Key EBP Nursing Topics: Enhancing Patient Results through Evidence-Based Practice
This article was written in collaboration with Christine T. and ChatGPT, our little helper developed by OpenAI.

Evidence-based practice (EBP) is the use of the best available evidence to inform clinical decision-making in nursing. EBP has become increasingly popular in nursing practice because it ensures that patient care is based on the most current and relevant research. In this article, we will discuss the latest evidence-based practice nursing research topics, how to choose them, and where to find EBP project ideas.

What is Evidence-Based Practice Nursing?
EBP nursing involves a cyclical process of asking clinical questions, seeking the best available evidence, critically evaluating that evidence, and then integrating it with the patient’s clinical experience and values to make informed decisions. By following this process, nurses can provide the best care for their patients and ensure that their practice is informed by the latest research.
One of the key components of EBP nursing is the critical appraisal of research evidence. Nurses must be able to evaluate the quality of studies, including study design, sample size, and statistical analysis. This requires an understanding of research methodology and the ability to apply critical thinking skills to evaluate research evidence.
EBP nursing also involves the use of clinical practice guidelines and protocols, which are evidence-based guidelines for clinical practice. These guidelines have been developed by expert groups and are based on the best available evidence. By following these guidelines, nurses can ensure that their practice is in line with the latest research and can provide the best possible care for their patients.
Finally, EBP nursing involves continuous professional development and a commitment to lifelong learning. Nurses must keep abreast of the latest research and clinical practice guidelines to ensure that their practice is informed by the latest research. This requires a commitment to ongoing learning and professional development, including attending conferences, reading scholarly articles, and participating in continuing education programs.
You can also learn more about evidence-based practice in nursing to gain a deeper understanding of the definition, stages, benefits, and challenges of implementing it.
Stay original!
Get 20% Discount for Plagiarism-Free and AI-Proof
How to Choose Evidence-Based Practice Nursing Research Topics
Choosing a science-based topic for nursing practice can be a daunting task, especially if you are new to the field. Here are some tips to help you choose a relevant and interesting EBP topic:
- Look for controversial or debated issues
Look for areas of nursing practice that are controversial or have conflicting evidence. These topics often have the potential to generate innovative and effective research.
- Consider ethical issues
Consider topics related to ethical issues in nursing practice. For example, bereavement care, informed consent , and patient privacy are all ethical issues that can be explored in an EBP project.
- Explore interdisciplinary topics
Nursing practice often involves collaboration with other health professionals such as physicians, social workers, and occupational therapists. Consider interdisciplinary topics that may be useful from a nursing perspective.
- Consider local or regional issues
Consider topics that are relevant to your local or regional healthcare facility. These topics may be relevant to your practice and have a greater impact on patient outcomes in your community.
- Check out the latest research
Review recent research in your area of interest to identify gaps in the literature or areas where further research is needed. This can help you develop a research question that is relevant and innovative.
With these tips in mind, you can expand your options for EBP nursing research topics and find a topic that fits your interests and goals. Remember that patient outcomes should be at the forefront of your research and choose a topic that has the potential to improve treatment and patient outcomes.
Where to Get EBP Project Ideas
There are several sources that nurses can use to get EBP project ideas. These sources are diverse and can provide valuable inspiration for research topics. By exploring these sources, nurses can find research questions that align with their interests and that address gaps in the literature. These include:
- Clinical Practice Guidelines
Look for clinical practice guidelines developed by professional organizations or healthcare institutions. These guidelines provide evidence-based guidelines for clinical practice and can help identify areas where further research is needed.
- Research databases
Explore research databases such as PubMed, CINAHL, and the Cochrane Library to find the latest studies and systematic reviews. These databases can help you identify gaps in the literature and areas where further research is needed.
- Clinical Experts
Consult with clinical experts in your practice area. These experts may have insights into areas where further research is needed or may provide guidance on areas of practice that may benefit from an EBP project.
- Quality Improvement Projects
Review quality improvement projects that have been implemented in your healthcare facility. These projects may identify areas where further research is needed or identify gaps in the literature that could be addressed in an EBP project.
- Patient and family feedback
Consider patient and family feedback to identify areas where further research is needed. Patients and families can provide valuable information about areas of nursing practice that can be improved or that could benefit from further research.
Remember, when searching for ideas for EBP nursing research projects, it is important to consider the potential impact on patient care and outcomes. Select a topic that has the potential to improve patient outcomes and consider the feasibility of the project in terms of time, resources, and access to data. By choosing a topic that matches your interests and goals and is feasible at your institution, you can conduct a meaningful and productive EBP research project in nursing.
Nursing EBP Topics You Can Use in Your Essay
Here are some of the latest evidence-based practice nursing research topics that you can use in your essay or explore further in your own research:
- The impact of telehealth on patient outcomes in primary care
- The use of music therapy to manage pain in post-operative patients
- The effectiveness of mindfulness-based stress reduction in reducing stress and anxiety in healthcare workers
- Combating health care-associated infections: a community-based approach
- The impact of nurse-led discharge education on readmission rates for heart failure patients
- The use of simulation in nursing education to improve patient safety
- The effectiveness of early mobilization in preventing post-operative complications
- The use of aromatherapy to manage agitation in patients with dementia
- The impact of nurse-patient communication on patient satisfaction and outcomes
- The effectiveness of peer support in improving diabetes self-management
- The impact of cultural competence training on patient outcomes in diverse healthcare settings
- The use of animal-assisted therapy in managing anxiety and depression in patients with chronic illnesses
- The effectiveness of nurse-led smoking cessation interventions in promoting smoking cessation among hospitalized patients
- Importance of literature review in evidence-based research
- The impact of nurse-led care transitions on hospital readmission rates for older adults
- The effectiveness of nurse-led weight management interventions in reducing obesity rates among children and adolescents
- The impact of medication reconciliation on medication errors and adverse drug events
- The use of mindfulness-based interventions to manage chronic pain in older adults
- The effectiveness of nurse-led interventions in reducing hospital-acquired infections
- The impact of patient-centered care on patient satisfaction and outcomes
- The use of art therapy to manage anxiety in pediatric patients undergoing medical procedures
- Pediatric oncology: working towards better treatment through evidence-based research
- The effectiveness of nurse-led interventions in improving medication adherence among patients with chronic illnesses
- The impact of team-based care on patient outcomes in primary care settings
- The use of music therapy to improve sleep quality in hospitalized patients
- The effectiveness of nurse-led interventions in reducing falls in older adults
- The impact of nurse-led care on maternal and infant outcomes in low-resource settings
- The use of acupressure to manage chemotherapy-induced nausea and vomiting
- The effectiveness of nurse-led interventions in promoting breastfeeding initiation and duration
- The impact of nurse-led palliative care interventions on end-of-life care in hospice settings
- The use of hypnotherapy to manage pain in labor and delivery
- The effectiveness of nurse-led interventions in reducing hospital length of stay for surgical patients
- The impact of nurse-led transitional care interventions on readmission rates for heart failure patients
- The use of massage therapy to manage pain in hospitalized patients
- The effectiveness of nurse-led interventions in promoting physical activity among adults with chronic illnesses
- The impact of technology-based interventions on patient outcomes in mental health settings
- The use of mind-body interventions to manage chronic pain in patients with fibromyalgia
- Optimizing the clarifying diagnosis of stomach cancer
- The effectiveness of nurse-led interventions in reducing medication errors in pediatric patients
- The impact of nurse-led interventions on patient outcomes in long-term care settings
- The use of aromatherapy to manage anxiety in patients undergoing cardiac catheterization
- The effectiveness of nurse-led interventions in improving glycemic control in patients with diabetes
- The impact of nurse-led interventions on patient outcomes in emergency department settings
- The use of relaxation techniques to manage anxiety in patients with cancer
- The effectiveness of nurse-led interventions in improving self-management skills among patients with heart failure
- The impact of nurse-led interventions on patient outcomes in critical care settings
- The use of yoga to manage symptoms in patients with multiple sclerosis
- The effectiveness of nurse-led interventions in promoting medication safety in community settings
- The impact of nurse-led interventions on patient outcomes in home healthcare settings
- The role of family involvement in the rehabilitation of stroke patients
- Assessing the effectiveness of virtual reality in pain management
- The impact of pet therapy on mental well-being in elderly patients
- Exploring the benefits of intermittent fasting on diabetic patients
- The efficacy of acupuncture in managing chronic pain in cancer patients
- Effect of laughter therapy on stress levels among healthcare professionals
- The influence of a plant-based diet on cardiovascular health
- Analyzing the outcomes of nurse-led cognitive behavioral therapy sessions for insomnia patients
- The role of yoga and meditation in managing hypertension
- Exploring the benefits of hydrotherapy in post-operative orthopedic patients
- The impact of digital health applications on patient adherence to medications
- Assessing the outcomes of art therapy in pediatric patients with chronic illnesses
- The role of nutrition education in managing obesity in pediatric patients
- Exploring the effects of nature walks on mental well-being in patients with depression
- The impact of continuous glucose monitoring systems on glycemic control in diabetic patients
The Importance of Incorporating EBP in Nursing Education
Evidence-based practice is not just a tool for seasoned nurses; it’s a foundational skill that should be integrated early into nursing education. By doing so, students learn the mechanics of nursing and the rationale behind various interventions grounded in scientific research.
- Bridging Theory and Practice:
Introducing EBP in the curriculum helps students bridge the gap between theoretical knowledge and clinical practice. They learn how to perform a task and why it’s done a particular way.
- Critical Thinking:
EBP promotes critical thinking. By regularly reviewing and appraising research, students develop the ability to discern the quality and applicability of studies. This skill is invaluable in a rapidly evolving field like healthcare.
- Lifelong Learning:
EBP instills a culture of continuous learning. It encourages nurses to regularly seek out the most recent research findings and adapt their practices accordingly.
- Improved Patient Outcomes:
At the heart of EBP is the goal of enhanced patient care. We ensure patients receive the most effective, up-to-date care by teaching students to base their practices on evidence.
- Professional Development:
Familiarity with EBP makes it easier for nurses to contribute to professional discussions, attend conferences, and conduct research. It elevates their professional stature and opens doors to new opportunities.
To truly prepare nursing students for the challenges of modern healthcare, it’s essential to make EBP a core part of their education.
In summary, evidence-based practice nursing is an essential component of providing quality patient care. As a nurse, it is important to stay up to date on the latest research in the field and incorporate evidence-based practices into your daily work. Choosing a research topic that aligns with your interests and addresses a gap in the literature can lead to valuable contributions to the field of nursing.
When it comes to finding EBP project ideas, there are many sources available, including professional organizations, academic journals, and healthcare conferences. By collaborating with colleagues and seeking feedback from mentors, you can refine your research question and design a study that is rigorous and relevant.
The nursing evidence-based practice topics listed above provide a starting point for further exploration and investigation. By studying the effectiveness of various nursing interventions and techniques, we can continue to improve patient outcomes and deliver better care. Ultimately, evidence-based practice nursing is about using the best available research to inform our decisions and provide the highest quality care possible to our patients.
📎 Related Articles
1. Top Nursing Research Topics for Students and Professionals 2. Nursing Debate Topics: The Importance of Discussing and Debating Nursing Issues 3. Mental Health Nursing Research Topics: Inspiring Ideas for Students 4. Top Nursing Argumentative Essay Topics: Engage in Thought-Provoking Debates 5. Top Nursing Topics for Discussion: Engaging Conversations for Healthcare Professionals 6. Exploring Controversial Issues in Nursing: Key Topics and Examples 7. Pediatric Nursing Research Topics for Students: A Comprehensive Guide
Table of content
Worried About Plagiarism?
Get 20% Off
on Plagiarism & AI Check Services!
What is Evidence-Based Practice in Nursing? (With Examples, Benefits, & Challenges)

Are you a nurse looking for ways to increase patient satisfaction, improve patient outcomes, and impact the profession? Have you found yourself caught between traditional nursing approaches and new patient care practices? Although evidence-based practices have been used for years, this concept is the focus of patient care today more than ever. Perhaps you are wondering, “What is evidence-based practice in nursing?” In this article, I will share information to help you begin understanding evidence-based practice in nursing + 10 examples about how to implement EBP.
What is Evidence-Based Practice in Nursing?
When was evidence-based practice first introduced in nursing, who introduced evidence-based practice in nursing, what is the difference between evidence-based practice in nursing and research in nursing, what are the benefits of evidence-based practice in nursing, top 5 benefits to the patient, top 5 benefits to the nurse, top 5 benefits to the healthcare organization, 10 strategies nursing schools employ to teach evidence-based practices, 1. assigning case studies:, 2. journal clubs:, 3. clinical presentations:, 4. quizzes:, 5. on-campus laboratory intensives:, 6. creating small work groups:, 7. interactive lectures:, 8. teaching research methods:, 9. requiring collaboration with a clinical preceptor:, 10. research papers:, what are the 5 main skills required for evidence-based practice in nursing, 1. critical thinking:, 2. scientific mindset:, 3. effective written and verbal communication:, 4. ability to identify knowledge gaps:, 5. ability to integrate findings into practice relevant to the patient’s problem:, what are 5 main components of evidence-based practice in nursing, 1. clinical expertise:, 2. management of patient values, circumstances, and wants when deciding to utilize evidence for patient care:, 3. practice management:, 4. decision-making:, 5. integration of best available evidence:, what are some examples of evidence-based practice in nursing, 1. elevating the head of a patient’s bed between 30 and 45 degrees, 2. implementing measures to reduce impaired skin integrity, 3. implementing techniques to improve infection control practices, 4. administering oxygen to a client with chronic obstructive pulmonary disease (copd), 5. avoiding frequently scheduled ventilator circuit changes, 6. updating methods for bathing inpatient bedbound clients, 7. performing appropriate patient assessments before and after administering medication, 8. restricting the use of urinary catheterizations, when possible, 9. encouraging well-balanced diets as soon as possible for children with gastrointestinal symptoms, 10. implementing and educating patients about safety measures at home and in healthcare facilities, how to use evidence-based knowledge in nursing practice, step #1: assessing the patient and developing clinical questions:, step #2: finding relevant evidence to answer the clinical question:, step #3: acquire evidence and validate its relevance to the patient’s specific situation:, step #4: appraise the quality of evidence and decide whether to apply the evidence:, step #5: apply the evidence to patient care:, step #6: evaluating effectiveness of the plan:, 10 major challenges nurses face in the implementation of evidence-based practice, 1. not understanding the importance of the impact of evidence-based practice in nursing:, 2. fear of not being accepted:, 3. negative attitudes about research and evidence-based practice in nursing and its impact on patient outcomes:, 4. lack of knowledge on how to carry out research:, 5. resource constraints within a healthcare organization:, 6. work overload:, 7. inaccurate or incomplete research findings:, 8. patient demands do not align with evidence-based practices in nursing:, 9. lack of internet access while in the clinical setting:, 10. some nursing supervisors/managers may not support the concept of evidence-based nursing practices:, 12 ways nurse leaders can promote evidence-based practice in nursing, 1. be open-minded when nurses on your teams make suggestions., 2. mentor other nurses., 3. support and promote opportunities for educational growth., 4. ask for increased resources., 5. be research-oriented., 6. think of ways to make your work environment research-friendly., 7. promote ebp competency by offering strategy sessions with staff., 8. stay up-to-date about healthcare issues and research., 9. actively use information to demonstrate ebp within your team., 10. create opportunities to reinforce skills., 11. develop templates or other written tools that support evidence-based decision-making., 12. review evidence for its relevance to your organization., bonus 8 top suggestions from a nurse to improve your evidence-based practices in nursing, 1. subscribe to nursing journals., 2. offer to be involved with research studies., 3. be intentional about learning., 4. find a mentor., 5. ask questions, 6. attend nursing workshops and conferences., 7. join professional nursing organizations., 8. be honest with yourself about your ability to independently implement evidence-based practice in nursing., useful resources to stay up to date with evidence-based practices in nursing, professional organizations & associations, blogs/websites, youtube videos, my final thoughts, frequently asked questions answered by our expert, 1. what did nurses do before evidence-based practice, 2. how did florence nightingale use evidence-based practice, 3. what is the main limitation of evidence-based practice in nursing, 4. what are the common misconceptions about evidence-based practice in nursing, 5. are all types of nurses required to use evidence-based knowledge in their nursing practice, 6. will lack of evidence-based knowledge impact my nursing career, 7. i do not have access to research databases, how do i improve my evidence-based practice in nursing, 7. are there different levels of evidence-based practices in nursing.
• Level One: Meta-analysis of random clinical trials and experimental studies • Level Two: Quasi-experimental studies- These are focused studies used to evaluate interventions. • Level Three: Non-experimental or qualitative studies. • Level Four: Opinions of nationally recognized experts based on research. • Level Five: Opinions of individual experts based on non-research evidence such as literature reviews, case studies, organizational experiences, and personal experiences.
8. How Can I Assess My Evidence-Based Knowledge In Nursing Practice?

Understanding Evidence-Based Practice in Nursing

In the ever-evolving field of healthcare, staying abreast of the latest advancements and providing optimal patient care is paramount. Evidence-Based Practice (EBP) in nursing stands at the forefront of this commitment, serving as a cornerstone for modern nursing practices. By harnessing the power of current research, clinical expertise, and patient preferences, EBP ensures that nursing care is both scientifically sound and deeply personalized. This approach not only enhances patient outcomes but also empowers nurses to make informed, effective clinical decisions. Let's delve deeper into the essence of EBP and its pivotal role in transforming nursing care.
Table of contents:
What is evidence-based practice in nursing?
Why is evidence-based practice important, evidence-based practice nursing examples.
Evidence-Based Practice (EBP) in nursing is a method of making clinical decisions based on the best available current research, clinical expertise, and patient preferences. This approach integrates the most relevant and up-to-date scientific evidence with clinical expertise and patient values to provide the highest quality of care.
EBP follows a systematic process that includes:
- Formulating a clear clinical question from a patient’s problem.
- Searching for the best available evidence.
- Appraising the quality of the evidence.
- Applying the evidence to clinical practice.
- Evaluating the outcomes of the decision or intervention.
- Improves Patient Outcomes: EBP ensures that patient care is based on the most current and valid research , which leads to better health outcomes.
- Enhances Nursing Practices: By continually integrating new research, nursing practices remain up-to-date and effective.
- Promotes Efficient Use of Resources: EBP helps in making informed decisions about resource allocation, reducing waste, and ensuring cost-effective care.
- Empowers Nurses: Nurses who use EBP are better equipped to provide high-quality care, which can increase job satisfaction and professional development.
- Meets Regulatory and Accreditation Standards: Many healthcare organizations and accrediting bodies emphasize the use of EBP to ensure high standards of care.
- Pressure ulcer prevention example
Research has shown that using specific mattress types and regular repositioning of patients can significantly reduce the incidence of pressure ulcers. By integrating these findings, nurses can create protocols to prevent pressure ulcers in at-risk patients.
- Hand hygiene practices example
EBP has demonstrated that proper hand hygiene is one of the most effective ways to prevent healthcare-associated infections (HAIs). Nursing protocols now include rigorous handwashing and the use of alcohol-based hand sanitizers to reduce infection rates.
- Pain management in postoperative patients example
Studies have shown that multimodal pain management approaches, which combine medications with non-pharmacological interventions (like ice packs, relaxation techniques, and physical therapy), can improve pain control. Nurses apply these strategies to manage postoperative pain more effectively.
- Fall prevention in elderly patients example
Evidence suggests that interventions such as regular exercise, home safety evaluations, and vision checks can reduce falls among the elderly. Nursing care plans often incorporate these evidence-based strategies to enhance patient safety.
- Diabetes management example
Research supports the effectiveness of self-management education and continuous glucose monitoring for patients with diabetes. Nurses play a crucial role in educating patients and implementing these practices to improve diabetes management and reduce complications.
Evidence-Based Practice in nursing is essential for providing high-quality, efficient, and patient-centered care. By integrating the best available research with clinical expertise and patient preferences, EBP enhances patient outcomes and supports continuous improvement in healthcare practices. Nurses who embrace EBP are well-positioned to lead the way in delivering innovative and effective care.
Wish you could choose your own nursing schedule? With CareRev you can.
Articles you may be interested in.

Guide to Earning Your Athletic Trainer Certification

Understanding CNA Burnout: Symptoms and Prevention

What is the Average Athletic Trainer Salary in the US?


