to Embrace Recovery (PROSPER), a peer-driven recovery community that provides a number of peer-driven supports for members to be able to recover from drug use and criminality as they transition back into the community and to provide support to their family members and loved ones. PROSPER provided a strategic mix of services, all planned, implemented, and delivered by peers including peer-run groups and group activities that take place in a light-hearted social environment away from traditional treatment settings. The aims of the program were to: 1) provide peer support environment, 2) build positive self-concept and achievement motivation, 3) reinforce family/significant others’ relationships and support, and 4) amplify the treatment continuum. 77 The study outcome measures were self-efficacy, perceived social support, personal feeling, perceived stress, and quality of life. Program effects were evaluated and demonstrated at 12 months from baseline with significant and positive changes in participants’ self-efficacy, social support perceptions, quality of life, and feelings of guilt and shame over a 12-month period. The result of this study suggests the importance of peer support among people who are reentering the community, which can promote positive outcomes such as reduced substance use and recidivism.
Despite the recent surge in the adoption of peer support services within addiction treatment systems, there are relatively limited data rigorously evaluating outcomes. 21 These data become even more limited when considering one form of peer support services, such as peer support groups as in the case of this review, due to the nature of peer support services being delivered often in a multitude of combined modalities. Thus, we included studies of peer support groups that were delivered often in an array of other peer support treatments, which diminished our ability to disentangle the results. However, this review still provides a useful platform to begin to explore the inclusion of these peer support groups as a component of other peer services and associated benefits thus far to guide the field in the future researching of this area.
Although methodological limitations existed in studies that resulted from previous existing systematic reviews of peer support services, beneficial effects were noted. 65 , 66 This article builds upon these reviews by the specificity on peer support groups, which is a common platform in treatment. To the authors’ knowledge, this is the first article to date to take such an approach reviewing controlled studies. The previous reviews examined a range of peer support services. Moreover, we expanded beyond existing reviews to include substance-related HIV/HCV risk behavior studies due to the high prevalence of substance use disorders in this population. Drug abuse is inextricably linked with HIV due to heightened risk both of contracting HIV and of worsening its consequences, and HCV is one of the most common viral hepatitis infections transmitted through drug-using high-risk behaviors, making reduction of risk behaviors one of the priorities in substance abuse treatment at the National Institute on Drug Abuse. 80 Finally, we also expanded our review to include 12-step studies due to their focus on peer support groups and contributions to the peer support movement.
Our review revealed articles that demonstrated peer support services that include groups delivered to those with substance use problems showing associated benefits in the following areas: 1) substance use, 2) treatment engagement, 3) HIV/HCV risk behaviors, and 4) secondary substance-related behaviors such as craving and self-efficacy.
Those who participated in treatments, including peer support groups, showed higher rates of abstinence than common in substance-abusing populations while also being more satisfied with the treatment. 67 Furthermore, significant reductions in relapse rates were shown in addition to significant reductions in return to homelessness in a challenging population to treat. 70 Reported benefits extended beyond those being the recipient of the peer support groups to those also delivering the services, where significant reductions in alcohol and drug use were shown not only for mentees but also for sustained abstinence in the majority of mentors. 21
Beyond substance use, peer support groups offer unique advantages to engaging our historically difficult-to-engage populations. Services that included peer support groups were found to be equally comparable to the additive of extensive DRT, and both were significantly better than standard treatment at increasing adherence to post-discharge substance abuse and medical and mental health outpatient appointments for high recidivism individuals with substance use disorders. 72 Moreover, consumers involved in the criminal justice system who had substance use disorders and were referred from drug courts, probation, or child protective services, who completed the program, were significantly more likely to have received recovery support groups. 68 However, it should be noted that only a relatively small sample completed, thus diminishing the impact of these results.