ANA Nursing Resources Hub
Search Resources Hub

What is Evidence-Based Practice in Nursing?
5 min read • June, 01 2023
Evidence-based practice in nursing involves providing holistic, quality care based on the most up-to-date research and knowledge rather than traditional methods, advice from colleagues, or personal beliefs.
Nurses can expand their knowledge and improve their clinical practice experience by collecting, processing, and implementing research findings. Evidence-based practice focuses on what's at the heart of nursing — your patient. Learn what evidence-based practice in nursing is, why it's essential, and how to incorporate it into your daily patient care.
How to Use Evidence-Based Practice in Nursing
Evidence-based practice requires you to review and assess the latest research. The knowledge gained from evidence-based research in nursing may indicate changing a standard nursing care policy in your practice Discuss your findings with your nurse manager and team before implementation. Once you've gained their support and ensured compliance with your facility's policies and procedures, merge nursing implementations based on this information with your patient's values to provide the most effective care.
You may already be using evidence-based nursing practices without knowing it. Research findings support a significant percentage of nursing practices, and ongoing studies anticipate this will continue to increase.
Evidence-Based Practice in Nursing Examples
There are various examples of evidence-based practice in nursing, such as:
- Use of oxygen to help with hypoxia and organ failure in patients with COPD
- Management of angina
- Protocols regarding alarm fatigue
- Recognition of a family member's influence on a patient's presentation of symptoms
- Noninvasive measurement of blood pressure in children
Improving patient care begins by asking how you can make it a safer, more compassionate, and personal experience.
Learn about pertinent evidence-based practice information on our Clinical Practice Material page .
Five Steps to Implement Evidence-Based Practice in Nursing

Evidence-based nursing draws upon critical reasoning and judgment skills developed through experience and training. You can practice evidence-based nursing interventions by following five crucial steps that serve as guidelines for making patient care decisions. This process includes incorporating the best external evidence, your clinical expertise, and the patient's values and expectations.
- Ask a clear question about the patient's issue and determine an ultimate goal, such as improving a procedure to help their specific condition.
- Acquire the best evidence by searching relevant clinical articles from legitimate sources.
- Appraise the resources gathered to determine if the information is valid, of optimal quality compared to the evidence levels, and relevant for the patient.
- Apply the evidence to clinical practice by making decisions based on your nursing expertise and the new information.
- Assess outcomes to determine if the treatment was effective and should be considered for other patients.
Analyzing Evidence-Based Research Levels
You can compare current professional and clinical practices with new research outcomes when evaluating evidence-based research. But how do you know what's considered the best information?
Use critical thinking skills and consider levels of evidence to establish the reliability of the information when you analyze evidence-based research. These levels can help you determine how much emphasis to place on a study, report, or clinical practice guideline when making decisions about patient care.
The Levels of Evidence-Based Practice
Four primary levels of evidence come into play when you're making clinical decisions.
- Level A acquires evidence from randomized, controlled trials and is considered the most reliable.
- Level B evidence is obtained from quality-designed control trials without randomization.
- Level C typically gets implemented when there is limited information about a condition and acquires evidence from a consensus viewpoint or expert opinion.
- Level ML (multi-level) is usually applied to complex cases and gets its evidence from more than one of the other levels.
Why Is Evidence-Based Practice in Nursing Essential?

Implementing evidence-based practice in nursing bridges the theory-to-practice gap and delivers innovative patient care using the most current health care findings. The topic of evidence-based practice will likely come up throughout your nursing career. Its origins trace back to Florence Nightingale. This iconic founder of modern nursing gathered data and conclusions regarding the relationship between unsanitary conditions and failing health. Its application remains essential today.
Other Benefits of Evidence-Based Practice in Nursing
Besides keeping health care practices relevant and current, evidence-based practice in nursing offers a range of other benefits to you and your patients:
- Promotes positive patient outcomes
- Reduces health care costs by preventing complications
- Contributes to the growth of the science of nursing
- Allows for incorporation of new technologies into health care practice
- Increases nurse autonomy and confidence in decision-making
- Ensures relevancy of nursing practice with new interventions and care protocols
- Provides scientifically supported research to help make well-informed decisions
- Fosters shared decision-making with patients in care planning
- Enhances critical thinking
- Encourages lifelong learning
When you use the principles of evidence-based practice in nursing to make decisions about your patient's care, it results in better outcomes, higher satisfaction, and reduced costs. Implementing this method promotes lifelong learning and lets you strive for continuous quality improvement in your clinical care and nursing practice to achieve nursing excellence .
Images sourced from Getty Images
Related Resources

Item(s) added to cart
Evidence-Based Practice in Nursing Essay
- To find inspiration for your paper and overcome writer’s block
- As a source of information (ensure proper referencing)
- As a template for you assignment
Introduction
Methods of communication, challenges of delivering primary health care, the dilemma of providing care to vulnerable populations, portrayal in media, people in the waiting room.
Evidence-based practice (EBP) is firmly established as an essential component of nursing practice. Despite being present in some form in all nursing roles, its presence is arguably more prominent in professional nursing settings (RN). The RN’s responsibilities include planning patients’ care, analyzing their medical history, and administering medications (Ericksen, 2015). In addition, several managerial tasks and the duty of communicating with clinicians increase the scope of responsibilities. Most of these tasks directly determine patient outcomes depending on the quality of the made decisions. While it would be an understatement to say that practical nurses do not rely on evidence-based practices, in most cases, the outcomes of the patients are only indirectly dependent on EBP, which is the most obvious differentiation between PN and RN.
Two of the most evident methods of communication used in nursing practice are verbal and written communication. The former is used for everyday interaction with the patients, thus fulfilling their basic needs and providing counseling, education, and support necessary for improving long-term results. In both instances, the clarity and accessibility of the presented information determine the quality of care received by the patient. The written communication is responsible for providing clear instructions on treatment and healthy behaviors, thus facilitating the safety and trust of the patients. Therefore, non-native-English-speaking healthcare providers are obliged to provide oral and written translations of important documents, offer competent interpreter services, and notify the stakeholders of their right to use the services (VonBriesen, n.d.).
An environment designed for emergency medicine poses two major challenges to delivering primary health care. First, it does not offer any feasible means of continuity of care, such as access to a detailed medical history or a scheduled follow-up visit, which leads to frequent admissions for avoidable conditions. Second, the inadequately long wait times often lead to complications caused by the escalation of initially simple conditions such as high blood pressure (Leydon, 2012).
One of the challenges of patient-centered care is the disruption of balance in addressing the needs of patients with different needs. While it may seem logical to allocate more time to patients with more pressing needs and demanding conditions, it contributes to the mistreatment of populations with less apparent health risks. This eventually creates a situation where the latter have greater chances of developing adverse health conditions. Unfortunately, I cannot think of any meaningful solution to the problem aside from introducing additional regulations that ensure adequate time for both groups, although I acknowledge that such an approach may result in complications.
In order to attract viewers, the popular media often deliberately introduces inconsistencies to the portrayal of emergency rooms. First, the technical details of many procedures are commonly misrepresented, mostly to make them apparent to the viewer, with defibrillators being the most common example (MedicalBag, 2014). Second, the formal side is often diminished or neglected in favor of action scenes that resonate with the viewer, such as rushing through the corridor with the patient in an unstable condition. Third, the ethical side of the profession can be inaccurately portrayed in order to attract viewers interested in on-screen romance.
The people who enter the waiting room are characterized by the presence of an apparent health risk as well as a possibility of further complication determined by the timely delivery of care. Therefore, it would be appropriate to describe them as stressed and vulnerable.
Ericksen, K. (2015). P ractical nursing vs. professional nursing: Understanding the differences. Web.
Leydon, J. (2012). Emergency situation: The Waiting Room examines health care — and the lack of it — in America . Web.
MedicalBag. (2014). Fact or fiction: Do doctor dramas accurately portray real life in the ER? . Web.
VonBriesen. (n.d.). Health care provider’s obligations to non-English speaking patients . Web.
- Negligence as a Legal Issue in Nursing Care
- Adult Day Health Care Center: Practice Summary
- The RN to BSN: Curriculum Mapping
- Nursing: Delegation of the Re-Insertion of a Gastrointestinal Tube
- Delegation: Evidence-Based Practice Change Project
- Mental Health Nursing Skills in Practice
- Nursing Work in Different Cultures
- Legal Ramifications for Exceeding Nursing Duties
- Nursing as an Exemplary Career
- "Day of Care - 2017" Nursing Simulation Video
- Chicago (A-D)
- Chicago (N-B)
IvyPanda. (2021, May 14). Evidence-Based Practice in Nursing. https://ivypanda.com/essays/evidence-based-practice-in-nursing/
"Evidence-Based Practice in Nursing." IvyPanda , 14 May 2021, ivypanda.com/essays/evidence-based-practice-in-nursing/.
IvyPanda . (2021) 'Evidence-Based Practice in Nursing'. 14 May.
IvyPanda . 2021. "Evidence-Based Practice in Nursing." May 14, 2021. https://ivypanda.com/essays/evidence-based-practice-in-nursing/.
1. IvyPanda . "Evidence-Based Practice in Nursing." May 14, 2021. https://ivypanda.com/essays/evidence-based-practice-in-nursing/.
Bibliography
IvyPanda . "Evidence-Based Practice in Nursing." May 14, 2021. https://ivypanda.com/essays/evidence-based-practice-in-nursing/.
IvyPanda uses cookies and similar technologies to enhance your experience, enabling functionalities such as:
- Basic site functions
- Ensuring secure, safe transactions
- Secure account login
- Remembering account, browser, and regional preferences
- Remembering privacy and security settings
- Analyzing site traffic and usage
- Personalized search, content, and recommendations
- Displaying relevant, targeted ads on and off IvyPanda
Please refer to IvyPanda's Cookies Policy and Privacy Policy for detailed information.
Certain technologies we use are essential for critical functions such as security and site integrity, account authentication, security and privacy preferences, internal site usage and maintenance data, and ensuring the site operates correctly for browsing and transactions.
Cookies and similar technologies are used to enhance your experience by:
- Remembering general and regional preferences
- Personalizing content, search, recommendations, and offers
Some functions, such as personalized recommendations, account preferences, or localization, may not work correctly without these technologies. For more details, please refer to IvyPanda's Cookies Policy .
To enable personalized advertising (such as interest-based ads), we may share your data with our marketing and advertising partners using cookies and other technologies. These partners may have their own information collected about you. Turning off the personalized advertising setting won't stop you from seeing IvyPanda ads, but it may make the ads you see less relevant or more repetitive.
Personalized advertising may be considered a "sale" or "sharing" of the information under California and other state privacy laws, and you may have the right to opt out. Turning off personalized advertising allows you to exercise your right to opt out. Learn more in IvyPanda's Cookies Policy and Privacy Policy .

How to Write an EBP Nursing Research Paper – Helpful Guide for APA Nursing Research Papers [+ 6 Examples & Outline]
Rachel andel rn, bsn.
- August 12, 2022
- Nursing Writing Guides
Writing an evidence-based practice nursing research paper is a structured process that requires extensive research and the help of the right tools and guidance. An EBP nursing research paper has different components requiring systematic research, writing, and editing.
In this guide, we provide a structured approach on how to write an effective EBP Nursing Research Paper .
How to Write an Evidence-Based Paper – Step By Step Guide for APA Nursing Research Papers
EBP Nursing Research Paper Writing
Get EBP Paper Writing Help
- Experienced and Qualified Writers
- 100% Plagiarism Free
- Timely Delivery
- 🎓 MSN & DNP – LeveL Writing
- Confidentiality and Privacy
When writing an EBP nursing research paper, it is important to consider the components of an effective nursing research paper. Here are the different elements of an EBP paper and how to write each.
Introduction to the EBP Nursing Research Papers
In an introduction, you should briefly overview the topic you will discuss. This will help your instructor understand the main points of your paper.
How do you write an introduction for an EBP Nursing Research Paper?
The introduction should be brief but provide enough information to orient readers to the topic and guide them through the rest of the paper. It should also introduce key concepts and explain what will come.
When writing your introduction, make sure it;
- Defines the problem; it answers the question
- Patient/Problem: What problems does the patient group have? What needs to be solved?
- Intervention: What intervention is being considered or evaluated? Cite appropriate literature.
- Comparison: What other interventions are possible? Cite appropriate literature.
- Outcome: What is the intended outcome of the research question?
- Introduces the key concept, thus providing a transition to the next section, which reveals that the target population
- Clearly states the purpose of the report
- Identifies the target population.
- Relates to the significance of the problem
- also relates to the significance of the problem
You should include a clear statement of the research problem at the beginning or end of the introduction. This research problem can also generate the research question used to conduct the research itself.
Here’s an EBP Nursing Research Paper example ;
(1) Root caries is a disease of humans, which manifests as lesions on the root surfaces of teeth producing loss of the natural tooth structure. (2) The lesions progress to deeper and deeper levels of the root as well as spreading laterally to enwrap it. (3) Ultimately a lesion can progress to involve the pulp, threatening the viability of the tooth resulting in pain and eventual tooth loss. (4) When located between the teeth, the lesions are difficult to acess and therefore difficult to excise and restore. (5) In otherwise healthy, North American populations, root caries lesions increase with age. (6) This report sets out to provide evidence-based guidelines on the prevention of root caries for Toronto Public Helath staff on the best available evidence. https://www.una.edu/writingcenter/docs/Writing-Resource
Working on an EBP Nursing Research Paper?
Get nursing writing help for EBP nursing research papers, capstone papers, DNP projects, and Nursing Capstone Presentations. ZERO AI, ZERO Plagiarism and 💯 Timely Delivery.
EBP Nursing Literature Review
The literature review is one of the most important sections of an EBP paper. It should provide a detailed overview of the studies conducted on your topic. You should also include any relevant quotes from these studies.
When writing an effective EBP literature review, it is important to keep in mind the following tips:
- Take the time to read all the articles you cite in your review. This will help you understand the literature better and contextualize it.
- Be sure to cite your sources correctly. If you use a journal article, for example, include the author’s last name and publication year in your citations.
- Be concise in your writing. A literature review should not exceed 10 pages in length. Try to focus on key points and highlight why they are important.
- Use analytical techniques to help you evaluate the literature. For example, consider using qualitative or quantitative methods to analyze data.
- Make sure that your writing is accessible to a broad audience. If your research is technical, explain clearly how it was conducted and what it suggests.
EBP Nursing Research Paper Methodology
The methods section should describe how you researched the topic you are writing about. You should include details about the study you chose to utilize and any statistical analysis you performed.
How to write a methodology in an EBP Nursing Research Paper
Instead of collecting data through surveys, interviews, or clinical records, as in a quantitative or qualitative study, the data you collect is the literature produced on your topic.
Remember, the research you obtain is evidence like quantitative or qualitative data. But what evidence do you select to analyze?
It can be difficult to select evidence. Don’t just go with sources that work well for you, as this will only discredit your ideas. Consider assessing the dependability of the source, ensuring you have different viewpoints when considering a change in practice.
- What database did you search?
- Which search terms did you use, and how many total articles came up with those searches?
- If the search yielded few or fewer results, that may be because the search was too narrow.
The author considers many factors when evaluating sources. Here’s how to evaluate sources for your nursing research Papers
- Assess how trustworthy the source is, how accurate it is, and whether the source has a bias.
- The credibility of study material—is the study/journal credible and original? Research can be found in scholarly journals rather than general reading material.
- Validity: Does the study measure what it says it measures? What demographic sample did the study use? A study may be invalid or inaccurate if it does not produce an accurate margin of error.
- The same test needs to be done to get a true sense of reliability and yield the same results. The test needs to end when the results have been favorable. The results of the study are valid. The report suggests high levels of consistency and validity.
Here’s How to write a Critical Analysis in Nursing
Findings – How to present findings in the EBP Nursing Research Paper
The results and discussion section should provide a detailed analysis of your findings. Discuss the implications of findings and how policymakers can use them.
Your findings will be an analysis, possibly including a chart or table. You should present the studies you selected as the most appropriate sources for studying your problem and instituting your proposed change.
Be sure to compare the following aspects of each study:
- Demographics, pools, and samples
- Methods of discovery and analysis
- Results and limitations
Remember that these studies are supposed to be the most reliable and valid ones for answering the problem you found or the practice you wish to change. Your findings should lay the groundwork for making this argument in your discussion section.
Discussion: Conclusion and Recommendations for the EBP Nursing Research Paper
The conclusion section should summarize everything that has been discussed in the paper. It should provide a summary of your findings, and make any recommendations that you have for policymakers. Be Sure to:
- Argue that the findings lead to the specific change in practice you identified in your introduction.
- Suggest a strategy for implementation. Will the change you recommend (which these studies probably also recommend) work in your situation? Why? What changes might be needed?
Here’s a video guide
Here are a few key points to remember when writing your conclusion for an EBP Research Paper. First, combine all the information and data you’ve gathered throughout your paper.
Second, summarize your study’s findings and what they mean for nursing practice. Finally, provide recommendations for future research in this area.
History of Evidence-based Practice
The history of evidence-based practice (EBP) can be traced back to the early 1990s, when the Institute of Medicine published “To Err Is Human: Building a Safer Health System” which called for more use of evidence in health care decision making.
In 1992, the National Academies Press published “Principles of Evidence-Based Practice” which was a synthesis of work from multiple organizations and aimed to provide guidance on how to use evidence to improve patient care.
Since then, EBP has evolved into an increasingly popular approach to nursing practice. Today, EBP is used by nurses at all levels of education and experience, and it is becoming more integral to the way nurses deliver care. There are many reasons why EBP has become such an important tool in nursing practice, and this article will discuss some of them.
First, EBP helps nurses make informed decisions about patient care. Nurses need reliable information to provide quality care for their patients, and EBP provides that information by providing systematic reviews of research studies. Systematic reviews are a type of scientific literature review that systematically assess the quality and applicability of research studies in order to provide recommendations for clinical practice.
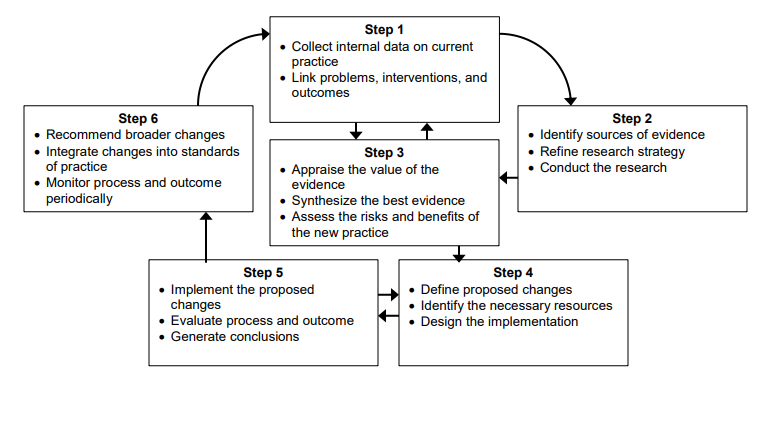
Steps of the EBP process
There are six steps in the Evidence-based Practice process:
Evidence-based practice involves the following six steps:
- Assess the need for change: Formulate the research question based on the inadequacies of current practice.- Identification of a problem or issue. Nurses should identify problems they see in their clinical practice and believe could benefit from intervention. For example, nurses may want to investigate whether patients who experience poor patient-centred outcomes after surgery have different factors, such as pain medication use or depression, that need to be addressed.
- Locate the best evidence: Obtain sources and assess their credibility and relevancy to the research question. Locate the best evidence & Synthesize evidence: Assessment of the current state of knowledge. To determine which interventions are likely to be effective, nurses should review the evidence on the effectiveness of interventions. This evidence can come from studies that have been conducted on interventions, from reviews of existing studies, or from clinical guidelines .
- 1) the target population for the intervention,
- 2) the severity of the problem or issue,
- 3) the feasibility of implementing the intervention
- 4) the cost of the intervention.
- Design the change: Apply the synthesized evidence to create a change in practice that reflects the new understanding. Selection and implementation of interventions. Nurses should select interventions that are likely effective for their target population, based on the factors listed in Step 3. They should then implement the interventions in a feasible and affordable way.
- Implement and evaluate: Apply the necessary changes and assess the changes to acquire new evidence. Evaluation of outcomes. After implementing interventions, nurses should evaluate their outcomes to determine their effectiveness. This evaluation can be done in several ways, such as through surveys or focus groups.
- Integrate and maintain changes: Reassess based on new evidence to continue improvement.
Nurses can use these steps to guide their EBP research in a number of ways. For example, they may want to investigate which interventions are most likely to be effective for a particular target population or problem, or they may want to determine which interventions are the most feasible and affordable to implement.
As you continue, nursingstudy.org/ has the top and most qualified writers to help with any of your assignments. All you need to do is place an order with us.
Find out more on
- How to write DNP capstone project Methodology Chapter
- How to write a DNP Capstone Project Literature Review
- How to write a DNP capstone project chapter 1 – Introduction
- DNP Capstone project Abstract Examples [Outline & How-to]
Evidence-Based Research Paper topics in Nursing
List of twenty EBP Nursing Research Paper ideas in nursing to write about
- Effectiveness of interventions for preventing falls in the elderly
- A pilot study of the efficacy of a home-based intervention to reduce falls in older adults
- Evaluating the effectiveness of a community-wide fall prevention intervention for older adults
- The impact of diabetes on balance and falls in older adults
- The effect of social isolation on falls in older adults
- The influence of ethnicity on falls in older adults
- Assessment and management of postural instability in the elderly
- Trends in hip fracture rates among older adults in the United States over time
- Reducing the risk factors for institutionalization among elders with Alzheimer’s disease
- Promoting healthy sleep habits among elders with dementia
- Assessing and managing sleep disturbances in elders with dementia
- Effects of exercise interventions on balance, mobility, and safety in seniors
- Rehabilitation after stroke: Targeting fall prevention
- The Effect of Nurse-Family Partnership on maternal and child health outcomes
- The Relationship of Depression to Nursing Home Use and Mortality
- Factors Influencing Patient Compliance with Diabetes Management Guidelines
- Contributions of Breastfeeding to Infant and Young Child Nutrition
- Role of the nurse in community-acquired pneumonia prevention
- Effectiveness of home health aide services on elder quality of life
- Impact of Acute Care Hospitals on the Nation’s Health
Plan of the EBP Nursing Research Paper
Writing an EBP Nursing research paper can be daunting, but it can be much easier with a plan. This guide will provide you with the essential steps you need to take to produce high-quality research papers. First, you will need to identify the problem you are researching. Next, identify the population most likely to experience the problem and/or share its consequences.
Finally, using evidence-based practices as your guide, develop a plan of action that will address the problem.
Read more on How to Format a CV for a Nursing Position Examples
Identify the Problem
The first step in writing an EBP nursing research paper is to identify the problem you are researching. This can be difficult, as the problem may be subtle or complex. However, you can use rigorous research methods to identify the problem and its consequences.
Once you have identified the problem, you must identify the population most likely to experience it and/or share its consequences. This can be a difficult task, as it may be difficult to differentiate between those affected by the problem and those not. However, by using reliable sources of information, you can develop a profile of the population that will help you identify which groups are most at risk.
Once you have identified the population most likely to experience the problem, you to develop a plan of action to address it. This action plan should be based on evidence-based practices, ensuring that your proposal is effective and efficient.
Find out more on Nursing Essay Thesis Statement [+How to & Examples]
Develop a Plan of Action
The next step in writing an EBP nursing research paper is to develop a plan of action. This action plan should be based on the evidence you have gathered and the population you have identified as most at risk.
Your action plan should include specific objectives, targets, timelines, and budgetary constraints. It should also include measures to resolve the problem, including benchmarks and measurements.
Finally, your action plan should be evaluated and revised based on stakeholder feedback. This feedback will help you ensure that your proposal is effective and efficient.
Writing an EBP nursing research paper can be daunting, but it can be much easier with a plan. This guide will provide you with the essential steps you need to take to produce high-quality research papers. First, you will need to identify the problem you are researching. Next, identify the population most likely to experience the problem and/or share its consequences. Finally, using evidence-based practices as your guide, develop a plan of action that will address the issue.
Steps of Writing an EBP Research Paper in Nursing
1. Determine the purpose of your EBP study. 2. Choose a relevant population or setting. 3. Identify the specific question you wish to answer. 4. Collect and analyze data. 5. Construct a hypothesis or theory based on your findings. 6. Write a conclusion that supports your thesis statement. 7. Offer suggestions for future research on evidence-based practice in nursing.
EBP Research Paper Literature Review Writing- Evidence-Based Practice (EBP)
Evidence-based practice (EBP) is an approach to nursing that focuses on using evidence to guide clinical decisions. EBP is effective in improving patient outcomes and reducing healthcare costs. To write an effective EBP literature review, it is important to understand the concepts of evidence and research.
The following section will provide a brief overview of the concept of evidence and its role in EBP. After this, the section will outline the different types of research used in EBP and discuss how to select appropriate research for your paper. Finally, the section will provide tips for writing an effective literature review.
You might be interested in Nursing Case Study Analysis [10 Examples & How-To Guides]
What is Evidence?
Evidence is information that supports a belief or theory. It can come from either personal experience or empirical research. Personal experience includes things like doctor’s orders or patient statements. Empirical research includes studies that use scientific methods to collect data about a particular topic.
Why Use Evidence in Nursing?
There are many reasons why using evidence in nursing is important. First, it can help improve patient outcomes. For example, using evidence-based practices when caring for patients with diabetes can help control their blood sugar levels and reduce the risk of complications.
Second, using evidence can reduce healthcare costs. For example, using evidence-based interventions when caring for patients with heart disease can help reduce the risk of death and hospitalization.
Finally, using evidence can help nurses make better decisions. For example, when caring for a patient with cancer, it is important to use evidence-based treatments that are effective in reducing the risk of cancer recurrence.
What Types of Research is Used in EBP?
There are many different types of research used in EBP. The following section will outline the different types of research and discuss how to select appropriate research for your paper.
- Clinical trials: Clinical trials are experiments that are designed to test the effectiveness of a new treatment or intervention. Clinical trials can be conducted in hospitals or clinics.
- Evaluation studies: Evaluation studies compare the outcomes of two or more treatments or interventions. Evaluation studies can be conducted in hospitals or clinics.
- Observational studies: Observational studies collect data about how people behave without Intervention. Observational studies can be conducted at home, work, or anywhere people gather data.
How to Select Appropriate Research for Your Paper
When selecting research for your EBP nursing research paper, it is important to consider the topic you are writing about and the audience you are writing for. The following tips can help you select appropriate research for your paper.
- First, consider the topic you are writing about. If you are writing about a new treatment or intervention, it is important to use clinical trials. Clinical trials are experiments that are designed to test the effectiveness of a new treatment or intervention.
- If you are writing about an existing treatment or intervention, it is important to use observational studies. Observational studies are studies that collect data about how people behave without Intervention. These studies can be conducted at home, work, or anywhere else people gather data.
- Second, consider the audience you are writing for. If you are writing for a healthcare provider, using evidence-based practices that effectively improve patient outcomes and reduce healthcare costs is essential. If you are writing for a patient or their family, using understandable and relatable information is essential.
- Finally, always check the credibility of any sources used in your paper. Credible sources will typically have references that can be verified.
Using credible sources for Evidence-based practice paper
Evidence-based practice (EBP) is a nursing research methodology that draws on published, peer-reviewed scientific studies to develop rationales for and recommendations for patient care.
- It is important to use credible sources to write an EBP paper that is both credible and useful. Credible sources have been examined by experts in the field and found to be reliable. To identify credible sources, it is helpful first to understand what constitutes evidence-based practice.
- The five types of evidence considered most important in EBP are randomized clinical trials (RCTs), systematic reviews, meta-analyses, case reports, and expert opinion.
- When using any of these types of evidence, it is important to ensure the study was conducted according to strict methodological standards.
- For example, RCTs must be blinded (i.e., the participants and investigators should not know which group is receiving the treatment being studied). Furthermore, all data collected during an RCT must be reported accurately and completely.
- Once you have identified a study as credible, the next step is to determine whether the study’s findings are relevant to your topic. It is important to note that not all studies that qualify as evidence-based practice apply to every topic.
- For example, a study that explores the use of acupuncture as a treatment for chronic neck pain would not apply to writing an EBP paper on the use of epidural analgesia in childbirth.
- Finally, it is important to consider the implications of the study’s findings when writing an EBP paper.
- For example, if a study found that a particular treatment was ineffective, it is important to discuss why this might be the case and what can be done to address the issue.
What are the 5 A’s in evidence-based practice?
Evidence-based practice is a healthcare approach that is based on the use of evidence from research studies to make decisions about care. Here are the A’s in evidence-based practice:
- Anchor: The anchor for your paper should be a specific and meaningful study that provides the basis for your argument.
- Background: State the purpose of your paper, including why you are studying the issue.
- Methods: Describe how you conducted your study and collected the data.
- Results: Discuss the findings of your study in detail, including any relevant conclusions.
- Discussion: Explain how this information can be used to improve patient care.
How do nurses write evidence based practice papers?
There are a few key steps that nurses should take when writing evidence based practice papers, including conducting research, analyzing data, and writing effective conclusions.
Here are more specific tips on how to go about each of these steps:
1. Conduct Research: The first step in writing an evidence-based practice paper is to conduct research. This means gathering information from reliable sources to support your arguments. You can find information on different types of research in the library, online databases, and journals. When selecting sources, be sure to select studies that are relevant to your topic and that you can trust.
2. Analyze Data: After you have gathered your data, it is important to analyze it carefully. This means looking at the data from different perspectives and using logic and reasoning to arrive at a conclusion. Be sure to state your findings clearly and concisely so that others can understand them.
3. Write Effective Conclusions: The final step in writing an evidence-based practice paper is to write effective conclusions. This section should summarize your findings and include any recommendations that you have for improving patient care. Remember to support your recommendations with credible evidence.
Working On an Assignment With Similar Concepts Or Instructions?
A Page will cost you $12, however, this varies with your deadline.
We have a team of expert nursing writers ready to help with your nursing assignments. They will save you time, and improve your grades.
Whatever your goals are, expect plagiarism-free works, on-time delivery, and 24/7 support from us.
Here is your 15% off to get started. Simply:
- Place your order ( Place Order )
- Click on Enter Promo Code after adding your instructions
- Insert your code – Get20
All the Best,
Have a subject expert Write for You Now
Have a subject expert finish your paper for you, edit my paper for me, have an expert write your dissertation's chapter, what you'll learn.
- Nursing Careers
- Nursing Paper Solutions
- Nursing Theories
- Nursing Topics and Ideas
Related Posts
- Kathleen Masters Nursing Theories: A Framework for Professional Practice
- Rural Nursing Theory: A Guide for Nursing Students
- Barbara Resnick Nursing Theory: A Comprehensive Guide for Nursing Students
Important Links
Knowledge base.
Nursingstudy.org helps students cope with college assignments and write papers on various topics. We deal with academic writing, creative writing, and non-word assignments.
All the materials from our website should be used with proper references. All the work should be used per the appropriate policies and applicable laws.
Our samples and other types of content are meant for research and reference purposes only. We are strongly against plagiarism and academic dishonesty.
Phone: +1 628 261 0844
Mail: [email protected]

We Accept:

@2015-2024, Nursingstudy.org
This website is intended for healthcare professionals

- { $refs.search.focus(); })" aria-controls="searchpanel" :aria-expanded="open" class="hidden lg:inline-flex justify-end text-gray-800 hover:text-primary py-2 px-4 lg:px-0 items-center text-base font-medium"> Search
Search menu
Brechin A. Introducing critical practice. In: Brechin A, Brown H, Eby MA (eds). London: Sage/Open University; 2000
Introduction to evidence informed decision making. 2012. https://cihr-irsc.gc.ca/e/45245.html (accessed 8 March 2022)
Cullen L, Adams SL. Planning for implementation of evidence-based practice. JONA: The Journal of Nursing Administration. 2012; 42:(4)222-230 https://doi.org/10.1097/NNA.0b013e31824ccd0a
DiCenso A, Guyatt G, Ciliska D. Evidence-based nursing. A guide to clinical practice.St. Louis (MO): Mosby; 2005
Implementing evidence-informed practice: International perspectives. In: Dill K, Shera W (eds). Toronto, Canada: Canadian Scholars Press; 2012
Dufault M. Testing a collaborative research utilization model to translate best practices in pain management. Worldviews Evid Based Nurs. 2004; 1:S26-S32 https://doi.org/10.1111/j.1524-475X.2004.04049.x
Epstein I. Promoting harmony where there is commonly conflict: evidence-informed practice as an integrative strategy. Soc Work Health Care. 2009; 48:(3)216-231 https://doi.org/10.1080/00981380802589845
Epstein I. Reconciling evidence-based practice, evidence-informed practice, and practice-based research: the role of clinical data-mining. Social Work. 2011; 56:(3)284-288 https://doi.org/10.1093/sw/56.3.284
Implementation research: a synthesis of the literature. 2005. https://tinyurl.com/mwpf4be4 (accessed 6 March 2022)
Graham ID, Logan J, Harrison MB Lost in knowledge translation: time for a map?. J Contin Educ Health Prof. 2006; 26:(1)13-24 https://doi.org/10.1002/chp.47
Greenhalgh T, Robert G, Bate P, MacFarlane F, Kyriakidou O. Diffusion of innovations in health service organisations. A systematic literature review.Malden (MA): Blackwell; 2005
Greenhalgh T, Howick J, Maskrey N. Evidence based medicine: a movement in crisis?. BMJ. 2014; 348 https://doi.org/10.1136/bmj.g3725
Haynes RB, Devereaux PJ, Guyatt GH. Clinical expertise in the era of evidence-based medicine and patient choice. BMJ Evidence-Based Medicine. 2002; 7:36-38 https://doi.org/10.1136/ebm.7.2.36
Hitch D, Nicola-Richmond K. Instructional practices for evidence-based practice with pre-registration allied health students: a review of recent research and developments. Adv Health Sci Educ Theory Pract. 2017; 22:(4)1031-1045 https://doi.org/10.1007/s10459-016-9702-9
Jerkert J. Negative mechanistic reasoning in medical intervention assessment. Theor Med Bioeth. 2015; 36:(6)425-437 https://doi.org/10.1007/s11017-015-9348-2
McSherry R, Artley A, Holloran J. Research awareness: an important factor for evidence-based practice?. Worldviews Evid Based Nurs. 2006; 3:(3)103-115 https://doi.org/10.1111/j.1741-6787.2006.00059.x
McSherry R, Simmons M, Pearce P. An introduction to evidence-informed nursing. In: McSherry R, Simmons M, Abbott P London: Routledge; 2002
Implementing excellence in your health care organization: managing, leading and collaborating. In: McSherry R, Warr J (eds). Maidenhead: Open University Press; 2010
Melnyk BM, Fineout-Overholt E, Stillwell SB, Williamson KM. Evidence-based practice: step by step: the seven steps of evidence-based practice. AJN, American Journal of Nursing. 2010; 110:(1)51-53 https://doi.org/10.1097/01.NAJ.0000366056.06605.d2
Implementing evidence-based practices: six ‘drivers’ of success. Part 3 in a Series on Fostering the Adoption of Evidence-Based Practices in Out-Of-School Time Programs. 2007. https://tinyurl.com/mu2y6ahk (accessed 8 March 2022)
Muir-Gray JA. Evidence-based healthcare. How to make health policy and management decisions.Edinburgh: Churchill Livingstone; 1997
Nevo I, Slonim-Nevo V. The myth of evidence-based practice: towards evidence-informed practice. British Journal of Social Work. 2011; 41:(6)1176-1197 https://doi.org/10.1093/bjsw/bcq149
Newhouse RP, Dearholt S, Poe S, Pugh LC, White K. The Johns Hopkins Nursing Evidence-based Practice Rating Scale.: The Johns Hopkins Hospital: Johns Hopkins University School of Nursing; 2005
Nursing and Midwifery Council. The Code. 2018. https://www.nmc.org.uk/standards/code (accessed 7 March 2022)
Nutley S, Walter I, Davies HTO. Promoting evidence-based practice: models and mechanisms from cross-sector review. Research on Social Work Practice. 2009; 19:(5)552-559 https://doi.org/10.1177/1049731509335496
Reed JE, Howe C, Doyle C, Bell D. Successful Healthcare Improvements From Translating Evidence in complex systems (SHIFT-Evidence): simple rules to guide practice and research. Int J Qual Health Care. 2019; 31:(3)238-244 https://doi.org/10.1093/intqhc/mzy160
Rosswurm MA, Larrabee JH. A model for change to evidence-based practice. Image J Nurs Sch. 1999; 31:(4)317-322 https://doi.org/10.1111/j.1547-5069.1999.tb00510.x
Rubin A. Improving the teaching of evidence-based practice: introduction to the special issue. Research on Social Work Practice. 2007; 17:(5)541-547 https://doi.org/10.1177/1049731507300145
Shlonsky A, Mildon R. Methodological pluralism in the age of evidence-informed practice and policy. Scand J Public Health. 2014; 42:18-27 https://doi.org/10.1177/1403494813516716
Straus SE, Tetroe J, Graham I. Defining knowledge translation. CMAJ. 2009; 181:(3-4)165-168 https://doi.org/10.1503/cmaj.081229
Titler MG, Everett LQ. Translating research into practice. Considerations for critical care investigators. Crit Care Nurs Clin North Am. 2001; 13:(4)587-604 https://doi.org/10.1016/S0899-5885(18)30026-1
Titler MG, Kleiber C, Steelman V Infusing research into practice to promote quality care. Nurs Res. 1994; 43:(5)307-313 https://doi.org/10.1097/00006199-199409000-00009
Titler MG, Kleiber C, Steelman VJ The Iowa model of evidence-based practice to promote quality care. Crit Care Nurs Clin North Am. 2001; 13:(4)497-509 https://doi.org/10.1016/S0899-5885(18)30017-0
Ubbink DT, Guyatt GH, Vermeulen H. Framework of policy recommendations for implementation of evidence-based practice: a systematic scoping review. BMJ Open. 2013; 3:(1) https://doi.org/10.1136/bmjopen-2012-001881
Wang LP, Jiang XL, Wang L, Wang GR, Bai YJ. Barriers to and facilitators of research utilization: a survey of registered nurses in China. PLoS One. 2013; 8:(11) https://doi.org/10.1371/journal.pone.0081908
Warren JI, McLaughlin M, Bardsley J, Eich J, Esche CA, Kropkowski L, Risch S. The strengths and challenges of implementing EBP in healthcare systems. Worldviews Evid Based Nurs. 2016; 13:(1)15-24 https://doi.org/10.1111/wvn.12149
Webber M, Carr S. Applying research evidence in social work practice: Seeing beyond paradigms. In: Webber M (ed). London: Palgrave; 2015
Evidence-based practice vs. evidence-based practice: what's the difference?. 2014. https://tinyurl.com/2p8msjaf (accessed 8 March 2022)
Evidence-informed practice: simplifying and applying the concept for nursing students and academics
Elizabeth Adjoa Kumah
Nurse Researcher, Faculty of Health and Social Care, University of Chester, Chester
View articles · Email Elizabeth Adjoa
Robert McSherry
Professor of Nursing and Practice Development, Faculty of Health and Social Care, University of Chester, Chester
View articles
Josette Bettany-Saltikov
Senior Lecturer, School of Health and Social Care, Teesside University, Middlesbrough
Paul van Schaik
Professor of Research, School of Social Sciences, Humanities and Law, Teesside University, Middlesbrough