Peer support services that include groups have also been associated with reductions in HIV and HCV risk behaviors in IDUs. One study demonstrated a reduction in injection and sexually transmitted risk behaviors in both conditions, but there was no significant difference between the peer condition and the control condition, which was also an intervention. 73 However, another study showed not just a reduction but significantly greater reductions in injection practices that could transmit HCV to other IDUs when comparing the peer support condition to the control group. 74 Consistent with previous research, the study suggests that this enhanced behavioral intervention of education and counseling was associated with safer injection practices. Thus, providing implications that these components (ie, skill building and education) of peer mentoring provided to HCV-injecting drug users can lead to safer practices of injection drug use and may contribute to reducing the risk in IDUs and the transmission of HCV to other IDUs. Another study demonstrated significant reductions not only in risk behaviors but also in heavy drinking while accomplishing this. 71
One of the key elements that peer support services significantly positively impact is improvement in participants’ self-efficacy, which was also found to be a positive mediator between interventions and distributive risk behaviors in one study. 69 Associated positive changes have also been demonstrated such as improvements in negative affect, social support perceptions, reductions in habitual craving, and feelings of guilt or shame. 69 , 79 All of these areas play important roles in one’s ability to achieve and sustain abstinence from substances. There were conflicting results from studies on whether or not quality-of-life improvements were associated with peer support groups being included in services. 69 , 70
Peer support groups included in addiction treatment show much promise in potentially reducing substance use, improving engagement, reducing HIV/HCV risk behaviors, and improving substance-related outcomes. However, even given their widespread use, there are relatively limited empirical data relevant to this topic, which may diminish the ability to draw definitive conclusions, with resulting studies being ten. Although this is similar in number to other reviews in related peer support topics, it is relatively low. We included only US studies due to not having access to other non-English search engines in addition to ruling out language barriers, but this also limits the data. Finally, some investigators note that self-selection into peer support groups and residential recovery homes is important in the process in treatment, 33 , 81 which then may confound outcomes and limit generalizability in RCTs for those select participants who may be solely interested in gains outside of participation such as participant payment. More rigorous research is needed, including meta-analytic studies as more data surface in this area, to substantiate the results of the studies included in this review and further expand on this important line of research.
Acknowledgments
This work was supported by the National Institute on Drug Abuse (R34DA034898) and the New York Harbor Healthcare System.
The authors report no conflicts of interest in this work.

Brill | Nijhoff
Brill | Wageningen Academic
Brill Germany / Austria
Böhlau
Brill | Fink
Brill | mentis
Brill | Schöningh
Vandenhoeck & Ruprecht
V&R unipress
Open Access
Open Access for Authors
Transformative Agreements
Open Access and Research Funding
Open Access for Librarians
Open Access for Academic Societies
Discover Brill’s Open Access Content
Organization
Stay updated
Corporate Social Responsiblity
Investor Relations
Policies, rights & permissions
Review a Brill Book
Author Portal
How to publish with Brill: Files & Guides
Fonts, Scripts and Unicode
Publication Ethics & COPE Compliance
Data Sharing Policy
Brill MyBook
Ordering from Brill
Author Newsletter
Piracy Reporting Form
Sales Managers and Sales Contacts
Ordering From Brill
Titles No Longer Published by Brill
Catalogs, Flyers and Price Lists
E-Book Collections Title Lists and MARC Records
How to Manage your Online Holdings
LibLynx Access Management
Discovery Services
KBART Files
MARC Records
Online User and Order Help
Rights and Permissions
Latest Key Figures
Latest Financial Press Releases and Reports
Annual General Meeting of Shareholders
Share Information
Specialty Products
Press and Reviews
Self-Help/Mutual Aid Groups and Peer Support
A literature review, series: brill research perspectives in humanities and social sciences , volume: 23 voluntaristics review , volume: 23.
Prices from (excl. shipping):
- Paperback: €74.00
- E-Book (PDF): €74.00
- View PDF Flyer
Copyright page
Biographical note, table of contents, share link with colleague or librarian, product details.
- North America
- Social History
- Sociology & Anthropology
- Social Work & Social Policy
- Global Studies
Related Content
Reference Works
Primary source collections
COVID-19 Collection
How to publish with Brill
Open Access Content
Contact & Info
Sales contacts
Publishing contacts
Stay Updated
Newsletters
Social Media Overview
Terms and Conditions
Privacy Statement
Cookie Settings
Accessibility
Legal Notice
Terms and Conditions | Privacy Statement | Cookie Settings | Accessibility | Legal Notice | Copyright © 2016-2024
Copyright © 2016-2024
- [195.190.12.77]
- 195.190.12.77
Character limit 500 /500
Europe PMC requires Javascript to function effectively.
Either your web browser doesn't support Javascript or it is currently turned off. In the latter case, please turn on Javascript support in your web browser and reload this page.
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
- My Bibliography
- Collections
- Citation manager
Save citation to file
Email citation, add to collections.
- Create a new collection
- Add to an existing collection
Add to My Bibliography
Your saved search, create a file for external citation management software, your rss feed.
- Search in PubMed
- Search in NLM Catalog
- Add to Search
Peer Support Interventions for People With CKD: A Scoping Review
Affiliations.
- 1 Department of Medicine, University of Calgary, Calgary, Alberta, Canada; Department of Community Health Sciences, University of Calgary, Calgary, Alberta, Canada; O'Brien Institute for Public Health, Cumming School of Medicine, University of Calgary, Calgary, Alberta, Canada. Electronic address: [email protected].