Background:
Nurses' ability to apply evidence effectively in practice is a critical factor in delivering high-quality patient care. Evidence-based practice (EBP) is recognised as the gold standard for the delivery of safe and effective person-centred care. However, decades following its inception, nurses continue to encounter difficulties in implementing EBP and, although models for its implementation offer stepwise approaches, factors, such as the context of care and its mechanistic nature, act as barriers to effective and consistent implementation. It is, therefore, imperative to find a solution to the way evidence is applied in practice. Evidence-informed practice (EIP) has been mooted as an alternative to EBP, prompting debate as to which approach better enables the transfer of evidence into practice. Although there are several EBP models and educational interventions, research on the concept of EIP is limited. This article seeks to clarify the concept of EIP and provide an integrated systems-based model of EIP for the application of evidence in clinical nursing practice, by presenting the systems and processes of the EIP model. Two scenarios are used to demonstrate the factors and elements of the EIP model and define how it facilitates the application of evidence to practice. The EIP model provides a framework to deliver clinically effective care, and the ability to justify the processes used and the service provided by referring to reliable evidence.
Evidence-based practice (EBP) was first mentioned in the literature by Muir-Gray, who defined EBP as ‘an approach to decision-making in which the clinician uses the best available evidence in consultation with the patient to decide upon the option which suits the patient best’ (1997:97). Since this initial definition was set out in 1997, EBP has gained prominence as the gold standard for the delivery of safe and effective health care.
There are several models for implementing EBP. Examples include:
Although a comprehensive review of these models is beyond the scope of this article, a brief assessment reveals some commonalities among them. These include a) asking or selecting a practice question, b) searching for the best evidence, c) critically appraising and applying the evidence, d) evaluating the outcome(s) of patient care delivery, and e) disseminating the outcome(s).
Regardless of the benefits of EBP, and the existence of multiple EBP models intended to facilitate the application of evidence into practice, health professionals, including nurses, continue to struggle to implement it effectively ( Ubbink et al, 2013 ). Critics of EBP have questioned its validity ( Rubin, 2007 ; Nevo and Slonim-Nevo, 2011 ); the best practice and setting to support its use ( Nutley et al, 2009 ); its failure to address the complexity of health and health care, as well as the patient's context ( Muir-Gray, 1997 ; Reed et al, 2019 ), and its mechanistic approach ( Epstein, 2009 ; Jerkert, 2015 ). Some of these criticisms are outlined below.
Register now to continue reading
Thank you for visiting British Journal of Nursing and reading some of our peer-reviewed resources for nurses. To read more, please register today. You’ll enjoy the following great benefits:
What's included
Limited access to clinical or professional articles
Unlimited access to the latest news, blogs and video content
Signing in with your registered email address
Masks Strongly Recommended but Not Required in Maryland
Respiratory viruses continue to circulate in Maryland, so masking remains strongly recommended when you visit Johns Hopkins Medicine clinical locations in Maryland. To protect your loved one, please do not visit if you are sick or have a COVID-19 positive test result. Get more resources on masking and COVID-19 precautions .
- Vaccines
- Masking Guidelines
- Visitor Guidelines
Center for Nursing Inquiry
Evidence-based practice, what is ebp.
As nurses, we often hear the term evidence-based practice (EBP). But, what does it actually mean? EBP is a process used to review, analyze, and translate the latest scientific evidence. The goal is to quickly incorporate the best available research, along with clinical experience and patient preference, into clinical practice, so nurses can make informed patient-care decisions ( Dang et al., 2022 ). EBP is the cornerstone of clinical practice. Integrating EBP into your nursing practice improves quality of care and patient outcomes.
How do I get involved in EBP?
As a nurse, you will have plenty of opportunities to get involved in EBP. Take that “AHA” moment. Do you think there’s a better way to do something? Let’s turn to the evidence and find out!
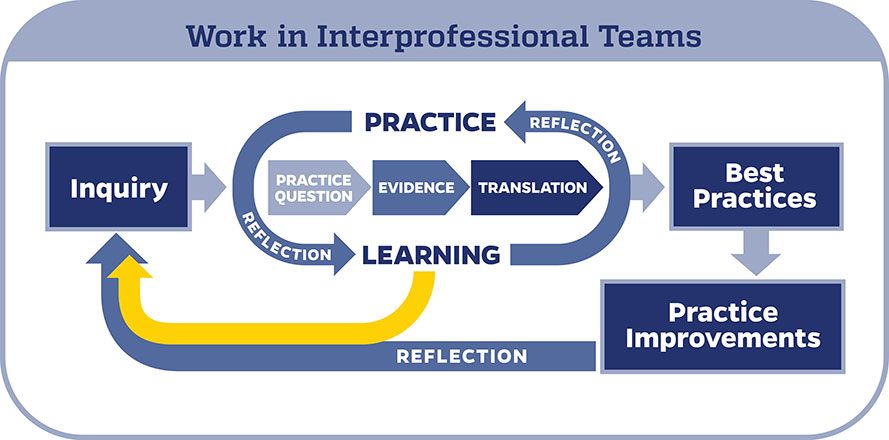
When conducting an EBP project, it is important to use a model to help guide your work. In the Johns Hopkins Health System, we use the Johns Hopkins Evidence-Based Practice (JHEBP) model. It is a three-phase approach referred to as the PET process: practice question, evidence, and translation. In the first phase, the team develops a practice question by identifying the patient population, interventions, and outcomes (PICO). In the second phase, a literature search is performed, and the evidence is appraised for strength and quality. In the third phase, the findings are synthesized to develop recommendations for practice.
The JHEBP model is accompanied by user-friendly tools. The tools walk you through each phase of the project. Johns Hopkins nurses can access the tools via our Inquiry Toolkit . The tools are available to individuals from other institutions via the Institute for Johns Hopkins Nursing (IJHN) .
If you’re interested in learning more about the JHEBP model and tools, Johns Hopkins nurses have access to a free online course entitled JHH Nursing | Central | Evidence-Based Practice Series in MyLearning. The course follows the JHEBP process from beginning to end and provides guidance to the learner on how to use the JHEBP tools. The course is available to individuals from other institutions for a fee via the Institute for Johns Hopkins Nursing (IJHN) .
Where should I start?
All EBP projects need to be submitted to the Center for Nursing Inquiry for review. The CNI ensures all nurse-led EBP projects are high-quality and value added. We also offer expert guidance and support, if needed.
Who can help me?
The Center for Nursing Inquiry can answer any questions you may have about the JHEBP tools. All 10 JHEBP tools can be found in our Inquiry Toolkit : project management guide, question development tool, stakeholder analysis tool, evidence level and quality guide, research evidence appraisal tool, non-research evidence appraisal tool, individual evidence summary tool, synthesis process and recommendations tool, action planning tool, and dissemination tool. The tools walk you through each phase of an EBP project.
The Welch Medical Library serves the information needs of the faculty, staff, and students of Johns Hopkins Medicine, Nursing and Public Health. Often, one of the toughest parts of conducting an EBP project is finding the evidence. The informationist assigned to your department can assist you with your literature search and citation management.
When do I share my work?
Your project is complete. Now what? It’s time to share your project with the scholarly community.
To prepare your EBP project for publication, use the JHEBP Dissemination Tool . The JHEBP Dissemination Tool (Appendix J) details what to include in each section of your manuscript, from the introduction to the discussion, and shows you which EBP appendices correspond to each part of a scientific paper. You can find the JHEBP Dissemination Tool in our Inquiry Toolkit .
You can also present your project at a local, regional, or national conference. Poster and podium presentation templates are available in our Inquiry Toolkit .
To learn more about sharing your project, check out our Abstract & Manuscript Writing webinar and our Poster & Podium Presentations webinar !
Submit Your Project
Do you have an idea for an EBP project?
- Research article
- Open access
- Published: 28 July 2018
Strategies for teaching evidence-based practice in nursing education: a thematic literature review
- May-Elin T. Horntvedt 1 ,
- Anita Nordsteien 2 ,
- Torbjørg Fermann 1 &
- Elisabeth Severinsson 3
BMC Medical Education volume 18 , Article number: 172 ( 2018 ) Cite this article
171k Accesses
152 Citations
8 Altmetric
Metrics details
Evidence-based practice (EBP) is imperative for ensuring patient safety. Although teaching strategies to enhance EBP knowledge and skills are recommended, recent research indicates that nurses may not be well prepared to apply EBP. A three-level hierarchy for teaching and learning evidence-based medicine is suggested, including the requirement for interactive clinical activities in EBP teaching strategies. This literature review identifies the teaching strategies for EBP knowledge and skills currently used in undergraduate nursing education. We also describe students’ and educators’ experiences with learning outcomes and barriers.
We conducted literature searches using Medline, Embase, CINAHL, ERIC and Academic Search Premier. Six qualitative studies and one mixed-method study met the inclusion criteria and were critically evaluated based on the Critical Appraisal Skills Programme. Using Braun and Clarke’s six phases, the seven studies were deductively and thematically analysed to discover themes.
Four teaching strategy themes were identified, including subthemes within each theme: i.e., interactive teaching strategies; interactive and clinical integrated teaching strategies; learning outcomes; and barriers. Although four studies included a vague focus on teaching EBP principles, they all included research utilisation and interactive teaching strategies. Reported learning outcomes included enhanced analytical and critical skills and using research to ensure patient safety. Barriers included challenging collaborations, limited awareness of EBP principles and poor information literacy skills.
Four of the seven analysed studies included a vague focus on the use of EBP teaching strategies. Interactive teaching strategies are used, but primary strategies focus on searching for and critically appraising research for practice-based application. Although this review included a relatively small sample of literature, the findings indicate a need for more qualitative research investigating interactive and clinically integrated teaching strategies towards further enhancing EBP undergraduate nursing students’ knowledge and skills.
Peer Review reports
Evidence-based practice (EBP) in health care has become imperative for patient safety. EBP involves a conscious use and application of various knowledge sources, including the use of published research in conjunction with clinical expertise and patient values and preferences [ 1 ]. The process of EBP includes that health-care personnel formulate structured queries, and then conduct searches of databases from which they acquire trustworthy and reliable evidence. Further, they must then critically appraise the research for its reliability, validity and applicability to a clinical context [ 2 , 3 ].
Interactive methods including interactive lectures, small group work, journal clubs, reading quizzes, clinical nurse presentations, workshops and problem-based learning are needed in teaching EBP [ 2 , 3 ]. An interactive approach involves an interaction amongst the participants [ 3 ]. Effective learning reflects the quality of teaching. Learning though a constructivist approach refers to the creation of an environment in which the learner is an active participant who gains experience and engages in reflection, leading to problem-based, transformative learning [ 4 ].To engage the next generation of nurses and enhance their EBP knowledge and skills, a variety of teaching strategies have been recommended [ 5 , 6 , 7 ].
Khan and Coomarasamy [ 3 ] have described a three-level hierarchy of evidence-based medicine (EBM) teaching and learning methods. The first level is interactive clinical activities. The second level is classroom didactics using clinical and interactive activities. Finally, although less preferred for teaching EBP, the third level is classroom didactic or stand-alone teaching [ 3 ]. According to Fineout-Overholt et al. [ 2 ], it is important to keep teaching strategies simple and integration of EBP must be a natural part of the academic culture.
Research supports the first level in this hierarchy when teaching EBP; i.e., an interactive style is often preferred because this method facilitates student learning [ 8 , 9 , 10 ]. Johnson et al. [ 11 ] found that new learning methods and blended approaches to teaching EBP impact students’ attitudes towards research. In addition, Crookes et al. [ 12 ] identified different meaningful and engaging teaching strategies that have been adopted by nurse educators, such as online teaching, gaming and simulation techniques. However, these authors also concluded that nursing education needs to include more active lecture styles to strengthen the link between course content and clinical practice [ 12 ]. Ryan [ 10 ] introduced teaching strategies as extrinsic factors and found that teaching EBP and research methods may be more relevant if taught in a clinical context rather than using traditional didactic methods.
A mixed-methods meta-synthesis examining awareness and adoption of EBP stated that EBP skills for registered nurses and Bachelor of Science in Nursing (RN-to-BSN) students are influenced by exposure to partnerships and contextual teaching and learning, as well as clinical practice experience [ 13 ]. Teaching and learning strategies have included clinical practicum projects, lectures, small group work, post-clinical conferences, online modules and simulations [ 13 ]. EBP teachers who collaborate with their students, and nurses in clinical practice also influence students’ integration of EBP [ 2 ].
To ensure nursing students’ enhanced EBP knowledge, it is also essential to build partnerships with librarians who teach information literacy, which involves searching for relevant research in databases and evaluating and using that information in relation to course requirements and assignments [ 2 , 14 ]. Reported barriers to the adoption of EBP include difficulties with searching databases and evaluating research, feeling isolated from knowledgeable colleagues and the perception that there are minimal benefits from EBP. Countering these barriers, Phillips and Cullen [ 13 ] found that a variety of teaching and learning strategies may empower students’ implementation of EBP in clinical practice.
Emerson and Records’ [ 15 ] overview of scholarship and its role in nursing education includes a description of catalysts that enhance EBP in nursing and the knowledge necessary for EBP teaching. They state that scholarly teaching is an academic expectation; however, it does not appear to advance either the education or the discipline beyond the individual level. Indeed, nurses face challenges to EBP from their inability to locate and critically evaluate information [ 16 , 17 , 18 , 19 ].
The European Higher Education Area (EHEA) framework specifies expected learning outcomes for candidates with a Bachelor’s degree, including skills in finding, evaluating, referring and applying scientific information [ 20 ]. Likewise, the Code of Ethics of the International Council of Nurses stresses that nurses must be aware of and implement research results into their clinical practice [ 21 ]. Despite these guidelines, it appears that teaching EBP in nursing education varies among nurse educators and universities, and that clinical preceptors may have insufficient knowledge needed to support students [ 2 , 10 , 19 ]. Recent research indicates that nurses may not be well prepared to use EBP in their clinical practice [ 22 , 23 ].
There is a dearth of literature regarding the effect of teaching and learning strategies on implementing EBP in nursing education [ 10 , 13 , 23 , 24 ] and it is currently unclear whether implementation of EBP training leads to improved nursing practice [ 13 ].
In this literature review, we aimed to identify strategies for teaching EBP in undergraduate nursing education. The review questions were: “What teaching strategies are used to enhance knowledge and skills in EBP in undergraduate nursing education and what are the learning outcomes and barriers?”
Identification of studies
We conducted literature searches using Medline, Embase, CINAHL, Academic Search Premier and ERIC. The PICo framework for qualitative research was used to develop the review questions, plan the search and define the inclusion criteria. The population or participants assessed were nursing students, nursing education and nursing programmes. The phenomenon of interest was teaching and the specific context was EBP education. These concepts were transformed into the actual subject headings and text used in the search strategy in Medline (Table 1 ), which represents how the concepts were truncated and combined using Boolean and proximity operators in all database searches. The search criteria included qualitative studies published in English from 2006 through 2017. This range was chosen based on an initial search in PubMed PubReMiner indicating that most research on EBP training in nursing education was published since 2006, when EBP gained a foothold in nursing education. We examined the references cited in the retrieved studies, as well as studies in Google Scholar that cited the retrieved studies.
The inclusion criteria were: 1) original, qualitative research focused on EBP teaching strategies in undergraduate nursing education, i.e., we focused on qualitative research to gain a deeper insight into teacher and student experiences with these strategies; 2) peer-reviewed, original research; 3) studies on educators, student participation, or both; and 4) studies evaluated as moderate or high quality according to the Critical Appraisal Skills Programme (CASP) [ 25 ]. The exclusion criteria were: reviews, quantitative studies, theoretical studies and contributions that were not original research articles. Articles related to teaching strategies directed at health-care personnel, master programmes or postgraduate nursing education were also excluded.
We used the Preferred Reporting Items for Systematic Reviews and Meta-Analysis (PRISMA) [ 26 ] flowchart in the retrieval and selection process (Fig. 1 ) to identify 972 records from an initial database search and an additional 35 by manually searching those studies’ bibliographies. After duplicates were eliminated, we screened the abstracts of 724 articles. Of these, 708 articles did not meet our inclusion criteria, thus we obtained 16 full-text articles for further analysis. Each of the four authors examined all 16 articles, of which nine were excluded because of their low quality, focus on clinical intervention, or lack of focus on undergraduate nursing education. The final seven articles were included in the review.
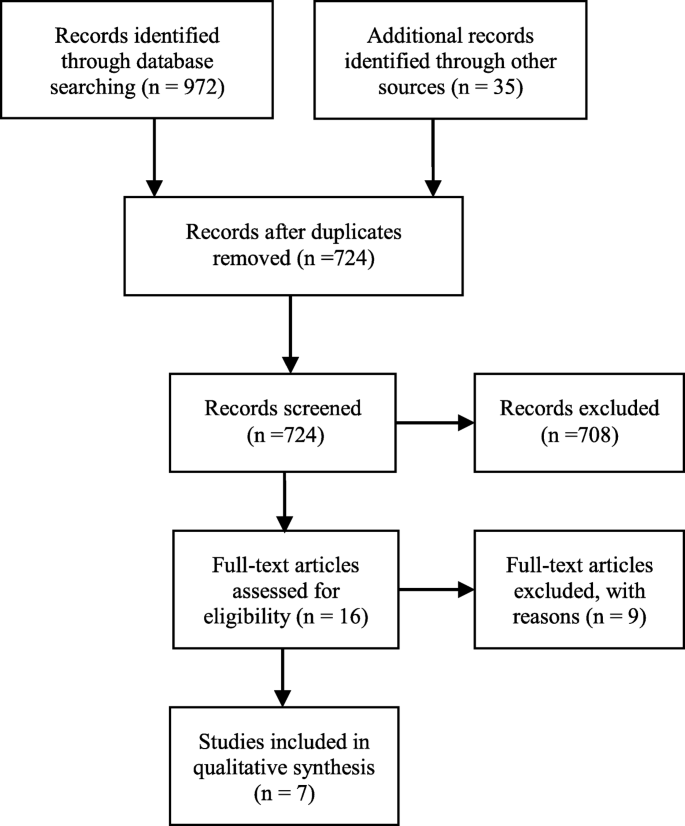
PRISMA flowchart of the screening and the assessment process
Critical appraisal
All four authors independently appraised the seven final articles for their methodological quality using CASP (Table 2 ), with moderate and high methodological quality defined as meeting 6–8 and 9–10 of the CASP checklist criteria, respectively. We discussed disagreements until consensus was reached.
A thematic analysis was conducted to identify themes based on the six phases described by Braun and Clarke [ 27 ], whose deductive approach refers to themes identified top down; in other words, we coded themes based on our specific review question. Although Braun and Clarke [ 27 ] recommend using narrative text, the included qualitative studies and mixed-methods study provided text-based data. In the first phase, all four authors familiarised themselves with the research by reading and rereading the data from each study. In the second phase, the first author carried out a systematic, manual coding of features that led to initial codes, before searching for themes in the third phase. Phase four involved reviewing the themes for correlation with the codes and identification of subthemes. After defining the themes in phase five, the findings were evaluated for relevance to the research question. The authors met several times to discuss the analysis process and to reach consensus on the labelling.
A summary of the studies and their findings are presented in Table 3 . The seven studies were conducted in Norway, the United Kingdom (UK), Sweden, Australia and Finland [ 28 , 29 , 30 , 31 , 32 , 33 ]. Qualitative data were also gathered from one mixed-methods study [ 34 ] conducted in the UK which, although using mixed methods, reported qualitative findings from students’ graffiti board comments and a focus group interview regarding lectures.
The four themes (and subthemes within each theme) were: 1) Interactive teaching strategies (Research utilisation, Information literacy and Assignments as learning activities); 2) Interactive and clinically integrated teaching strategies (Teaching EBP principles and Clinical integration and collaborations); 3) Learning outcomes (Enhancing analytical skills and Changing attitudes toward utilising research); and 4) Barriers (Information literacy skills and knowledge and Challenging collaboration).
Interactive teaching strategies
An improved understanding of the differences between quantitative and qualitative methods was highlighted as an important aspect of preparation for nursing practice [ 29 , 30 , 31 , 32 , 34 ]. Interactive strategies to teach the research process, critical appraisal and development of information literacy skills were also emphasised. Interactive learning activities such as problem-based learning, sharing information, flipped classroom and virtual simulation, workshops, group work and seminars with discussions were identified [ 30 , 33 , 34 ]. In some studies, oral presentations of students’ research findings in a clinical setting were highlighted as an important part of the teaching and learning strategy [ 28 , 32 , 34 ].
Research utilisation
Traditional teaching methods preparing students to use research were aimed at improving critical thinking skills, critically evaluating various literature sources and developing information literacy skills [ 30 , 31 , 32 , 34 ].
Group work was also identified as a teaching strategy for establishing research utilisation [ 28 , 30 , 34 ]. In the mixed-methods study [ 30 ], several workshops and monthly sessions were conducted to improve research competence among both lecturers and students.
Experiential learning was often supplemented by collaborative group learning, such as partnerships for learning course content [ 34 ]. The authors presented experiential teaching approaches as a motivational tool for improving research learning. The students used student-centred approaches and completed small group research studies. Assignments included carrying out a literature review, developing a proposal, facing a mock ethics committee, and collecting and analysing data. This student work was supported by pertinent lectures, including via ‘Blackboard’, a virtual learning platform. Finally, students presented their methodologic and analytic approaches on the virtual learning platform [ 34 ].
Information literacy
Teaching information literacy and interdisciplinary collaboration, especially with librarians, was emphasised as an important part of students’ learning how to find and use research [ 29 , 30 , 31 , 33 , 34 , 35 ]. In contrast, collaboration with librarians was not mentioned in Mattila and Eriksson’s [ 32 ] study.
Friberg and Lyckhage’s [ 30 ] study emphasised the significance of research utility and disseminating research results. Cader et al. [ 29 ] revealed differences in students’ knowledge of computer and information literacy skills. In one study, differences appear to have been influenced by the role of the library in supporting nursing students, curriculum content and emphasis, and interaction with lecturers and peers [ 33 ]. Nurse educators indicated a need for staff development and a progressive approach to the curriculum to ensure students’ understanding of IL and its links to learning [ 33 ].
An environment supportive of the learning process promoted change and development. Collaboration with and facilitation and guidance by academic and library staff was considered essential for a successful process and outcome [ 29 , 33 ]. It was also clear from these studies that nursing students need greater support to access, use and evaluate information fully [ 29 , 32 , 33 ].
Assignments as learning activities
Course assignments were included as a part of the learning process in all evaluated studies, which included activities preparing students to use research or enhance their EBP knowledge and skills. Assignments that were integrated into clinical practice were particularly emphasised in the studies that focused on teaching EBP principles [ 28 , 29 , 31 ].
An assignment focusing on analysis of health needs was undertaken to help student nurses gain an understanding of the relevance of EBP [ 29 ]. Nursing students were found to require further development of their critical appraisal skills and further improvement of the guidance from both academics and librarians was needed [ 29 ].
Friberg and Lyckhage [ 30 ] emphasised essay writing as a learning tool and used different literature-based research methods to meet this goal.
Interactive and clinically integrated teaching strategies
The thematic analysis identified interactive and clinically integrated teaching strategies. Interactive clinical strategies included assignments based on collaboration with health-care personnel in clinical practice. Learning activities with oral presentations of the findings from the students’ studies delivered in their clinical work settings were also mentioned [ 28 , 32 ].
Teaching EBP principles
A focus on teaching the six EBP steps was evident in the studies by André et al. [ 28 ], Cader et al. [ 29 ] and Malik et al. [ 31 ]. Research utilisation was emphasised in these reports. There was a vague focus on EBP principles in three of the studies [ 30 , 32 , 33 ] and integrated teaching activities to teach clinical strategies were described in four of the studies [ 28 , 29 , 31 , 32 ].
Clinical integration and collaboration
In the study by Malik et al. [ 31 ], students participated in clinical projects and analysed data with researchers. Clinical experts were also engaged in the lectures.
Cader et al. [ 29 ] emphasised the benefit of students carrying out analyses of health needs through collaboration within the clinical practice context. To this end, nursing students conducted ‘mini’ research projects including an analysis of the health needs of a particular patient group with a common problem or diagnosis. Although the nursing students found the assignment challenging and time consuming, they also considered it meaningful because accessing information about health needs made the evidence relevant.
Mattila and Eriksson [ 32 ] outlined a learning assignment conducted during a six-week clinical practice period in which students chose topics aimed at utilising research and enhancing their competence in the clinical practice context. The clinical instructor approved a selected research article that was applicable to clinical practice and the nursing students orally presented their findings to fellow students and staff at their clinical practice placement.
A Norwegian pilot study by André et al. [ 28 ] focused on participation and cooperation in clinical research projects, which nursing students specified was a motivation for learning EBP. These students strongly appreciated working with experienced nurses on their clinical projects.
Learning outcomes
Students expressed that writing assignments helped them understand the research process. Based on the nursing students’ reports, they were motivated by being able to choose topics that were of interest to them [ 29 , 32 , 34 ]. Learning outcomes from teaching strategies were presented in most of the studies we evaluated, and it was from these outcomes that the Enhancing analytical skills and Increased awareness of using research subthemes were identified.
Enhancing analytical skills
Nursing students reported learning enhanced analytical and critical thinking skills, and some of the findings were outcomes of specific assignments and teaching strategies [ 28 , 29 , 30 , 34 ]. Students experienced learning outcomes and thus acknowledged the importance of research utilisation to their future clinical practice. It was emphasised in the reports that these students considered their key roles to be research consumers rather than producers [ 28 , 29 , 30 , 32 , 34 ]. Students also developed a greater awareness of the core role of nursing and that use of research is imperative in the nursing profession.
Based on the assignments they were given, the students in these studies reported learning outcomes such as understanding how to apply relevant evidence to everyday clinical practice. In this way, they learned to link research to health needs [ 28 , 29 , 30 ]. Mattila and Eriksson [ 32 ] reported that nursing students gained greater insight into their future profession. That academic presentations and discussions inspired them to search for research was considered ‘meaningful’.
Although nursing students considered themselves prepared to use research, Friberg and Lyckhage [ 30 ] emphasised that students are insufficiently skilled to assess research critically. This perspective is consistent with the findings by Cader et al. [ 29 ] that there is a need for further support for developing students’ critical evaluation skills.
Some students emphasised the importance of bringing together clinical practice, their own practical experiences and the research context. They experienced EBP as a platform to facilitate the development of their curiosity and critical reflection within clinical practice [ 28 ].
Changing attitudes toward utilising research
Nursing students reported research awareness as a learning outcome associated with information gathering and improved information literacy skills [ 29 , 30 ]. Despite completing acourse, students in one study stated that they had neither a comprehensive understanding of the information literacy concept nor improved skills [ 33 ]. Computer and information literacy skills apparently vary among both lecturers and students [ 33 , 35 ]. However, in several of the studies, increased awareness and understanding of research appeared to be an important learning outcome of information literacy teaching strategies for nursing students [ 29 , 30 , 32 , 34 ].
Generating an awareness of how to critically evaluate research evidence rather than producing research is necessary for implementing EBP. To obtain this awareness, it is crucial to find creative ways of guiding undergraduate nursing students to find and critically appraise research reports [ 30 ]. These studies emphasised nursing students’ increased awareness that implementing nursing research in clinical practice is a prerequisite to providing safer patient care [ 28 , 29 , 30 , 32 ].
Barriers to acquiring EBP and research utilisation skills were divided into two subthemes: i.e., information literacy skills and knowledge, and Challenging collaborations.
Information literacy skills and knowledge
Discontinuity of information literacy content throughout the curriculum seems to constitute a barrier to searching for and finding research [ 33 ]. In addition, some academics reported their own limited awareness of EBP teaching strategies [ 31 ].
Nursing students reported finding it challenging to find and interpret research. They were dependent on assistance from librarians and lecturers [ 32 , 33 ]. The need for more interdisciplinary support to teach information literacy skills was also emphasised in several studies [ 29 , 32 , 33 , 35 ]. When integrating EBP, it was challenging for academic nurses to implement innovative teaching strategies because they lacked knowledge, had a large workload or had insufficient time and resources to study new strategies [ 31 ].
Challenging collaboration
In one study, group work was interpreted as a barrier to learning EBP [ 34 ], which demonstrated that dysfunctional group dynamics can negatively affect the learning process. In contrast, in the same study, some students reported positive teamwork experiences that were motivating and enhanced their learning process [ 34 ]. In the study by Malik et al. [ 31 ], the academic educators reported that their students loved workshops on searching databases. Some nursing students reported that their clinical practice status made it difficult to gather the information required for their assignments [ 29 ].
The findings from this initial review demonstrate that various interactive teaching strategies have been emphasised to enhance knowledge and utilise research. However, despite being recommended strategies [ 3 , 14 , 36 ], factors such as teaching strategies that include clinical activities to develop EBP knowledge and skills seem to be given a lower priority. This review identified that self-reports and evaluations show that nursing students report development of critical thinking skills as a learning outcome of various teaching strategies [ 28 , 29 , 30 , 34 ], which is consistent with earlier studies [ 16 , 17 , 18 ]. In contrast, barriers to enhancing students’ EBP knowledge and skills included a weak understanding of information literacy and difficulties finding and interpreting research.
All analysed studies herein reported at least some use of interactive teaching strategies. Patient safety and quality of care in Western society require that future nurses have EBP knowledge, which means that they must use available research as well as patients’ preferences and their own clinical expertise in decision-making processes [ 14 , 36 ]. We identified studies that emphasised teaching strategies specifically aimed at finding research, critical appraisal and research utilisation through interactive methods [ 30 , 32 , 33 ]. However, it may be challenging for future nurses to obtain sound EBP knowledge if teaching strategies are mainly focused on research utilisation. A commission of health-care professionals and academic leaders presented their vision and common strategy toward strengthening global health-care systems, which argued that cross-professional collaboration in education is a powerful instrument for improving health-care outcomes [ 37 ]. Guiding principles, such as the code of ethics, the EHEA framework for expected learning outcomes [ 20 , 21 ] and health legislation emphasise wider use of the best research evidence in nursing practice, which may explain why teaching strategies are primarily directed at research utilisation. Information literacy skills are important to EBP; however, studies show that nurses and nursing students lack these skills [ 17 , 18 , 38 , 39 , 40 ].
Clinically integrated teaching strategies
In the present review, three studies [ 28 , 29 , 32 ] focused on clinically integrated teaching strategies in particular. The relationships between the clinical practice context and health needs analysis [ 29 ] were emphasised in a six-week clinical practice assignment, using oral presentation as a learning activity [ 32 ] and participation in clinical research projects [ 28 ].
Ryan [ 10 ] identified that learning EBP would have greater relevance for students if teaching strategies took place in a clinical setting. According to Llasus et al. [ 38 ], knowledge translation from education to clinical practice is challenging. These authors argue that if nursing students are expected to be able to implement EBP in clinical practice, they must have both EBP knowledge and EBP ‘readiness’, which requires strengthening their confidence in EBP.
Phillips and Cullen [ 13 ] observed that development of EBP skills for RN-to-BSN students was influenced by exposure to educational partnerships, contextual teaching and learning, and clinical practice experience. However, the findings from a Norwegian study in physiotherapy students reported a lack of both EBP culture and role models in their clinical practice [ 41 ].
A systematic review showed that EBP knowledge in medicine is increasing, irrespective of whether or not it is provided at undergraduate or postgraduate levels. Indeed, learning outcomes appear more effective if the teaching strategies are connected to clinical practice [ 42 ]. This notion was emphasised in the core clinical evaluation criteria developed in the Delphi Study by Bostwick and Linden [ 43 ]. In contrast, Ilic and Maloney [ 44 ] found no difference in learning outcomes. Despite the variety of teaching strategies across the studies we reviewed, they cumulatively show good evidence that any form of teaching EBM increases knowledge.
The findings from this review demonstrate that collaboration through clinical practice and patient care appears to be a relatively low priority. Patients’ preferences are not explicitly considered, despite an increased focus on seeing the patient as a collaborative partner in the EBP paradigm, ethical guidelines and legislation on education and health [ 2 , 3 , 20 , 21 ]. This is also contrary to recommendations about the factors that influence EBP skills, such as contextual teaching and learning and practical experience opportunities [ 13 ].
Becoming more analytical
It is worth mentioning that the nursing students in some of the studies included in this review increased their analytical skills because of EBP teaching strategies [ 28 , 29 , 30 , 34 ], regardless of whether the teaching focused exclusively on interactive or targeted both interactive and clinical strategies. However, research has shown that nursing students have inadequate knowledge to make them capable of judging, reflecting on and critically assessing research [ 10 ]. Becoming more analytical and changing attitudes towards utilising research in clinical situations may be essential for nurses in their future careers and could contribute to increased patient safety. These skills may lead to nurses with a higher level of analytical skills and clinical judgment, who have a greater ability to reflect and reason.
Course assignments as a teaching and learning strategy
According to the review findings, a variety of course assignments promote EBP knowledge and skills. Choosing topics of interest to students motivates them to develop EBP knowledge [ 29 , 32 , 34 ]. Several studies argue that assignments are essential for self-directed, continuous learning [ 18 , 38 , 39 , 40 ].

Methodological limitations
There are some limitations to this review. We used a relatively small sample of articles and excluded non-English language studies, which may have caused us to overlook some studies on enhancing EBP skills and knowledge in nursing education. However, to ensure a systematic search process, the literature search was performed by AN, an academic librarian. In addition, our use of several databases likely decreased the possibility of selection bias. The six qualitative studies included in this study were homogeneous in terms of their qualitative research design and meeting our inclusion criteria. Qualitative data from the mixed-methods study that addressed our research question was also included. Variations such as cultural diversity and differences in participant perspectives may also have affected the analyses in these studies. Despite these limitations, we met our goal of examining teaching strategies, learning outcomes and barriers in undergraduate nursing education, from the perspectives of both educators and students.
Conclusions
Insufficient attention has been paid to the use of EBP principles in nursing education. The teaching strategies identified in the represented studies show that interactive teaching strategies are used alongside traditional lectures to enhance research utilisation skills in nursing education. However, collaboration with clinical practice to enhance EBP knowledge was only vaguely addressed in most of these studies. In conclusion, there is a need to improve educators’ consciousness of and competences in teaching EBP principles, which involves using interactive and clinical integrated teaching strategies. Only seven studies met criteria for inclusion in this review, indicating that further targeted qualitative research is needed.
Abbreviations
Bachelor Nurse
Critical Appraisal Skills Programme
Evidence-Based Medicine
Evidence-Based Practice
European Higher Education Area
Information Literacy
Population Interest Context
Preferred Reporting Items for Systematic Reviews and Meta-Analysis
Registered Nurses and Bachelor of Science in Nursing
United Kingdom
Straus SE, Richardson WS, Glasziou P, Haynes RB. Evidence-based medicine: how to practice and teach it. Edinburgh: Churchill Livingstone/Elsevier; 2011.
Google Scholar
Fineout-Overholt E, Stillwell SB, Williamson KM, Cox JF III, Robbins BW. Teaching evidence-based practice in academic settings. In: Melnyk BM, Fineout-Overholt E, editors. Evidence-based practice in nursing & healthcare: a guide to best practice. Philadelphia: Wolters Kluwer/Lippincott Williams & Wilkins; 2011. p. 291–329.
Khan KS, Coomarasamy A. A hierarchy of effective teaching and learning to acquire competence in evidenced-based medicine. BMC Med Educ. 2006;6:59.
Article Google Scholar
Levin RF. Integrating evidence-based practice with educational theory in clinical practice for nurse practitioners: bridging the theory practice gap. Res Theory Nurs Pract. 2010;24:213–6.
McCurry MK, Martins DC. Teaching undergraduate nursing research: a comparison of traditional and innovative approaches for success with millennial learners. J Nurs Educ. 2010;49:276–9.
Montenery MS, Walker MM, Sorensen ME, Thompson MR, Kirklin MD, White MR, et al. Millennial generation student nurses’ perceptions of the impact of multiple technologies on learning. Nurs Educ Perspect. 2013;34:405–9.
Young T, Rohwer A, Volmink J, Clarke M. What are the effects of teaching evidence-based health care (EBHC)? Overview of systematic reviews. PLoS One. 2014;9:e86706.
Fiset VJ, Graham ID, Davies BL. Evidence-based practice in clinical nursing education: a scoping review. J Nurs Educ. 2017;56:534–41.
Häggman-Laitila A, Mattila LR, Melender HL. Educational interventions on evidence-based nursing in clinical practice: a systematic review with qualitative analysis. Nurse Educ Today. 2016;43:50–9.
Ryan EJ. Undergraduate nursing students’ attitudes and use of research and evidence-based practice - an integrative literature review. J Clin Nurs. 2016;25:1548–56.
Johnson N, List-Ivankovic J, Eboh WO, Ireland J, Adams D, Mowatt E, et al. Research and evidence based practice: using a blended approach to teaching and learning in undergraduate nurse education. Nurse Educ Pract. 2010;10:43–7.
Crookes K, Crookes PA, Walsh K. Meaningful and engaging teaching techniques for student nurses: a literature review. Nurse Educ Pract. 2013;13:239–43.
Phillips JM, Cullen D. Improving the adoption of evidence-based practice through RN-to-BSN education. J Contin Educ Nurs. 2014;45:467–72.
Melnyk BM, Fineout-Overholt E. Making the case for evidence-based practice and cultivating a spirit of inquiry. In: Melnyk BM, Fineout-Overholt E, editors. Evidence-based practice in nursing and healthcare: a guide to best practice. Philadelphia: Wolters Kluwer/Lippincott Williams & Wilkins; 2011. p. 3–24.
Emerson RJ, Records K. Today’s challenge, tomorrow’s excellence: the practice of evidence-based education. J Nurs Educ. 2008;47:359–70.
Barnard A, Nash R, O’Brien M. Information literacy: developing lifelong skills through nursing education. J Nurs Educ. 2005;44:505–10.
Duncan V, Holtslander L. Utilizing grounded theory to explore the information-seeking behavior of senior nursing students. J Med Libr Assoc. 2012;100:20–7.
Klem ML, Weiss PM. Evidence-based resources and the role of librarians in developing evidence-based practice curricula. J Prof Nurs. 2005;21:380–7.
Florin J, Ehrenberg A, Wallin L, Gustavsson P. Educational support for research utilization and capability beliefs regarding evidence-based practice skills: a national survey of senior nursing students. J Adv Nurs. 2012;68:888–97.
Ministry of Education and Research. Norwegian qualifications framework: levels and learning outcome descriptors; 2011. https://www.regjeringen.no/contentassets/e579f913fa1d45c2bf2219afc726670b/nkr.pdf Accessed 15 May 2018.
International Council of Nurses (ICN). ICN code of ethics for nurses. Geneva: ICN; 2012. http://www.icn.ch/images/stories/documents/about/icncode_english.pdf . Accessed 15 May 2018
Saunders H, Stevens KR, Vehviläinen-Julkunen K. Nurses’ readiness for evidence-based practice at Finnish university hospitals: a national survey. J Adv Nurs. 2016;72:1863–74.
Saunders H, Vehviläinen-Julkunen K. The state of readiness for evidence-based practice among nurses: an integrative review. Int J Nurs Stud. 2016;56:128–40.
Alqahtani N. The effect of different learning strategies on nursing students’ knowledge and attitudes towards the use of evidence-based practice: a systematic review. Int J Nurs Health Sci. 2015;2:83–90.
Critical Appraisal Skills Programme. Making sense of evidence about clinical effectiveness. 10 questions to help you make sense of qualitative research. Oxford: CASP; 2018. https://casp-uk.net/wp-content/uploads/2018/01/CASP-Qualitative-Checklist.pdf . Accessed 15 May 2018
Moher D, Liberati A, Tetzlaff J, Altmann D, PRISMA Group. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Phys Ther. 2009;89:873–80.
Braun V, Clarke V. Using thematic analysis in psychology. Qual Res Psychol. 2006;3:77–101.
André B, Aune AG, Brænd JA. Embedding evidence-based practice among nursing undergraduates: results from a pilot study. Nurse Educ Pract. 2016;18:30–5.
Cader R, Derbyshire J, Smith AG, Gannon-Leary P, Walton G. In search of evidence: a small scale study exploring how student nurses accessed information for a health needs assignment. Nurse Educ Today. 2006;26:403–8.
Friberg F, Lyckhage ED. Changing essay writing in undergraduate nursing education through action research: a Swedish example. Nurs Educ Perspect. 2013;34:226–32.
Malik G, McKenna L, Griffiths D. Using pedagogical approaches to influence evidence-based practice integration – processes and recommendations: findings from a grounded theory study. J Adv Nurs. 2017;73:883–93.
Mattila L-R, Eriksson E. Nursing students learning to utilize nursing research in clinical practice. Nurse Educ Today. 2007;27:568–76.
Nayda R, Rankin E. Information literacy skill development and life long learning: exploring nursing students’ and academics’ understandings. Aust J Adv Nurs. 2008;26:27–33.
Irvine F, Gracey C, Jones OS, Roberts JL, Tamsons RE, Tranter S. Research awareness: making learning relevant for pre-registration nursing students. Nurse Educ Pract. 2008;8:267–75.
McNeil BJ, Elfrink V, Beyea SC, Pierce ST, Bickford CJ. Computer literacy study: report of qualitative findings. J Prof Nurs. 2006;22:52–9.
DiCenso A, Guyatt G, Ciliska D. Evidence-based nursing: a guide to clinical practice. St. Louis: Elsevier Mosby; 2005.
Frenk J, Bhutta ZA, Chen LC-H, Cohen J, Crisp N, Evans T, et al. Health professionals for a new century: transforming education to strengthen health systems in an interdependent world. Lancet. 2010;376:1923–58.
Llasus L, Angosta AD, Clark M. Graduating baccalaureate students’ evidence-based practice knowledge, readiness, and implementation. J Nurs Educ. 2014;53:S82–9.
Mittermeyer D. Incoming first year undergraduate students: how information literate are they? Educ Inf. 2005;23:203–32.
Ragneskog H, Gerdner L. Competence in nursing informatics among nursing students and staff at a nursing institute in Sweden. Health Inf Libr J. 2006;23:126–32.
Olsen NR, Bradley P, Lomborg K, Nortvedt MW. Evidence based practice in clinical physiotherapy education: a qualitative interpretive description. BMC Med Educ. 2013;13:52.
Ilic D. Teaching evidence-based practice: perspectives from the undergraduate and post-graduate viewpoint. Ann Acad Med Singap. 2009;38:559–63.
Bostwick L, Linden L. Evaluation criteria for nursing student application of evidence-based practice: a Delphi study. J Nurs Educ. 2016;55:336–41.
Ilic D, Maloney S. Methods of teaching medical trainees evidence-based medicine: a systematic review. Med Educ. 2014;48:124–35.
Download references
Acknowledgements
The authors acknowledge The University of South-Eastern Norway, Faculty of Health and Social Sciences for supporting this research.
The University of South-Eastern Norway, Faculty of Health and Social Sciences supported this research.
Availability of data and materials
Not applicable. All studies included in this review can be sourced online.
Author information
Authors and affiliations.
Faculty of Health and Social Sciences, the Department of Nursing and Health Sciences, University of South-Eastern Norway, P.O. Box 235, N-3603, Kongsberg, Norway
May-Elin T. Horntvedt & Torbjørg Fermann
Department of Research and Internationalisation, University of South-Eastern Norway, P.O. Box 235, N-3603, Kongsberg, Norway
Anita Nordsteien
Centre for Women’s, Family and Child Health, Faculty of Health and Social Sciences, University of South-Eastern Norway, P.O. Box 235, N-3603, Kongsberg, Norway
Elisabeth Severinsson
You can also search for this author in PubMed Google Scholar
Contributions
METH was the lead author who planned and implemented the study in close collaboration with AN, TF and ES. AN predominantly carried out the literature research. All authors collaborated on analyses. ES provided substantial support for the study as an expert in qualitative research. METH drafted the manuscript. All authors provided critical comments on the manuscript and have approved the final version.
Corresponding author
Correspondence to May-Elin T. Horntvedt .
Ethics declarations
Ethics approval and consent to participate.
Not applicable.
Consent for publication
Competing interests.
The authors declare that they have no competing interests.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License ( http://creativecommons.org/licenses/by/4.0/ ), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated.
Reprints and permissions
About this article
Cite this article.
Horntvedt, ME.T., Nordsteien, A., Fermann, T. et al. Strategies for teaching evidence-based practice in nursing education: a thematic literature review. BMC Med Educ 18 , 172 (2018). https://doi.org/10.1186/s12909-018-1278-z
Download citation
Received : 17 January 2018
Accepted : 13 July 2018
Published : 28 July 2018
DOI : https://doi.org/10.1186/s12909-018-1278-z
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Teaching strategies
- Evidence-based practice
- Nursing education
- Learning outcome
BMC Medical Education
ISSN: 1472-6920
- General enquiries: [email protected]
Log in using your username and password
- Search More Search for this keyword Advanced search
- Latest content
- Current issue
- Write for Us
- BMJ Journals
You are here
- Volume 22, Issue 1
- How to appraise qualitative research
- Article Text
- Article info
- Citation Tools
- Rapid Responses
- Article metrics
- Calvin Moorley 1 ,
- Xabi Cathala 2
- 1 Nursing Research and Diversity in Care, School of Health and Social Care , London South Bank University , London , UK
- 2 Institute of Vocational Learning , School of Health and Social Care, London South Bank University , London , UK
- Correspondence to Dr Calvin Moorley, Nursing Research and Diversity in Care, School of Health and Social Care, London South Bank University, London SE1 0AA, UK; Moorleyc{at}lsbu.ac.uk
https://doi.org/10.1136/ebnurs-2018-103044
Statistics from Altmetric.com
Request permissions.
If you wish to reuse any or all of this article please use the link below which will take you to the Copyright Clearance Center’s RightsLink service. You will be able to get a quick price and instant permission to reuse the content in many different ways.
Introduction
In order to make a decision about implementing evidence into practice, nurses need to be able to critically appraise research. Nurses also have a professional responsibility to maintain up-to-date practice. 1 This paper provides a guide on how to critically appraise a qualitative research paper.
What is qualitative research?
- View inline
Useful terms
Some of the qualitative approaches used in nursing research include grounded theory, phenomenology, ethnography, case study (can lend itself to mixed methods) and narrative analysis. The data collection methods used in qualitative research include in depth interviews, focus groups, observations and stories in the form of diaries or other documents. 3
Authenticity
Title, keywords, authors and abstract.
In a previous paper, we discussed how the title, keywords, authors’ positions and affiliations and abstract can influence the authenticity and readability of quantitative research papers, 4 the same applies to qualitative research. However, other areas such as the purpose of the study and the research question, theoretical and conceptual frameworks, sampling and methodology also need consideration when appraising a qualitative paper.
Purpose and question
The topic under investigation in the study should be guided by a clear research question or a statement of the problem or purpose. An example of a statement can be seen in table 2 . Unlike most quantitative studies, qualitative research does not seek to test a hypothesis. The research statement should be specific to the problem and should be reflected in the design. This will inform the reader of what will be studied and justify the purpose of the study. 5
Example of research question and problem statement
An appropriate literature review should have been conducted and summarised in the paper. It should be linked to the subject, using peer-reviewed primary research which is up to date. We suggest papers with a age limit of 5–8 years excluding original work. The literature review should give the reader a balanced view on what has been written on the subject. It is worth noting that for some qualitative approaches some literature reviews are conducted after the data collection to minimise bias, for example, in grounded theory studies. In phenomenological studies, the review sometimes occurs after the data analysis. If this is the case, the author(s) should make this clear.
Theoretical and conceptual frameworks
Most authors use the terms theoretical and conceptual frameworks interchangeably. Usually, a theoretical framework is used when research is underpinned by one theory that aims to help predict, explain and understand the topic investigated. A theoretical framework is the blueprint that can hold or scaffold a study’s theory. Conceptual frameworks are based on concepts from various theories and findings which help to guide the research. 6 It is the researcher’s understanding of how different variables are connected in the study, for example, the literature review and research question. Theoretical and conceptual frameworks connect the researcher to existing knowledge and these are used in a study to help to explain and understand what is being investigated. A framework is the design or map for a study. When you are appraising a qualitative paper, you should be able to see how the framework helped with (1) providing a rationale and (2) the development of research questions or statements. 7 You should be able to identify how the framework, research question, purpose and literature review all complement each other.
There remains an ongoing debate in relation to what an appropriate sample size should be for a qualitative study. We hold the view that qualitative research does not seek to power and a sample size can be as small as one (eg, a single case study) or any number above one (a grounded theory study) providing that it is appropriate and answers the research problem. Shorten and Moorley 8 explain that three main types of sampling exist in qualitative research: (1) convenience (2) judgement or (3) theoretical. In the paper , the sample size should be stated and a rationale for how it was decided should be clear.
Methodology
Qualitative research encompasses a variety of methods and designs. Based on the chosen method or design, the findings may be reported in a variety of different formats. Table 3 provides the main qualitative approaches used in nursing with a short description.
Different qualitative approaches
The authors should make it clear why they are using a qualitative methodology and the chosen theoretical approach or framework. The paper should provide details of participant inclusion and exclusion criteria as well as recruitment sites where the sample was drawn from, for example, urban, rural, hospital inpatient or community. Methods of data collection should be identified and be appropriate for the research statement/question.
Data collection
Overall there should be a clear trail of data collection. The paper should explain when and how the study was advertised, participants were recruited and consented. it should also state when and where the data collection took place. Data collection methods include interviews, this can be structured or unstructured and in depth one to one or group. 9 Group interviews are often referred to as focus group interviews these are often voice recorded and transcribed verbatim. It should be clear if these were conducted face to face, telephone or any other type of media used. Table 3 includes some data collection methods. Other collection methods not included in table 3 examples are observation, diaries, video recording, photographs, documents or objects (artefacts). The schedule of questions for interview or the protocol for non-interview data collection should be provided, available or discussed in the paper. Some authors may use the term ‘recruitment ended once data saturation was reached’. This simply mean that the researchers were not gaining any new information at subsequent interviews, so they stopped data collection.
The data collection section should include details of the ethical approval gained to carry out the study. For example, the strategies used to gain participants’ consent to take part in the study. The authors should make clear if any ethical issues arose and how these were resolved or managed.
The approach to data analysis (see ref 10 ) needs to be clearly articulated, for example, was there more than one person responsible for analysing the data? How were any discrepancies in findings resolved? An audit trail of how the data were analysed including its management should be documented. If member checking was used this should also be reported. This level of transparency contributes to the trustworthiness and credibility of qualitative research. Some researchers provide a diagram of how they approached data analysis to demonstrate the rigour applied ( figure 1 ).
- Download figure
- Open in new tab
- Download powerpoint
Example of data analysis diagram.
Validity and rigour
The study’s validity is reliant on the statement of the question/problem, theoretical/conceptual framework, design, method, sample and data analysis. When critiquing qualitative research, these elements will help you to determine the study’s reliability. Noble and Smith 11 explain that validity is the integrity of data methods applied and that findings should accurately reflect the data. Rigour should acknowledge the researcher’s role and involvement as well as any biases. Essentially it should focus on truth value, consistency and neutrality and applicability. 11 The authors should discuss if they used triangulation (see table 2 ) to develop the best possible understanding of the phenomena.
Themes and interpretations and implications for practice
In qualitative research no hypothesis is tested, therefore, there is no specific result. Instead, qualitative findings are often reported in themes based on the data analysed. The findings should be clearly linked to, and reflect, the data. This contributes to the soundness of the research. 11 The researchers should make it clear how they arrived at the interpretations of the findings. The theoretical or conceptual framework used should be discussed aiding the rigour of the study. The implications of the findings need to be made clear and where appropriate their applicability or transferability should be identified. 12
Discussions, recommendations and conclusions
The discussion should relate to the research findings as the authors seek to make connections with the literature reviewed earlier in the paper to contextualise their work. A strong discussion will connect the research aims and objectives to the findings and will be supported with literature if possible. A paper that seeks to influence nursing practice will have a recommendations section for clinical practice and research. A good conclusion will focus on the findings and discussion of the phenomena investigated.
Qualitative research has much to offer nursing and healthcare, in terms of understanding patients’ experience of illness, treatment and recovery, it can also help to understand better areas of healthcare practice. However, it must be done with rigour and this paper provides some guidance for appraising such research. To help you critique a qualitative research paper some guidance is provided in table 4 .
Some guidance for critiquing qualitative research
- ↵ Nursing and Midwifery Council . The code: Standard of conduct, performance and ethics for nurses and midwives . 2015 https://www.nmc.org.uk/globalassets/sitedocuments/nmc-publications/nmc-code.pdf ( accessed 21 Aug 18 ).
- Barrett D ,
- Cathala X ,
- Shorten A ,
Patient consent for publication Not required.
Competing interests None declared.
Provenance and peer review Commissioned; internally peer reviewed.
Read the full text or download the PDF:
Evidence-Based Practice Essay
The purpose of this study is to demonstrate the use of evidence-based practice in answering a PICO question: “Do stimulants increase academic performance in university students?” Drawing references from peer-reviewed articles, this study will illustrate how clinical decisions are made from the inferences acquired from the literature sources. Through demonstrating an understanding of the principles of evidence-based practice, the paper will prove the validity of the statement by Khalil (2017) that it is imperative to evaluate and apply evidence-based practice in improving the quality of healthcare.
This study adopts a quantitative research design in which the researchers used a sample of eighteen healthy university students to report on the non medical use of elicit and prescription stimulants for enhancing academic performance. The data was collected through face to face interview. The methodology and methods of research were appropriate to course of the study since the researchers had a large sample size which guaranteed the generalization of the research findings.
Munro, B., Weyandt, L., Marraccini, M., & Oster, D. (2017). The relationship between nonmedical use of prescription stimulants, executive functioning and academic outcomes. Addictive Behaviors, 65, 250-257. http://dx.doi.org/10.1016/j.addbeh.2016.08.023