- 2 Department of Medicine, University of Calgary, Calgary, Alberta, Canada; Department of Community Health Sciences, University of Calgary, Calgary, Alberta, Canada; O'Brien Institute for Public Health, Cumming School of Medicine, University of Calgary, Calgary, Alberta, Canada; Libin Cardiovascular Institute, Cumming School of Medicine, University of Calgary, Calgary, Alberta, Canada.
- 3 Department of Medicine, University of Calgary, Calgary, Alberta, Canada.
- 4 Department of Community Health Sciences, University of Calgary, Calgary, Alberta, Canada; O'Brien Institute for Public Health, Cumming School of Medicine, University of Calgary, Calgary, Alberta, Canada.
- 5 Patient Partner, Can-SOLVE CKD Network, Canada.
- 6 Faculty of Medicine and Dentistry, University of Alberta, Edmonton, Alberta, Canada.
- 7 Department of Community Health Sciences, University of Calgary, Calgary, Alberta, Canada.
- PMID: 39154886
- DOI: 10.1053/j.ajkd.2024.07.007
Rationale & objective: Formalized peer support is a promising approach for addressing the emotional and practical needs of people living with chronic kidney disease (CKD). We aimed to systematically identify and summarize peer support interventions studied in individuals with CKD with or without kidney replacement therapy (KRT).
Sources of evidence: We searched electronic databases and grey literature sources in March 2023.
Eligibility criteria: Studies of any design were eligible if they reported sufficient detail on peer support interventions and outcomes for adults with CKD with or without KRT and/or their caregivers.
Charting methods: We extracted information on study and intervention characteristics and reported outcomes using established frameworks. We summarized quantitative data descriptively and qualitative data thematically. Our approach observed the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) extension for scoping reviews.
Results: We included 77 studies describing 56 unique peer support interventions. Most reports were program evaluations (39%) or randomized controlled trials (27%) published after 2013. Two thirds of interventions focused on in-centre hemodialysis or mixed CKD populations, and three quarters were integrated within a kidney care clinic or program. Whereas most peer interactions centered on informational support, few programs offered focused support in areas such as transplant navigation or dialysis modality selection. Only one third of outcomes were assessed against a comparator group, with results suggesting improvements in psychological health with peer support.
Limitations: Heterogeneity of included studies; lack of rigorous program evaluation.
Conclusions: This review suggests recent growth in peer support programming with a variety of formats and delivery methods to address the diverse needs of people living with kidney disease. Notable gaps in peer support availability for transplant and home dialysis recipients and the lack of rigorous evaluations present opportunities to expand the reach and impact of peer support in the kidney care context.
Keywords: dialysis; kidney disease; peer mentorship; peer support; scoping review; transplant.
Copyright © 2024. Published by Elsevier Inc.
PubMed Disclaimer
Similar articles
- Folic acid supplementation and malaria susceptibility and severity among people taking antifolate antimalarial drugs in endemic areas. Crider K, Williams J, Qi YP, Gutman J, Yeung L, Mai C, Finkelstain J, Mehta S, Pons-Duran C, Menéndez C, Moraleda C, Rogers L, Daniels K, Green P. Crider K, et al. Cochrane Database Syst Rev. 2022 Feb 1;2(2022):CD014217. doi: 10.1002/14651858.CD014217. Cochrane Database Syst Rev. 2022. PMID: 36321557 Free PMC article.
- Beyond the black stump: rapid reviews of health research issues affecting regional, rural and remote Australia. Osborne SR, Alston LV, Bolton KA, Whelan J, Reeve E, Wong Shee A, Browne J, Walker T, Versace VL, Allender S, Nichols M, Backholer K, Goodwin N, Lewis S, Dalton H, Prael G, Curtin M, Brooks R, Verdon S, Crockett J, Hodgins G, Walsh S, Lyle DM, Thompson SC, Browne LJ, Knight S, Pit SW, Jones M, Gillam MH, Leach MJ, Gonzalez-Chica DA, Muyambi K, Eshetie T, Tran K, May E, Lieschke G, Parker V, Smith A, Hayes C, Dunlop AJ, Rajappa H, White R, Oakley P, Holliday S. Osborne SR, et al. Med J Aust. 2020 Dec;213 Suppl 11:S3-S32.e1. doi: 10.5694/mja2.50881. Med J Aust. 2020. PMID: 33314144
- Outpatient Interventions for Managing Acute Complications of Chronic Diseases: A Scoping Review and Implications for Patients With CKD. Elliott MJ, Love S, Donald M, Manns B, Donald T, Premji Z, Hemmelgarn BR, Grinman M, Lang E, Ronksley PE. Elliott MJ, et al. Am J Kidney Dis. 2020 Dec;76(6):794-805. doi: 10.1053/j.ajkd.2020.04.006. Epub 2020 May 30. Am J Kidney Dis. 2020. PMID: 32479925 Review.