Barriers for the Application of Evidence in Practice
How closely the research studies provided align with the pico question.
1. Barclay, L. (2012). Evidence: Making an impact. International Journal of Evidence-Based Healthcare, 10(1), 1-2. http://dx.doi.org/10.1111/j.1744-1609.2012.00258.x
2. Bergstrom, N. (2008). The gap between discovery and practice implementation in evidence-based practice. International Journal of Evidence-Based Healthcare, 6(2), 135-136. http://dx.doi.org/10.1097/01258363-200806000-00001
3. Frewin, D. (2014). The International Journal of Evidence-Based Healthcare – Quo vadis? International Journal of Evidence-Based Healthcare, 12(1), 1-2. http://dx.doi.org/10.1097/xeb.0000000000000000
4. Frewin, D., & Court, A. (2009). Elements of evidence-based healthcare. International Journal of Evidence-Based Healthcare, 7(1), 1-2. http://dx.doi.org/10.1111/j.1744-1609.2009.00125.x
5. Hildt, E., Lieb, K., & Franke, A. (2014). Life context of pharmacological academic performance enhancement among university students – A qualitative approach. BMC Medical Ethics, 15(1). http://dx.doi.org/10.1186/1472-6939-15-23
6. Khalil, H. (2017). Evidence-based quality improvement. International Journal of Evidence-Based Healthcare, 15(3), 81. http://dx.doi.org/10.1097/xeb.0000000000000118
7. Munro, B., Weyandt, L., Marraccini, M., & Oster, D. (2017). The relationship between nonmedical use of prescription stimulants, executive functioning and academic outcomes. Addictive Behaviors, 65, 250-257. http://dx.doi.org/10.1016/j.addbeh.2016.08.023
8. Tan, M. (2013). Mentoring nurses in evidence-based projects. International Journal of Evidence-Based Healthcare, 11(3), 252-253. http://dx.doi.org/10.1097/01258363-201309000-00081
- AACN Synergy Model
- Advanced Practice Nurse (ADN)
- American Nurses’ Association (ANA)
- Communication

Warning: The NCBI web site requires JavaScript to function. more...
An official website of the United States government
The .gov means it's official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you're on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
- Browse Titles
NCBI Bookshelf. A service of the National Library of Medicine, National Institutes of Health.
Hughes RG, editor. Patient Safety and Quality: An Evidence-Based Handbook for Nurses. Rockville (MD): Agency for Healthcare Research and Quality (US); 2008 Apr.