- Recovery schools for improving behavioral and academic outcomes among students in recovery from substance use disorders: a systematic review. Hennessy EA, Tanner-Smith EE, Finch AJ, Sathe N, Kugley S. Hennessy EA, et al. Campbell Syst Rev. 2018 Oct 4;14(1):1-86. doi: 10.4073/csr.2018.9. eCollection 2018. Campbell Syst Rev. 2018. PMID: 37131375 Free PMC article.
- Web-Based Peer Support Interventions for Adults Living With Chronic Conditions: Scoping Review. Hossain SN, Jaglal SB, Shepherd J, Perrier L, Tomasone JR, Sweet SN, Luong D, Allin S, Nelson MLA, Guilcher SJT, Munce SEP. Hossain SN, et al. JMIR Rehabil Assist Technol. 2021 May 25;8(2):e14321. doi: 10.2196/14321. JMIR Rehabil Assist Technol. 2021. PMID: 34032572 Free PMC article. Review.
Related information
Linkout - more resources, full text sources.
- Elsevier Science
Research Materials
- NCI CPTC Antibody Characterization Program
- Citation Manager
NCBI Literature Resources
MeSH PMC Bookshelf Disclaimer
The PubMed wordmark and PubMed logo are registered trademarks of the U.S. Department of Health and Human Services (HHS). Unauthorized use of these marks is strictly prohibited.
Information
- Author Services
Initiatives
You are accessing a machine-readable page. In order to be human-readable, please install an RSS reader.
All articles published by MDPI are made immediately available worldwide under an open access license. No special permission is required to reuse all or part of the article published by MDPI, including figures and tables. For articles published under an open access Creative Common CC BY license, any part of the article may be reused without permission provided that the original article is clearly cited. For more information, please refer to https://www.mdpi.com/openaccess .
Feature papers represent the most advanced research with significant potential for high impact in the field. A Feature Paper should be a substantial original Article that involves several techniques or approaches, provides an outlook for future research directions and describes possible research applications.
Feature papers are submitted upon individual invitation or recommendation by the scientific editors and must receive positive feedback from the reviewers.
Editor’s Choice articles are based on recommendations by the scientific editors of MDPI journals from around the world. Editors select a small number of articles recently published in the journal that they believe will be particularly interesting to readers, or important in the respective research area. The aim is to provide a snapshot of some of the most exciting work published in the various research areas of the journal.
Original Submission Date Received: .
- Active Journals
- Find a Journal
- Proceedings Series
- For Authors
- For Reviewers
- For Editors
- For Librarians
- For Publishers
- For Societies
- For Conference Organizers
- Open Access Policy
- Institutional Open Access Program
- Special Issues Guidelines
- Editorial Process
- Research and Publication Ethics
- Article Processing Charges
- Testimonials
- Preprints.org
- SciProfiles
- Encyclopedia

Article Menu

- Subscribe SciFeed
- Author Biographies
- Google Scholar
- on Google Scholar
- Table of Contents
Find support for a specific problem in the support section of our website.
Please let us know what you think of our products and services.
Visit our dedicated information section to learn more about MDPI.
JSmol Viewer
Dexmedetomidine as adjunctive therapy for the treatment of alcohol withdrawal syndrome: a systematic review and meta-analysis.

1. Introduction
2.1. primary outcome (tracheal intubation), 2.2. secondary outcome (bradycardia), 2.3. secondary outcome (hypotension), 3. discussion, 4.1. study search, 4.2. study selection, 4.3. definition and outcome, 4.4. data extraction and quality assessment, 4.5. data analysis, 5. conclusions, author contributions, data availability statement, acknowledgments, conflicts of interest.
- Association, A.P. Diagnostic and Statistical Manual of Mental Disorders , 5th ed.; American Psychiatric Association: Arlington, VA, USA, 2000. [ Google Scholar ] [ CrossRef ]
- Ganatra, R.B.; Breu, A.C.; Ronan, M.V. Clinical guideline highlights for the hospitalist: 2020 American Society of Addiction Medicine clinical practice guideline on alcohol withdrawal management. J. Hosp. Med. 2022 , 17 , 47–49. [ Google Scholar ] [ CrossRef ]
- Weerink, M.A.S.; Struys, M.M.R.F.; Hannivoort, L.N.; Barends, C.R.M.; Absalom, A.R.; Colin, P. Clinical Pharmacokinetics and Pharmacodynamics of Dexmedetomidine. Clin. Pharmacokinet. 2017 , 56 , 893–913. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Yuki, K. The immunomodulatory mechanism of dexmedetomidine. Int. Immunopharmacol. 2021 , 97 , 107709. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- U.S. Department of Health and Human Services (HHS); Substance Abuse and Mental Health Services Administration (SAMHSA); Center for Behavioral Health Statistics and Quality; Treatment Services Branch. Preliminary Findings from Drug-Related Emergency Department Visits. 2021. Available online: https://store.samhsa.gov/sites/default/files/PEP22-07-03-001.pdf (accessed on 16 April 2024).
- Peterson, C.; Li, M.; Xu, L.; Mikosz, C.A.; Luo, F. Assessment of Annual Cost of Substance Use Disorder in US Hospitals. JAMA Netw. Open 2021 , 4 , e210242. [ Google Scholar ] [ CrossRef ]
- Chang, D.W.; Shapiro, M.F. Association between Intensive Care Unit Utilization during Hospitalization and Costs, Use of Invasive Procedures, and Mortality. JAMA Intern. Med. 2016 , 176 , 1492–1499. [ Google Scholar ] [ CrossRef ]
- Harrer, M.; Cuijpers, P.; Furukawa, T.A.; Ebert, D.D. Doing Meta-Analysis with R: A Hands-On Guide , 1st ed.; Chapman & Hall/CRC Press: Boca Raton, FL, USA; London, UK, 2021. [ Google Scholar ]
- Crispo, A.L.; Daley, M.J.; Pepin, J.L.; Harford, P.H.; Brown, C.V. Comparison of clinical outcomes in nonintubated patients with severe alcohol withdrawal syndrome treated with continuous-infusion sedatives: Dexmedetomidine versus benzodiazepines. Pharmacotherapy 2014 , 34 , 910–917. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Bielka, K.; Kuchyn, I.; Glumcher, F. Addition of dexmedetomidine to benzodiazepines for patients with alcohol withdrawal syndrome in the intensive care unit: A randomized controlled study. Ann. Intensive Care 2015 , 5 , 33. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- VanderWeide, L.A.; Foster, C.J.; MacLaren, R.; Kiser, T.H.; Fish, D.N.; Mueller, S.W. Evaluation of Early Dexmedetomidine Addition to the Standard of Care for Severe Alcohol Withdrawal in the ICU:A Retrospective Controlled Cohort Study. J. Intensive Care Med. 2016 , 31 , 198–204. [ Google Scholar ] [ CrossRef ]
- Lizotte, R.J.; Kappes, J.A.; Bartel, B.J.; Hayes, K.M.; Lesselyoung, V.L. Evaluating the effects of dexmedetomidine compared to propofol as adjunctive therapy in patients with alcohol withdrawal. Clin. Pharmacol. 2014 , 6 , 171–177. [ Google Scholar ] [ CrossRef ]
- Love, K.; Zimmermann, A.E. Use of Propofol Plus Dexmedetomidine in Patients Experiencing Severe Alcohol Withdrawal in the Intensive Care Unit. J. Clin. Pharmacol. 2020 , 60 , 439–443. [ Google Scholar ] [ CrossRef ]
- Collier, T.E.; Farrell, L.B.; Killian, A.D.; Kataria, V.K. Effect of Adjunctive Dexmedetomidine in the Treatment of Alcohol Withdrawal Compared to Benzodiazepine Symptom-Triggered Therapy in Critically Ill Patients: The EvADE Study. J. Pharm. Pract. 2022 , 35 , 356–362. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Mueller, S.W.; Preslaski, C.R.; Kiser, T.H.; Fish, D.N.; Lavelle, J.C.; Malkoski, S.P.; MacLaren, R. A randomized, double-blind, placebo-controlled dose range study of dexmedetomidine as adjunctive therapy for alcohol withdrawal. Crit. Care Med. 2014 , 42 , 1131–1139. [ Google Scholar ] [ CrossRef ]
- Ludtke, K.A.; Stanley, K.S.; Yount, N.L.; Gerkin, R.D. Retrospective Review of Critically Ill Patients Experiencing Alcohol Withdrawal: Dexmedetomidine Versus Propofol and/or Lorazepam Continuous Infusions. Hosp. Pharm. 2015 , 50 , 208–213. [ Google Scholar ] [ CrossRef ]
- Wong, A.; Benedict, N.J.; Kane-Gill, S.L. Multicenter evaluation of pharmacologic management and outcomes associated with severe resistant alcohol withdrawal. J. Crit. Care 2015 , 30 , 405–409. [ Google Scholar ] [ CrossRef ]
- Riihioja, P.; Jaatinen, P.; Oksanen, H.; Haapalinna, A.; Heinonen, E.; Hervonen, A. Dexmedetomidine, diazepam, and propranolol in the treatment of ethanol withdrawal symptoms in the rat. Alcohol. Clin. Exp. Res. 1997 , 21 , 804–808. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Rovasalo, A.; Tohmo, H.; Aantaa, R.; Kettunen, E.; Palojoki, R. Dexmedetomidine as an adjuvant in the treatment of alcohol withdrawal delirium: A case report. Gen. Hosp. Psychiatry 2006 , 28 , 362–363. [ Google Scholar ] [ CrossRef ]