Patient Safety and Quality: An Evidence-Based Handbook for Nurses.
Chapter 7 the evidence for evidence-based practice implementation.
Marita G. Titler .
Affiliations
Overview of evidence-based practice.
Evidence-based health care practices are available for a number of conditions such as asthma, heart failure, and diabetes. However, these practices are not always implemented in care delivery, and variation in practices abound. 1–4 Traditionally, patient safety research has focused on data analyses to identify patient safety issues and to demonstrate that a new practice will lead to improved quality and patient safety. 5 Much less research attention has been paid to how to implement practices. Yet, only by putting into practice what is learned from research will care be made safer. 5 Implementing evidence-based safety practices are difficult and need strategies that address the complexity of systems of care, individual practitioners, senior leadership, and—ultimately—changing health care cultures to be evidence-based safety practice environments. 5
Nursing has a rich history of using research in practice, pioneered by Florence Nightingale. 6–9 Although during the early and mid-1900s, few nurses contributed to this foundation initiated by Nightingale, 10 the nursing profession has more recently provided major leadership for improving care through application of research findings in practice. 11
Evidence-based practice (EBP) is the conscientious and judicious use of current best evidence in conjunction with clinical expertise and patient values to guide health care decisions. 12–15 Best evidence includes empirical evidence from randomized controlled trials; evidence from other scientific methods such as descriptive and qualitative research; as well as use of information from case reports, scientific principles, and expert opinion. When enough research evidence is available, the practice should be guided by research evidence in conjunction with clinical expertise and patient values. In some cases, however, a sufficient research base may not be available, and health care decision making is derived principally from nonresearch evidence sources such as expert opinion and scientific principles. 16 As more research is done in a specific area, the research evidence must be incorporated into the EBP. 15
Models of Evidence-Based Practice
Multiple models of EBP are available and have been used in a variety of clinical settings. 16–36 Although review of these models is beyond the scope of this chapter, common elements of these models are selecting a practice topic (e.g., discharge instructions for individuals with heart failure), critique and syntheses of evidence, implementation, evaluation of the impact on patient care and provider performance, and consideration of the context/setting in which the practice is implemented. 15 , 17 The learning that occurs during the process of translating research into practice is valuable information to capture and feed back into the process, so that others can adapt the evidence-based guideline and/or the implementation strategies.
A recent conceptual framework for maximizing and accelerating the transfer of research results from the Agency for Healthcare Research and Quality (AHRQ) patient safety research portfolio to health care delivery was developed by the dissemination subcommittee of the AHRQ Patient Safety Research Coordinating Committee. 37 This model is a synthesis of concepts from scientific information on knowledge transfer, social marketing, social and organizational innovation, and behavior change (see Figure 1 ). 37 Although the framework is portrayed as a series of stages, the authors of this framework do not believe that the knowledge transfer process is linear; rather, activities occur simultaneously or in different sequences, with implementation of EBPs being a multifaceted process with many actors and systems.
AHRQ Model of Knowledge Transfer Adapted from Nieva, V., Murphy, R., Ridley, N., et al. Used with permission. http://www.ahrq.gov/qual/advances/
Steps of Evidence-Based Practice
Steps of promoting adoption of EBPs can be viewed from the perspective of those who conduct research or generate knowledge, 23 , 37 those who use the evidence-based information in practice, 16 , 31 and those who serve as boundary spanners to link knowledge generators with knowledge users. 19
Steps of knowledge transfer in the AHRQ model 37 represent three major stages: (1) knowledge creation and distillation, (2) diffusion and dissemination, and (3) organizational adoption and implementation. These stages of knowledge transfer are viewed through the lens of researchers/creators of new knowledge and begin with determining what findings from the patient safety portfolio or individual research projects ought to be disseminated.
Knowledge creation and distillation is conducting research (with expected variation in readiness for use in health care delivery systems) and then packaging relevant research findings into products that can be put into action—such as specific practice recommendations—thereby increasing the likelihood that research evidence will find its way into practice. 37 It is essential that the knowledge distillation process be informed and guided by end users for research findings to be implemented in care delivery. The criteria used in knowledge distillation should include perspectives of the end users (e.g., transportability to the real-world health care setting, feasibility, volume of evidence needed by health care organizations and clinicians), as well as traditional knowledge generation considerations (e.g., strength of the evidence, generalizability).
Diffusion and dissemination involves partnering with professional opinion leaders and health care organizations to disseminate knowledge that can form the basis of action (e.g., essential elements for discharge teaching for hospitalized patient with heart failure) to potential users. Dissemination partnerships link researchers with intermediaries that can function as knowledge brokers and connectors to the practitioners and health care delivery organizations. Intermediaries can be professional organizations such as the National Patient Safety Foundation or multidisciplinary knowledge transfer teams such as those that are effective in disseminating research-based cancer prevention programs. In this model, dissemination partnerships provide an authoritative seal of approval for new knowledge and help identify influential groups and communities that can create a demand for application of the evidence in practice. Both mass communication and targeted dissemination are used to reach audiences with the anticipation that early users will influence the latter adopters of the new usable, evidence-based research findings. Targeted dissemination efforts must use multifaceted dissemination strategies, with an emphasis on channels and media that are most effective for particular user segments (e.g., nurses, physicians, pharmacists).
End user adoption, implementation, and institutionalization is the final stage of the knowledge transfer process. 37 This stage focuses on getting organizations, teams, and individuals to adopt and consistently use evidence-based research findings and innovations in everyday practice. Implementing and sustaining EBPs in health care settings involves complex interrelationships among the EBP topic (e.g., reduction of medication errors), the organizational social system characteristics (such as operational structures and values, the external health care environment), and the individual clinicians. 35 , 37–39 A variety of strategies for implementation include using a change champion in the organization who can address potential implementation challenges, piloting/trying the change in a particular patient care area of the organization, and using multidisciplinary implementation teams to assist in the practical aspects of embedding innovations into ongoing organizational processes. 35 , 37 Changing practice takes considerable effort at both the individual and organizational level to apply evidence-based information and products in a particular context. 22 When improvements in care are demonstrated in the pilot studies and communicated to other relevant units in the organization, key personnel may then agree to fully adopt and sustain the change in practice. Once the EBP change is incorporated into the structure of the organization, the change is no longer considered an innovation but a standard of care. 22 , 37
In comparison, other models of EBP (e.g., Iowa Model of Evidence-based Practice to Promote Quality of Care 16 ) view the steps of the EBP process from the perspective of clinicians and/or organizational/clinical contexts of care delivery. When viewing steps of the EBP process through the lens of an end user, the process begins with selecting an area for improving care based on evidence (rather than asking what findings ought to be disseminated); determining the priority of the potential topic for the organization; formulating an EBP team composed of key stakeholders; finding, critiquing, and synthesizing the evidence; setting forth EBP recommendations, with the type and strength of evidence used to support each clearly documented; determining if the evidence findings are appropriate for use in practice; writing an EBP standard specific to the organization; piloting the change in practice; implementing changes in practice in other relevant practice areas (depending on the outcome of the pilot); evaluating the EBP changes; and transitioning ongoing quality improvement (QI) monitoring, staff education, and competency review of the EBP topic to appropriate organizational groups as defined by the organizational structure. 15 , 40 The work of EBP implementation from the perspective of the end user is greatly facilitated by efforts of AHRQ, professional nursing organizations (e.g., Oncology Nursing Society), and others that distill and package research findings into useful products and tools for use at the point of care delivery.
When the clinical questions of end users can be addressed through use of existing evidence that is packaged with end users in mind, steps of the EBP process take less time and more effort can be directed toward the implementation, evaluation, and sustainability components of the process. For example, finding, critiquing, and synthesizing the evidence; setting forth EBP recommendations with documentation of the type and strength of evidence for each recommendation; and determining appropriateness of the evidence for use in practice are accelerated when the knowledge-based information is readily available. Some distilled research findings also include quick reference guides that can be used at the point of care and/or integrated into health care information systems, which also helps with implementation. 41 , 42
Translation Science: An Overview
Translation science is the investigation of methods, interventions, and variables that influence adoption by individuals and organizations of EBPs to improve clinical and operational decisionmaking in health care. 35 , 43–46 This includes testing the effect of interventions on promoting and sustaining adoption of EBPs. Examples of translation studies include describing facilitators and barriers to knowledge uptake and use, organizational predictors of adherence to EBP guidelines, attitudes toward EBPs, and defining the structure of the scientific field. 11 , 47–49
Translation science must be guided by a conceptual model that organizes the strategies being tested, elucidates the extraneous variables (e.g., behaviors and facilitators) that may influence adoption of EBPs (e.g., organizational size, characteristics of users), and builds a scientific knowledge base for this field of inquiry. 15 , 50 Conceptual models used in the translating-research-into-practice studies funded by AHRQ were adult learning, health education, social influence, marketing, and organizational and behavior theories. 51 Investigators have used Rogers’s Diffusion of Innovation model, 35 , 39 , 52–55 the Promoting Action on Research Implementation in Health Services (PARIHS) model, 29 the push/pull framework, 23 , 56 , 57 the decisionmaking framework, 58 and the Institute for Healthcare Improvement (IHI) model 59 in translation science.
Study findings regarding evidence-based practices in a diversity of health care settings are building an empirical foundation of translation science. 19 , 43 , 51 , 60–83 These investigations and others 18 , 84–86 provide initial scientific knowledge to guide us in how to best promote use of evidence in practice. To advance knowledge about promoting and sustaining adoption of EBPs in health care, translation science needs more studies that test translating research into practice (TRIP) interventions: studies that investigate what TRIP interventions work, for whom, in what circumstances, in what types of settings; and studies that explain the underlying mechanisms of effective TRIP interventions. 35 , 49 , 79 , 87 Partnership models, which encourage ongoing interaction between researchers and practitioners, may be the way forward to carry out such studies. 56 Challenges, issues, methods, and instruments used in translation research are described elsewhere. 11 , 19 , 49 , 78 , 88–97
- Research Evidence
What Is Known About Implementing Evidence-Based Practices?
Multifaceted implementation strategies are needed to promote use of research evidence in clinical and administrative health care decisionmaking. 15 , 22 , 37 , 45 , 64 , 72 , 77 , 79 , 98 , 99 Although Grimshaw and colleagues 65 suggest that multifaceted interventions are no more effective than single interventions, context (site of care delivery) was not incorporated in the synthesis methodology. As noted by others, the same TRIP intervention may meet with varying degrees of effectiveness when applied in different contexts. 35 , 49 , 79 , 80 , 87 , 100 , 101 Implementation strategies also need to address both the individual practitioner and organizational perspective. 15 , 22 , 37 , 64 , 72 , 77 , 79 , 98 When practitioners decide individually what evidence to use in practice, considerable variability in practice patterns result, 71 potentially resulting in adverse patient outcomes.
For example, an “individual” perspective of EBP would leave the decision about use of evidence-based endotracheal suctioning techniques to each nurse and respiratory therapist. Some individuals may be familiar with the research findings for endotracheal suctioning while others may not. This is likely to result in different and conflicting practices being used as people change shifts every 8 to 12 hours. From an organizational perspective, endotracheal suctioning policies and procedures based on research are written, the evidence-based information is integrated into the clinical information systems, and adoption of these practices by nurses and other practitioners is systematically promoted in the organization. This includes assuring that practitioners have the necessary knowledge, skills, and equipment to carry out the evidence-based endotracheal suctioning practice. The organizational governance supports use of these practices through various councils and committees such as the Practice Committee, Staff Education Committee, and interdisciplinary EBP work groups.
The Translation Research Model, 35 built on Rogers’s seminal work on diffusion of innovations, 39 provides a guiding framework for testing and selecting strategies to promote adoption of EBPs. According to the Translation Research Model, adoption of innovations such as EBPs are influenced by the nature of the innovation (e.g., the type and strength of evidence, the clinical topic) and the manner in which it is communicated (disseminated) to members (nurses) of a social system (organization, nursing profession). 35 Strategies for promoting adoption of EBPs must address these four areas (nature of the EBP topic; users of the evidence; communication; social system) within a context of participative change (see Figure 2 ). This model provided the framework for a multisite study that tested the effectiveness of a multifaceted TRIP intervention designed to promote adoption of evidence-based acute pain management practices for hospitalized older adults. The intervention improved the quality of acute pain management practices and reduced costs. 81 The model is currently being used to test the effectiveness of a multifaceted TRIP intervention to promote evidence-based cancer pain management of older adults in home hospice settings. * This guiding framework is used herein to overview what is known about implementation interventions to promote use of EBPs in health care systems (see Evidence Table ).
*Implementation Model Redrawn from Rogers EM. Diffusion of innovations. 5th ed. New York: The Free Press; 2003; Titler MG, Everett LQ. Translating research into practice: considerations for critical care investigators. Crit Care Nurs Clin North Am 2001a;13(4):587-604. (more...)
Evidence Table
Evidence-Based Practice in Nursing
Nature of the Innovation or Evidence-Based Practice
Characteristics of an innovation or EBP topic that affect adoption include the relative advantage of the EBP (e.g., effectiveness, relevance to the task, social prestige); the compatibility with values, norms, work, and perceived needs of users; and complexity of the EBP topic. 39 For example, EBP topics that are perceived by users as relatively simple (e.g., influenza vaccines for older adults) are more easily adopted in less time than those that are more complex (acute pain management for hospitalized older adults). Strategies to promote adoption of EBPs related to characteristics of the topic include practitioner review and “reinvention” of the EBP guideline to fit the local context, use of quick reference guides and decision aids, and use of clinical reminders. 53 , 59 , 60 , 65 , 74 , 82 , 102–107 An important principle to remember when planning implementation of an EBP is that the attributes of the EBP topic as perceived by users and stakeholders (e.g., ease of use, valued part of practice) are neither stable features nor sure determinants of their adoption. Rather it is the interaction among the characteristics of the EBP topic, the intended users, and a particular context of practice that determines the rate and extent of adoption. 22 , 35 , 39
Studies suggest that clinical systems, computerized decision support, and prompts that support practice (e.g., decisionmaking algorithms, paper reminders) have a positive effect on aligning practices with the evidence base. 15 , 51 , 65 , 74 , 80 , 82 , 102 , 104 , 107–110 Computerized knowledge management has consistently demonstrated significant improvements in provider performance and patient outcomes. 82 Feldman and colleagues, using a just-in-time e-mail reminder in home health care, have demonstrated (1) improvements in evidence-based care and outcomes for patients with heart failure, 64 , 77 and (2) reduced pain intensity for cancer patients. 75 Clinical information systems should deploy the evidence base to the point of care and incorporate computer decision-support software that integrates evidence for use in clinical decisionmaking about individual patients. 40 , 104 , 111–114 There is still much to learn about the “best” manner of deploying evidence-based information through electronic clinical information systems to support evidence-based care. 115
Methods of Communication
Interpersonal communication channels, methods of communication, and influence among social networks of users affect adoption of EBPs. 39 Use of mass media, opinion leaders, change champions, and consultation by experts along with education are among strategies tested to promote use of EBPs. Education is necessary but not sufficient to change practice, and didactic continuing education alone does little to change practice behavior. 61 , 116 There is little evidence that interprofessional education as compared to discipline-specific education improves EBP. 117 Interactive education, used in combination with other practice-reinforcing strategies, has more positive effects on improving EBP than didactic education alone. 66 , 68 , 71 , 74 , 118 , 119 There is evidence that mass media messages (e.g., television, radio, newspapers, leaflets, posters and pamphlets), targeted at the health care consumer population, have some effect on use of health services for the targeted behavior (e.g., colorectal cancer screening). However, little empirical evidence is available to guide framing of messages communicated through planned mass media campaigns to achieve the intended change. 120
Several studies have demonstrated that opinion leaders are effective in changing behaviors of health care practitioners, 22 , 68 , 79 , 100 , 116 , 121–123 especially in combination with educational outreach or performance feedback. Opinion leaders are from the local peer group, viewed as a respected source of influence, considered by associates as technically competent, and trusted to judge the fit between the innovation and the local situation. 39 , 116 , 121 , 124–127 With their wide sphere of influence across several microsystems/units, opinion leaders’ use of the innovation influences peers and alters group norms. 39 , 128 The key characteristic of an opinion leader is that he or she is trusted to evaluate new information in the context of group norms. Opinion leadership is multifaceted and complex, with role functions varying by the circumstances, but few successful projects to implement innovations in organizations have managed without the input of identifiable opinion leaders. 22 , 35 , 39 , 81 , 96 Social interactions such as “hallway chats,” one-on-one discussions, and addressing questions are important, yet often overlooked components of translation. 39 , 59 Thus, having local opinion leaders discuss the EBPs with members of their peer group is necessary to translate research into practice. If the EBP that is being implemented is interdisciplinary in nature, discipline-specific opinion leaders should be used to promote the change in practice. 39
Change champions are also helpful for implementing innovations. 39 , 49 , 81 , 129–131 They are practitioners within the local group setting (e.g., clinic, patient care unit) who are expert clinicians, passionate about the innovation, committed to improving quality of care, and have a positive working relationship with other health care professionals. 39 , 125 , 131 , 132 They circulate information, encourage peers to adopt the innovation, arrange demonstrations, and orient staff to the innovation. 49 , 130 The change champion believes in an idea; will not take “no” for an answer; is undaunted by insults and rebuffs; and, above all, persists. 133 Because nurses prefer interpersonal contact and communication with colleagues rather than Internet or traditional sources of practice knowledge, 134–137 it is imperative that one or two change champions be identified for each patient care unit or clinic where the change is being made for EBPs to be enacted by direct care providers. 81 , 138 Conferencing with opinion leaders and change champions periodically during implementation is helpful to address questions and provide guidance as needed. 35 , 66 , 81 , 106
Because nurses’ preferred information source is through peers and social interactions, 134–137 , 139 , 140 using a core group in conjunction with change champions is also helpful for implementing the practice change. 16 , 110 , 141 A core group is a select group of practitioners with the mutual goal of disseminating information regarding a practice change and facilitating the change by other staff in their unit/microsystem. 142 Core group members represent various shifts and days of the week and become knowledgeable about the scientific basis for the practice; the change champion educates and assists them in using practices that are aligned with the evidence. Each member of the core group, in turn, takes the responsibility for imparting evidence-based information and effecting practice change with two or three of their peers. Members assist the change champion and opinion leader with disseminating the EBP information to other staff, reinforce the practice change on a daily basis, and provide positive feedback to those who align their practice with the evidence base. 15 Using a core-group approach in conjunction with a change champion results in a critical mass of practitioners promoting adoption of the EBP. 39
Educational outreach, also known as academic detailing, promotes positive changes in practice behaviors of nurses and physicians. 22 , 64 , 66 , 71 , 74 , 75 , 77 , 81 , 119 , 143 Academic detailing is done by a topic expert, knowledgeable of the research base (e.g., cancer pain management), who may be external to the practice setting; he or she meets one-on-one with practitioners in their setting to provide information about the EBP topic. These individuals are able to explain the research base for the EBPs to others and are able to respond convincingly to challenges and debates. 22 This strategy may include providing feedback on provider or team performance with respect to selected EBP indicators (e.g., frequency of pain assessment). 66 , 81 , 119
Users of the Innovation or Evidence-Based Practice
Members of a social system (e.g., nurses, physicians, clerical staff) influence how quickly and widely EBPs are adopted. 39 Audit and feedback, performance gap assessment (PGA), and trying the EBP are strategies that have been tested. 15 , 22 , 65 , 66 , 70–72 , 81 , 98 , 124 , 144 PGA and audit and feedback have consistently shown a positive effect on changing practice behavior of providers. 65 , 66 , 70 , 72 , 81 , 98 , 124 , 144 , 145 PGA (baseline practice performance) informs members, at the beginning of change, about a practice performance and opportunities for improvement. Specific practice indicators selected for PGA are related to the practices that are the focus of evidence-based practice change, such as every-4-hour pain assessment for acute pain management. 15 , 66 , 81
Auditing and feedback are ongoing processes of using and assessing performance indicators (e.g., every-4-hour pain assessment), aggregating data into reports, and discussing the findings with practitioners during the practice change. 22 , 49 , 66 , 70 , 72 , 81 , 98 , 145 This strategy helps staff know and see how their efforts to improve care and patient outcomes are progressing throughout the implementation process. Although there is no clear empirical evidence for how to provide audit and feedback, 70 , 146 effects may be larger when clinicians are active participants in implementing change and discuss the data rather than being passive recipients of feedback reports. 67 , 70 Qualitative studies provide some insight into use of audit and feedback. 60 , 67 One study on use of data feedback for improving treatment of acute myocardial infarction found that (1) feedback data must be perceived by physicians as important and valid, (2) the data source and timeliness of data feedback are critical to perceived validity, (3) time is required to establish credibility of data within a hospital, (4) benchmarking improves the validity of the data feedback, and (5) physician leaders can enhance the effectiveness of data feedback. Data feedback that profiles an individual physician’s practices can be effective but may be perceived as punitive; data feedback must persist to sustain improved performance; and effectiveness of data feedback is intertwined with the organizational context, including physician leadership and organizational culture. 60 Hysong and colleagues 67 found that high-performing institutions provided timely, individualized, nonpunitive feedback to providers, whereas low performers were more variable in their timeliness and nonpunitiveness and relied more on standardized, facility-level reports. The concept of useful feedback emerged as the core concept around which timeliness, individualization, nonpunitiveness, and customizability are important.
Users of an innovation usually try it for a period of time before adopting it in their practice. 22 , 39 , 147 When “trying an EBP” (piloting the change) is incorporated as part of the implementation process, users have an opportunity to use it for a period of time, provide feedback to those in charge of implementation, and modify the practice if necessary. 148 Piloting the EBP as part of implementation has a positive influence on the extent of adoption of the new practice. 22 , 39 , 148
Characteristics of users such as educational preparation, practice specialty, and views on innovativeness may influence adoption of an EBP, although findings are equivocal. 27 , 39 , 130 , 149–153 Nurses’ disposition to critical thinking is, however, positively correlated with research use, 154 and those in clinical educator roles are more likely to use research than staff nurses or nurse managers. 155
Social System
Clearly, the social system or context of care delivery matters when implementing EBPs. 2 , 30 , 33 , 39 , 60 , 84 , 85 , 91 , 92 , 101 , 156–163 For example, investigators demonstrated the effectiveness of a prompted voiding intervention for urinary incontinence in nursing homes, but sustaining the intervention in day-to-day practice was limited when the responsibility of carrying out the intervention was shifted to nursing home staff (rather than the investigative team) and required staffing levels in excess of a majority of nursing home settings. 164 This illustrates the importance of embedding interventions into ongoing processes of care.
Several organizational factors affect adoption of EBPs. 22 , 39 , 79 , 134 , 165–167 Vaughn and colleagues 101 demonstrated that organizational resources, physician full-time employees (FTEs) per 1,000 patient visits, organizational size, and whether the facility was located in or near a city affected use of evidence in the health care system of the Department of Veterans Affairs (VA). Large, mature, functionally differentiated organizations (e.g., divided into semiautonomous departments and units) that are specialized, with a focus of professional knowledge, slack resources to channel into new projects, decentralized decisionmaking, and low levels of formalization will more readily adopt innovations such as new practices based on evidence. Larger organizations are generally more innovative because size increases the likelihood that other predictors of innovation adoption—such as slack financial and human resources and differentiation—will be present. However, these organizational determinants account for only about 15 percent of the variation in innovation adoption between comparable organizations. 22 Adler and colleagues 168 hypothesize that while more structurally complex organizations may be more innovative and hence adopt EBPs relatively early, less structurally complex organizations may be able to diffuse EBPs more effectively. Establishing semiautonomous teams is associated with successful implementation of EBPs, and thus should be considered in managing organizational units. 168–170
As part of the work of implementing EBPs, it is important that the social system—unit, service line, or clinic—ensures that policies, procedures, standards, clinical pathways, and documentation systems support the use of the EBPs. 49 , 68 , 72 , 73 , 103 , 140 , 171 Documentation forms or clinical information systems may need revision to support changes in practice; documentation systems that fail to readily support the new practice thwart change. 82
Absorptive capacity for new knowledge is another social system factor that affects adoption of EBPs. Absorptive capacity is the knowledge and skills to enact the EBPs; the strength of evidence alone will not promote adoption. An organization that is able to systematically identify, capture, interpret, share, reframe, and recodify new knowledge, and put it to appropriate use, will be better able to assimilate EBPs. 82 , 103 , 172 , 173 A learning organizational culture and proactive leadership that promotes knowledge sharing are important components of building absorptive capacity for new knowledge. 66 , 139 , 142 , 174 Components of a receptive context for EBP include strong leadership, clear strategic vision, good managerial relations, visionary staff in key positions, a climate conducive to experimentation and risk taking, and effective data capture systems. Leadership is critical in encouraging organizational members to break out of the convergent thinking and routines that are the norm in large, well-established organizations. 4 , 22 , 39 , 122 , 148 , 163 , 175