- DeMuro, J.P.; Botros, D.G.; Wirkowski, E.; Hanna, A.F. Use of dexmedetomidine for the treatment of alcohol withdrawal syndrome in critically ill patients: A retrospective case series. J. Anesth. 2012 , 26 , 601–605. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Rayner, S.G.; Weinert, C.R.; Peng, H.; Jepsen, S.; Broccard, A.F. Dexmedetomidine as adjunct treatment for severe alcohol withdrawal in the ICU. Ann. Intensive Care 2012 , 2 , 12. [ Google Scholar ] [ CrossRef ]
- Frazee, E.N.; Personett, H.A.; Leung, J.G.; Nelson, S.; Dierkhising, R.A.; Bauer, P.R. Influence of dexmedetomidine therapy on the management of severe alcohol withdrawal syndrome in critically ill patients. J. Crit. Care 2014 , 29 , 298–302. [ Google Scholar ] [ CrossRef ]
- Polintan, E.T.T.; Danganan, L.M.L.; Cruz, N.S.; Macapagal, S.C.; Catahay, J.A.; Patarroyo-Aponte, G.; Azmaiparashvili, Z.; Lo, K.B. Adjunctive Dexmedetomidine in Alcohol Withdrawal Syndrome: A Systematic Review and Meta-analysis of Retrospective Cohort Studies and Randomized Controlled Trials. Ann. Pharmacother. 2022 , 57 , 696–705. [ Google Scholar ] [ CrossRef ]
- Fiore, M.; Torretta, G.; Passavanti, M.B.; Sansone, P.; Pace, M.C.; Alfieri, A.; Aurilio, C.; Simeon, V.; Chiodini, P.; Pota, V. Dexmedetomidine as adjunctive therapy for the treatment of alcohol withdrawal syndrome: A systematic review protocol. JBI Database Syst. Rev. Implement. Rep. 2019 , 17 , 2159–2164. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. BMJ 2021 , 372 , n71. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Sterne, J.A.C.; Savović, J.; Page, M.J.; Elbers, R.G.; Blencowe, N.S.; Boutron, I.; Cates, C.J.; Cheng, H.-Y.; Corbett, M.S.; Eldridge, S.M.; et al. RoB 2: A revised tool for assessing risk of bias in randomised trials. BMJ 2019 , 366 , l4898. [ Google Scholar ] [ CrossRef ]
- Wells, G.A.; Shea, B.; O’Connell, D.; Peterson, J.; Welch, V.; Losos, M.; Tugwell, P. The Newcastle-Ottawa Scale (NOS) for Assessing the Quality of Nonrandomised Studies in Meta-Analyses ; Ottawa Hospital Research Institute: Ottawa, ON, USA, 2000. [ Google Scholar ]
- Mantel, N.; Haenszel, W. Statistical aspects of the analysis of data from retrospective studies of disease. J. Natl. Cancer Inst. 1959 , 22 , 719–748. [ Google Scholar ]
- Hedges, L.V.; Vevea, J.L. Estimating Effect Size under Publication Bias: Small Sample Properties and Robustness of a Random Effects Selection Model. J. Educ. Behav. Stat. 1996 , 21 , 299–332. [ Google Scholar ] [ CrossRef ]
- Paule, R.C.; Mandel, J. Consensus Values and Weighting Factors. J. Res. Natl. Bur. Stand. 1982 , 87 , 377–385. [ Google Scholar ] [ CrossRef ]
Click here to enlarge figure
| Author (Published Year) [Ref.] | Setting | Study Design | Control Group | Time Spam | N. Patients | Outcome(s) |
|---|---|---|---|---|---|---|
| Crispo, A.L. (2014) [ ] | ED | RC | BZD | 2011–2012 | 122 | TI + B + H |
| Bielka, K. (2015) [ ] | ED | RCT | BZD | NS | 134 | TI + B + H |
| VanderWeide, L.A. (2016) [ ] | Mixed | RC | BZD | 2008–2012 | 84 | TI + B + H |
| Lizotte, R.J. (2014) [ ] | ED | RC | BZD + P | 2010–2013 | 82 | TI + B + H |
| Love, K. (2020) [ ] | ICU | RC | BZD + P | 2015–2018 | 53 | TI + B + H |
| Collier, T.E. (2022) [ ] | ICU | RC | BZD | 2015–2018 | 110 | TI + B |
| Mueller, S. (2014) [ ] | ED | RCT | BZD | 2009–2012 | 48 | B + H |
| Ludtke, K.A. (2015) [ ] | ED | RC | BZD + P | 2002–2009 | 64 | TI |
| Wong, A. (2015) [ ] | Mixed | RC | BZD + P | 2009–2012 | 258 | TI |
| Study | Ref. | R | D | Mi | Me | S | O |
|---|---|---|---|---|---|---|---|
| Bielka, K. | [ ] | + | − | + | + | + | + |
| Mueller, S. | [ ] | + | + | − | + | + | + |
| Study | Ref. | Selection | Comparability | Outcome |
|---|---|---|---|---|
| Crispo, A.L. | [ ] | *** | * | *** |
| Lizotte, R.J. | [ ] | *** | ** | ** |
| VanderWeide, L.A. | [ ] | ** | * | ** |
| Ludtke, K.A. | [ ] | *** | * | *** |
| Wong, A. | [ ] | *** | ** | *** |
| Love, K. | [ ] | *** | ** | *** |
| Collier, T.E. | [ ] | *** | ** | ** |
| Participants | Intervention | Comparison | Outcomes | Study Design |
|---|---|---|---|---|
| Adult patients in any setting with alcohol withdrawal syndrome | Dexmedetomidine as adjunctive therapy to standard of care | Standard of care | Primary outcomes: Tracheal intubation Secondary outcomes: (a) Hypotension (b) Bradycardia | Randomized controlled trials and observational studies (including cohort and case-control studies) |
| The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
Share and Cite
Fiore, M.; Alfieri, A.; Torretta, G.; Passavanti, M.B.; Sansone, P.; Pota, V.; Simeon, V.; Chiodini, P.; Corrente, A.; Pace, M.C. Dexmedetomidine as Adjunctive Therapy for the Treatment of Alcohol Withdrawal Syndrome: A Systematic Review and Meta-Analysis. Pharmaceuticals 2024 , 17 , 1125. https://doi.org/10.3390/ph17091125
Fiore M, Alfieri A, Torretta G, Passavanti MB, Sansone P, Pota V, Simeon V, Chiodini P, Corrente A, Pace MC. Dexmedetomidine as Adjunctive Therapy for the Treatment of Alcohol Withdrawal Syndrome: A Systematic Review and Meta-Analysis. Pharmaceuticals . 2024; 17(9):1125. https://doi.org/10.3390/ph17091125
Fiore, Marco, Aniello Alfieri, Giacomo Torretta, Maria Beatrice Passavanti, Pasquale Sansone, Vincenzo Pota, Vittorio Simeon, Paolo Chiodini, Antonio Corrente, and Maria Caterina Pace. 2024. "Dexmedetomidine as Adjunctive Therapy for the Treatment of Alcohol Withdrawal Syndrome: A Systematic Review and Meta-Analysis" Pharmaceuticals 17, no. 9: 1125. https://doi.org/10.3390/ph17091125
Article Metrics
Article access statistics, further information, mdpi initiatives, follow mdpi.

Subscribe to receive issue release notifications and newsletters from MDPI journals

IMAGES
COMMENTS
Peer Support in Mental Health: Literature Review. Reham A Hameed Shalaby, Department of Psychiatry, University of Alberta, 1E1 Walter Mackenzie Health Sciences Centre, 8440 112 St NW, Edmonton, AB, T6G 2B7, Canada, Phone: 1 4034702050, Email: ac.atrebalau@ybalahsr.
Peer support in mental health has been variously defined in the literature and is simply known as the help and support that people with lived experience of mental illness or a learning disability can give to one another. Although PSSs date back to several centuries, it is only in the last few decades that these services have formally evolved ...
Peer support for mental health is recommended across international policy guidance and provision. Our systematic umbrella review summarises evidence on the effectiveness, implementation, and experiences of paid peer support approaches for mental health. We searched MEDLINE, EMBASE, PsycINFO, The Campbell Collaboration, and The Cochrane Database of Systematic Reviews (2012-2022) for reviews ...
Background: A growing gap has emerged between people with mental illness and health care professionals, which in recent years has been successfully closed through the adoption of peer support services (PSSs). Peer support in mental health has been variously defined in the literature and is simply known as the help and support that people with lived experience of mental illness or a learning ...
Aims: To review the published research literature relating to the process of peer support and its underpinning mechanisms to better understand how and why it works. Method: A scoping review of published literature identified studies relating to peer support mechanisms, processes and relationships. Studies were summarised and findings analysed.
The literature reports a wide variability of peer support activities provided [] and no generally agreed upon outcomes to measure [].Peer support is conceptualized and delivered in a wide range of formats [], including protocolized interventions delivered at least in part by a peer supporter [9, 10], traditional mental health services with at least one peer supporter on the service team [11,12 ...
Peer support is being integrated within mental health services to further the development of a recovery approach. However, the most effective models and formats of intervention delivery are unknown. We conducted this systematic review and meta-analysis to determine the effectiveness of peer support for improving outcomes for people with lived experience of mental health conditions, when ...
According to published literature, peer support among young adults is being evaluated as delivered predominantly via in-person modality, though several studies investigated group peer support and other modalities of delivery (ie, over the internet or phone). ... A review of the literature on peer support in mental health services. J Ment Health ...
Peer support, defined as "giving and receiving help founded on key principles of respect, shared responsibility, and mutual agreement of what is helpful" delivered by individuals with lived experiences of mental illness, is regarded as a central element in recovery-oriented practices (1, 8-13).In the 1970s, peer support emerged in nongovernmental organizations (NGOs), and in recent years ...
Corresponding Author: Reham A Hameed Shalaby, MD Department of Psychiatry University of Alberta 1E1 Walter Mackenzie Health Sciences Centre. 8440 112 St NW Edmonton, AB, T6G 2B7 Canada Phone: 1 ...
An updated review, focussed on one-to-one peer support, is timely given current policy interest. ... The peer support literature has been reviewed before, with Pitt and colleagues finding a small reduction in emergency service use where peer workers were compared with other mental health professionals working in similar roles ...
Repper J, Carter T. A review of the literature on peer support in mental health services. Journal of Mental Health. 2011; 20 (4):392-411. doi: 10.3109/09638237.2011.583947. [Google Scholar] Shepardson RL, Johnson EM, Possemato K, Arigo D, Funderburk JS. Perceived barriers and facilitators to implementation of peer support in veterans health ...
Aims: To review the published research literature relating to the process of peer support and its underpinning mechanisms to better understand how and why it works. Method: A scoping review of published literature identified studies relating to peer support mechanisms, processes and relationships. Studies were summarised and findings analysed.
Background: Although mutual support and self-help groups based on shared experience play a large part in recovery, the employment of peer support workers (PSWs) in mental health services is a recent development. However, peer support has been implemented outside the UK and is showing great promise in facilitating recovery. Aims: This article aims to review the literature on PSWs employed in ...
Method: A scoping review of published literature identified studies relating to peer support mechanisms, processes and relationships. Studies were summarised and findings analysed.
A number of reviews of the literature concerned with self-help/mutual support (Pistrang, Barker, & Humphreys, 2008; Raiff, 1984) and peer-run services (e.g. Davidson et al., 1999; Humphreys, 1997) have been published. Other reviews have concerned themselves with all types of service user employment in evaluation, training and service delivery ...
Greetwell Road, Lincoln LN2 5UA, UK. Abstract. Background. Although mutual support and self-help groups based on shared experience play a large. part in recovery, the employment of peer support ...
In this scoping review, we examine peer support work within the context of intimate partner violence (IPV) service provision, including an examination of how this approach is conceptualized, the mechanisms underlying it, the impact of professionalism, and the benefits and challenges experienced by IPV peer support workers (PSWs).
This article reports the results of a literature review that was undertaken to assess the effects of peer support groups, one aspect of peer support services, in the treatment of addiction. Methods The authors of this article searched electronic databases of relevant peer-reviewed research literature including PubMed and MedLINE.
A Literature Review. Thomasina Borkman reviews English-language social science research on North American self-help/mutual aid groups (SHGs) and organizations and some from industrialized countries. SHGs, known by many names, are voluntary, member-run groups of peers who share a common issue, utilize lived experience, and practice mutual aid.
Search terms included peer support, peer support in mental health, social support, peer, family support, and integrated care. We began the review with an examination of the definitions, origins, and types of peer support contributions and within different clinical contexts, aiming at deepening the view to the diverse effects of such a workforce.
Writing a literature review requires a range of skills to gather, sort, evaluate and summarise peer-reviewed published data into a relevant and informative unbiased narrative. Digital access to research papers, academic texts, review articles, reference databases and public data sets are all sources of information that are available to enrich ...
The academic literature acknowledges the significance of the expatriation process, but the studies on the final phase of this process, repatriation, remain fragmented. This paper systematically reviews and analyses 129 articles published in peer-reviewed journals.
Rationale & objective: Formalized peer support is a promising approach for addressing the emotional and practical needs of people living with chronic kidney disease (CKD). We aimed to systematically identify and summarize peer support interventions studied in individuals with CKD with or without kidney replacement therapy (KRT).
We retrieved literature from PubMed, EMBASE, and CENTRAL until 10 January 2024. Eligible studies were both randomized trials and nonrandomised studies with a control group, published in the English language and peer-reviewed journals. The primary outcome was tracheal intubation; secondary outcomes were (i) bradycardia and (ii) hypotension.