An organization may be generally amenable to innovations but not ready or willing to assimilate a particular EBP. Elements of system readiness include tension for change, EBP-system fit, assessment of implications, support and advocacy for the EBP, dedicated time and resources, and capacity to evaluate the impact of the EBP during and following implementation. If there is tension around specific work or clinical issues and staff perceive that the situation is intolerable, a potential EBP is likely to be assimilated if it can successfully address the issues, and thereby reduce the tension. 22 , 175
Assessing and structuring workflow to fit with a potential EBP is an important component of fostering adoption. If implications of the EBP are fully assessed, anticipated, and planned for, the practice is more likely to be adopted. 148 , 162 , 176 If supporters for a specific EBP outnumber and are more strategically placed within the organizational power base than opponents, the EBP is more likely to be adopted by the organization. 60 , 175 Organizations that have the capacity to evaluate the impact of the EBP change are more likely to assimilate it. Effective implementation needs both a receptive climate and a good fit between the EBP and intended adopters’ needs and values. 22 , 60 , 140 , 175 , 177
Leadership support is critical for promoting use of EBPs. 33 , 59 , 72 , 85 , 98 , 122 , 178–181 This support, which is expressed verbally, provides necessary resources, materials, and time to fulfill assigned responsibilities. 148 , 171 , 182 , 183 Senior leaders need to create an organizational mission, vision, and strategic plan that incorporate EBP; implement performance expectations for staff that include EBP work; integrate the work of EBP into the governance structure of the health care system; demonstrate the value of EBPs through administrative behaviors; and establish explicit expectations that nurse leaders will create microsystems that value and support clinical inquiry. 122 , 183 , 184
A recent review of organizational interventions to implement EBPs for improving patient care examined five major aspects of patient care. The review suggests that revision of professional roles (changing responsibilities and work of health professionals such as expanding roles of nurses and pharmacists) improved processes of care, but it was less clear about the effect on improvement of patient outcomes. Multidisciplinary teams (collaborative practice teams of physicians, nurses, and allied health professionals) treating mostly patients with prevalent chronic diseases resulted in improved patient outcomes. Integrated care services (e.g., disease management and case management) resulted in improved patient outcomes and cost savings. Interventions aimed at knowledge management (principally via use of technology to support patient care) resulted in improved adherence to EBPs and patient outcomes. The last aspect, quality management, had the fewest reviews available, with the results uncertain. A number of organizational interventions were not included in this review (e.g., leadership, process redesign, organizational learning), and the authors note that the lack of a widely accepted taxonomy of organizational interventions is a problem in examining effectiveness across studies. 82
An organizational intervention that is receiving increasing attention is tailored interventions to overcome barriers to change. 162 , 175 , 185 This type of intervention focuses on first assessing needs in terms of what is causing the gap between current practice and EBP for a specified topic, what behaviors and/or mechanism need to change, what organizational units and persons should be involved, and identification of ways to facilitate the changes. This information is then used in tailoring an intervention for the setting that will promote use of the specified EBP. Based on a recent systematic review, effectiveness of tailored implementation interventions remains uncertain. 185
In summary, making an evidence-based change in practice involves a series of action steps and a complex, nonlinear process. Implementing the change will take several weeks to months, depending on the nature of the practice change. Increasing staff knowledge about a specific EBP and passive dissemination strategies are not likely to work, particularly in complex health care settings. Strategies that seem to have a positive effect on promoting use of EBPs include audit and feedback, use of clinical reminders and practice prompts, opinion leaders, change champions, interactive education, mass media, educational outreach/academic detailing, and characteristics of the context of care delivery (e.g., leadership, learning, questioning). It is important that senior leadership and those leading EBP improvements are aware of change as a process and continue to encourage and teach peers about the change in practice. The new practice must be continually reinforced and sustained or the practice change will be intermittent and soon fade, allowing more traditional methods of care to return. 15
- Practice Implications From Translation Science
Principles of Evidence-Based Practice for Patient Safety
Several translation science principles are informative for implementing patient safety initiatives:
- First, consider the context and engage health care personnel who are at the point of care in selecting and prioritizing patient safety initiatives, clearly communicating the evidence base (strength and type) for the patient safety practice topic(s) and the conditions or setting to which it applies. These communication messages need to be carefully designed and targeted to each stakeholder user group.
- Second, illustrate, through qualitative or quantitative data (e.g., near misses, sentinel events, adverse events, injuries from adverse events), the reason the organization and individuals within the organization should commit to an evidence-based safety practice topic. Clinicians tend to be more engaged in adopting patient safety initiatives when they understand the evidence base of the practice, in contrast to administrators saying, “We must do this because it is an external regulatory requirement.” For example, it is critical to converse with busy clinicians about the evidence-based rationale for doing fall-risk assessment, and to help them understand that fall-risk assessment is an external regulatory agency expectation because the strength of the evidence supports this patient safety practice.
- Third, didactic education alone is never enough to change practice; one-time education on a specific safety initiative is not enough. Simply improving knowledge does not necessarily improve practice. Rather, organizations must invest in the tools and skills needed to create a culture of evidence-based patient safety practices where questions are encouraged and systems are created to make it easy to do the right thing.
- Fourth, the context of EBP improvements in patient safety need to be addressed at each step of the implementation process; piloting the change in practice is essential to determine the fit between the EBP patient safety information/innovation and the setting of care delivery. There is no one way to implement, and what works in one agency may need modification to fit the organizational culture of another context.
- Finally, it is important to evaluate the processes and outcomes of implementation. Users and stakeholders need to know that the efforts to improve patient safety have a positive impact on quality of care. For example, if a new barcoding system is being used to administer blood products, it is imperative to know that the steps in the process are being followed (process indicators) and that the change in practice is resulting in fewer blood product transfusion errors (outcome indicators).
Research Implications
Translation science is young, and although there is a growing body of knowledge in this area, we have, to date, many unanswered questions. These include the type of audit and feedback (e.g., frequency, content, format) strategies that are most effective, the characteristics of opinion leaders that are critical for success, the role of specific context variables, and the combination of strategies that are most effective. We also know very little about use of tailored implementation interventions, or the key context attributes to assess and use in developing and testing tailored interventions. The types of clinical reminders that are most effective for making EBP knowledge available at the point of care require further empirical explanation. We also know very little about the intensity and intervention dose of single and multifaceted strategies that are effective for promoting and sustaining use of EBPs or how the effectiveness differs by type of topic (e.g., simple versus complex). Only recently has the context of care delivery been acknowledged as affecting use of evidence, and further empirical work is needed in this area to understand how complex adaptive systems of practice incorporate knowledge acquisition and use. Lastly, we do not know what strategies or combination of strategies work for whom, in what context, why they work in some settings or cases and not others, and what is the mechanism by which these strategies or combination of strategies work.
This is an exciting area of investigation that has a direct impact on implementing patient safety practices. In planning investigations, researchers must use a conceptual model to guide the research and add to the empirical and theoretical understanding of this field of inquiry. Additionally, funding is needed for implementation studies that focus on evidence-based patient safety practices as the topic of concern. To generalize empirical findings from patient safety implementation studies, we must have a better understanding of what implementation strategies work, with whom, and in what types of settings, and we must investigate the underlying mechanisms of these strategies. This is likely to require mixed methods, a better understanding of complexity science, and greater appreciation for nontraditional methods and realistic inquiry. 87
Although the science of translating research into practice is fairly new, there is some guiding evidence of what implementation interventions to use in promoting patient safety practices. However, there is no magic bullet for translating what is known from research into practice. To move evidence-based interventions into practice, several strategies may be needed. Additionally, what works in one context of care may or may not work in another setting, thereby suggesting that context variables matter in implementation. 80
- Search Strategy
Several electronic databases were searched (MEDLINE ® , CINAHL ® , PubMed ® ) using terms of evidence-based practice research, implementation research, and patient safety. (The terms “quality improvement” or “quality improvement intervention research” were not used.) The Cochrane Collaboration–Cochrane Reviews was also searched to look for systematic reviews of specific implementation strategies, and the Journal of Implementation Science was also reviewed. I also requested the final reports of the TRIP I and TRIP II studies funded by AHRQ. Classic articles known to the author were also included in this chapter (e.g.,Locock et al. 123 ).
*Principal Investigator: Keela Herr (R01 grant no. CA115363-01; National Cancer Institute (NCI))Background
- Cite this Page Titler MG. The Evidence for Evidence-Based Practice Implementation. In: Hughes RG, editor. Patient Safety and Quality: An Evidence-Based Handbook for Nurses. Rockville (MD): Agency for Healthcare Research and Quality (US); 2008 Apr. Chapter 7.
- PDF version of this page (470K)
In this Page
Other titles in this collection.
- Advances in Patient Safety
Related information
- PMC PubMed Central citations
- PubMed Links to PubMed
Similar articles in PubMed
- It Is Not That Simple nor Compelling! Comment on "Translating Evidence Into Healthcare Policy and Practice: Single Versus Multi-faceted Implementation Strategies - Is There a Simple Answer to a Complex Question?". [Int J Health Policy Manag. 2015] It Is Not That Simple nor Compelling! Comment on "Translating Evidence Into Healthcare Policy and Practice: Single Versus Multi-faceted Implementation Strategies - Is There a Simple Answer to a Complex Question?". Bucknall T, Fossum M. Int J Health Policy Manag. 2015 Jul 28; 4(11):787-8. Epub 2015 Jul 28.
- Nursing implementation science: how evidence-based nursing requires evidence-based implementation. [J Nurs Scholarsh. 2008] Nursing implementation science: how evidence-based nursing requires evidence-based implementation. van Achterberg T, Schoonhoven L, Grol R. J Nurs Scholarsh. 2008; 40(4):302-10.
- Review The science of implementation: changing the practice of critical care. [Curr Opin Crit Care. 2008] Review The science of implementation: changing the practice of critical care. Weinert CR, Mann HJ. Curr Opin Crit Care. 2008 Aug; 14(4):460-5.
- Review Integrative review of implementation strategies for translation of research-based evidence by nurses. [Clin Nurse Spec. 2014] Review Integrative review of implementation strategies for translation of research-based evidence by nurses. Wuchner SS. Clin Nurse Spec. 2014 Jul-Aug; 28(4):214-23.
- Review A realist analysis of hospital patient safety in Wales: applied learning for alternative contexts from a multisite case study [ 2015] Review A realist analysis of hospital patient safety in Wales: applied learning for alternative contexts from a multisite case study Herepath A, Kitchener M, Waring J. 2015 Sep
Recent Activity
- The Evidence for Evidence-Based Practice Implementation - Patient Safety and Qua... The Evidence for Evidence-Based Practice Implementation - Patient Safety and Quality
Your browsing activity is empty.
Activity recording is turned off.
Turn recording back on
Connect with NLM
National Library of Medicine 8600 Rockville Pike Bethesda, MD 20894
Web Policies FOIA HHS Vulnerability Disclosure
Help Accessibility Careers
- Open access
- Published: 15 September 2024
Exploring academic and clinical nurses’ perspectives on evidence-based nursing course for undergraduates from perspectives of academic-practice partnerships: a qualitative study
- Guiyun Wang 1 ,
- Yuting Xia 2 ,
- Qirong Chen 2 ,
- Xirongguli Halili 2 &
- Hui Huang 3
BMC Nursing volume 23 , Article number: 657 ( 2024 ) Cite this article
Metrics details
To explore nurses’ perceptions of evidence-based nursing courses for undergraduates through academic-practice partnerships.
A deductive thematic analysis based on the practice-academic logic model.
Fifteen academic and clinical nurses were interviewed between November and December 2023, either online or through face-to-face meetings. Each interview lasted 20–30 min. The interview outline was constructed based on the practice-academic partnership logic model, which was followed during the process of recorded, analyzed, and checked.
Themes identified include inputs (e.g., stakeholder commitment), activities (e.g., communication), outputs (e.g., nursing projects), and outcomes (e.g., improved competence). These themes highlight the various aspects and outcomes of academic-practice partnerships in evidence-based nursing courses.
Effective academic-practice partnerships are crucial for developing evidence-based nursing courses, leading to positive educational and professional outcomes.
Nurses’ perceptions provide valuable guidelines for developing effective evidence-based nursing courses.
Patient or public contribution
No patient or public users participated in this study.
Peer Review reports
Introduction
Evidence-based nursing (EBN) is a systematic approach to addressing clinical questions that combines research findings, clinicians’ expertise, and patients’ values [ 1 ]. Conducting evidence-based nursing practices (EBNP) has a significant effect on improving the quality of nursing care and reducing healthcare expenses [ 2 , 3 , 4 ]. Over the past decade, researchers have emphasized the importance of EBNP [ 5 ]. However, limited EBNP projects has been conducted in clinical nursing [ 6 ]. The main reason for the insufficient implementation of EBNP is the lack of EBN knowledge, competence, resources, and adherence to complete processes and pathways by nurses [ 7 ]. Conducting high-quality EBN education is a key measure to improve the EBN competence of nurses [ 8 ]. Undergraduate nursing students are the future of the nursing workforce [ 9 , 10 ]. Undergraduate nursing students will have the competence to conduct EBNP projects to promote the development of nursing care towards a more professional and scientific direction [ 11 ]. American Medical Association has pointed out that conducting EBP education for undergraduate nursing students is the key to equipping them with EBN competence and enabling them to conduct EBNP [ 12 ].
Nevertheless, there is limited studies focused on developing of EBN education for undergraduate nursing students [ 11 ]. Existing studies have shown that EBN education for undergraduate nursing students mainly focuses on lectures, interactive, and blended online and offline teaching and the EBNP education for undergraduate nursing students were conducted by clinical nurses [ 12 , 13 , 14 ]. However, most of the clinical nurses lacked of time to provide systematic EBN theory education for undergraduate, which caused the undergraduate nursing student with low level of EBN knowledge and ability [ 13 , 14 , 15 , 16 , 17 ]. The separation of theory and practice is the main drawback of existing EBN education for undergraduate nursing students [ 13 , 14 ]. However, theory and practice are two essential and complementary components of EBN [ 18 ].
Academic-practice partnerships (APPs) refers to the establishment of strategic relationships between academic and clinical institutions, fully utilizing the advantages of both sides, and promoting common vision in teaching, practice, and research [ 19 ]. Conducting APPs in EBN (APPs-EBN) education will overcome the key obstacle of the existing EBN education for undergraduate nursing students [ 12 , 20 ]. To understand the content of APPs-EBN education, the steps of existing research of APPs-EBN training program for nursing students was shown as following [ 21 , 22 ]: (1) clinical nurses to identify their needs; (2) academic nurses assigned nursing students specific topics, provide reading materials and videos; (3) nursing students formulated EBNP questions (PICOs, including participants, interventions, comparison, outcomes, and study design [ 23 ]. PICOs were the important content of EBNP questions [ 23 ].); (4) academic nurses, clinical nurses and nursing students discussed the accuracy of EBNP questions (PICOs); (5) nursing students submitted their homework and received their grades with feedback; (6) academic and clinical nurses chose a final EBNP question (PICOs) that was befitting for each student group.
Academic nurses and clinical nurses should be the core of APPs-EBN education for undergraduate nursing students, actively participating in all stages of EBN education process [ 22 ]. Moreover, conducting APPs-EBN education must be achieved through individual-level partnerships of academic nurses and clinical nurses [ 20 , 24 ]. However, existing studies focused on discussing APPs-EBN practice at institutional level, with limited studies focused on the individual perspectives of APPs-EBN education, especially for the undergraduate nursing student’s EBN education [ 19 , 20 , 25 ]. Therefore, it is crucial to understand the perceptions of academic and clinical nurses on APPs-EBN course for undergraduate nursing students to provide information for improving the quality of APPs-EBN course for undergraduate nursing students. However, there is a lack of individual-level evidence on specific perceptions of APPs-EBN course for undergraduate nursing students.
Practice-academic partnership logic model was designed for APPs program. Given the efficacy of this model has been approved in the aspect of APPs and its appropriateness for this qualitative study to deductive specific and essential content during the process of APPs, further to provide basis for researchers conduct APPs-EBN course for undergraduate nursing students [ 22 ]. This model emphasizes that having specific inputs and conducting specific activities in the process of APPs may result in corresponding outputs and outcomes (inputs and activities → outputs and outcomes). Inputs encompass the necessary investments in the APPs-EBN education program, including partnership champions, compatible philosophies, common vision, key stakeholder commitment, formalized partnership agreement, shared goals and accountabilities and dedicated time and resources [ 22 , 26 ]. Activities involve specific actions or processes that must be undertaken to yield desired outcomes from the APPs, including open, ongoing communications, shared decision-making and professional development [ 22 , 26 ]. Outputs are the tangible and immediate deliverables stemming from the inputs and activities, including action plans and strategic plans [ 22 , 26 ]. Outcomes, both short-term and long-term, denote the changes or impacts that arise from the APPs, including successful completion of short-term (action plan) goals and successful completion of long-term (strategic) goals [ 22 , 26 ]. Therefore, this study aimed to explore and interpret the perceptions on APPs-EBN course for undergraduate nursing students among the academic nurses and clinical nurses based on the partnership-academic partnership logic model. This study will provide a valuable information for further constructing APPs-EBN course for undergraduate nursing students.
This qualitative study used deductive thematic analysis by using the practice-academic logic model [ 27 ]. The qualitative study was reported following the Consolidated Criteria for Reporting Qualitative Research checklist [ 28 ].
Participants
Considering that academic and clinical nurses were the main stakeholders in APPs-EBN course for undergraduate nursing students, this study conducted qualitative interviews with these two groups of people. Inclusion criteria for academic nurses was that academic nurses had experience in teaching EBN course for undergraduate and/or graduate nursing students. Inclusion criteria for clinical nurses were as follows: (1) clinical nurses were responsible for providing direct care to patients in a hospital unit. (2) clinical nurses have the experience in EBNP.
Data collection
The data were collected between November and December 2023. The interviews were conducted through online videoconferencing meetings or face-to-face meetings in participants’ offices. Each participant underwent a single interview session, with each interview lasting approximately 20–30 min. The interviews were conducted by the corresponding author (Y.X.) who was a female master’s nursing student and has completed qualitative research training.
The sampling method employed was purposive sampling, which can consciously select some participants who understand the research questions and provide rich information in the interviews [ 29 ]. The interview outline was constructed based on the practice-academic partnership logic model, which mainly includes what support did we need from both the organizational and individual levels to conduct APPs-EBN course for undergraduate nursing students? What activities could be conducted in APPs-EBN course to improve teaching effectiveness? What were the outputs of conducting APPs-EBN course for undergraduate nursing students? What were the outcomes for conducting APPs-EBN course for undergraduate nursing students?
Before conducting the formal interview, the researchers contacted the interviewees through WeChat (the social media most commonly used in China) to introduce the purpose, significance, and methods of this part of the research. After obtaining consent from the participants, the interview schedule was arranged to accommodate their availability. Before commencing the formal interviews, the researchers reiterated the research’s purpose, significance, and methodologies to the interviewees, while also ensuring the protection of their privacy. Detailed explanations were provided concerning the recording procedures, and the interviewees were requested to sign an informed consent form before the interviews officially commenced, including the recording process. The semi-structured interview outline served as a comprehensive guide throughout the interview process, ensuring that the interview content remained closely aligned with the research objectives. All the interviews were recorded. Any questions that arose during the interview were promptly addressed to maintain clarity and depth of the responses.
Data analysis
Within 24 h after the interview, two researchers (Y.X. and H.H) converted 15 interview recordings into written materials and listened to the recordings multiple times to ensure the accuracy of the transcription results. The interview transcriptions were analyzed in NVivo 12.0. The corresponding author (Y.X.) followed the following steps to code the perspectives of participants: immersing in the data, developing an initial thematic template, organizing the data based on the template, condensing data and reflecting, comparing and contrasting data within similar participant categories, and comparing and contrasting data with different participant categories [ 20 ]. After completing the initial encoding of all data, the corresponding author (Y.X.) shared and validated the encoding results with other members of the research team to form the final encoding result [ 30 ].
Ethic considerations
This study was approved by the Ethics Committee of a nursing school in Hunan Province in March 2023 (review number: E202313). All the recorded data are only used for this study and were backed up in an encrypted computer without Internet connection.
Nine academic nurses participated in this study, two males and seven females, with an average age of (38.00 ± 8.00) years. Among them, eight academic nurses have a doctoral degree, and one academic nurse has a master’s degree. The nine academic nurses were from five different school of nursing in China and both of them have the experience in participating the APP-EBN courses for nurses or graduate nursing students. Six clinical nurses participated in this study, all of them were females and have a master’s degree, with an average age of (37.17 ± 4.26) years. And six clinical nurses were from four different comprehensive hospital in China and three clinical nurses have the experience in participating the APP-EBN projects.
Four themes with 16 subthemes were generated based on practice-academic partnership logic model (Table 1 ), including inputs, activities, outputs, outcomes.
All participants considered the multilevel contents of inputs were the necessary investment of APPs-EBN course for undergraduate nursing students.
Key stakeholder commitment
A few participants noted that academic and clinical institutions needed to form formal partnership before developed APPs-EBN course for undergraduate nursing students, which was beneficial for promoting APPs-EBN course. As the opinion by one participant, “The first step of developing APPs-EBN course is to reach a consensus and sign a partnership agreement between academic and clinical leadership , and vigorously promote developing APPs-EBN course.” (Participant 14 , Clinical nurse) Developing a teaching team was one of the important aspects of achieving key stakeholder commitment of APPs. “How to attract clinical nurses to participate in the teaching team requires the academic and clinical institutions to sign some partnership agreements.” (Participant 2 , Academic nurse).
Key stakeholder commitment was an important input for developing APPs-EBN course for undergraduate nursing students and further promoting common interests in EBN education, practice, and research [ 31 ].
Shared mission
Some participants believed that shared mission was an important input for developing of APPs-EBN course for undergraduate nursing students. As a participant mentioned, “It is necessary to consider shared mission. For example , if the goal is to implement EBNP projects in clinical settings after the course , plans must be made to enhance these projects while developing the course.” (Participant 2 , Academic nurse) Academic and clinical institution had shared mission was conducive to making the partnerships process smoother [ 26 ]. For example, “The leadership is very important during the process of APPs. Leaderships of the academic and the nursing department of the clinical focus on a shared mission to develop this course , which may have a significant impact (on the development of APPs-EBN course for undergraduate nursing students).” (Participant 3 , Academic nurse) .
EBN training
Participants mentioned that EBN training was necessary for academic and clinical nurses to improve their EBN competence and acquire the newest knowledge about EBN.
“From organizational level , it is necessary to regularly provide EBNP training opportunities for clinical nurses or provide more updates and lectures on this EBN to academic nurses.” (Participant 3 , Academic nurse) . “If there is such specialized EBN training , it would be best for academic and clinical nurses to participate in systematic learning.” (Participant 5 , Academic nurse) . “Regular training for academic and clinical nurses is necessary. Academic nurses primarily participate in training programs related to EBNP and teaching ability , while clinical nurses primarily participate in training programs related to teaching ability.” (Participant 8 , Academic nurse) .
Developing and conducting APPs-EBN course for undergraduate nursing students required academic and clinical nurses to input a significant amount of time in communication and preparing for teaching APPs-EBN course.
“For some (academic and clinical) nurses , time may be the biggest problem , as building the APPs-EBN course requires partnerships between academic and clinical nurses , including spending time on partnership and individual lesson preparation.” (Participant 10 , Clinical nurse) . “It is difficult for clinical nurses to participant in teaching APPs-EBN course for undergraduate student during their own rest.” (Participant 7 , Academic nurse) . “Developing the APPs-EBN course demands a substantial investment of time from both academic and clinical nurses. From a clinical perspective , the success of this endeavor largely hinges on the level of support from nursing leaders. If nursing leaders truly value this course , they will ensure that clinical nurses have sufficient time to contribute to its teaching.” (Participant 14 , Clinical nurse) .
Instructional design
According to the characteristics of the target population (undergraduate nursing students), the development of APPs-EBN course instructional design (including learning objectives, learning contents, learning methods, and learning resources) was the cornerstone of developing and implementing EBN education [ 32 ]. “The learning objectives is actually your initial origin of instructional design. Firstly , it is necessary to analyze what abilities undergraduate nursing students need to possess in the future clinical nursing , what kind of foundation they need nurses (academic and clinical nurses) to lay for them during their learning period , and what kind of (EBN) knowledge and skills they need to be taught.” (Participant 9 , Academic nurse) .
Comprehensive and systematic educational resources form the foundation for promoting the acquisition of EBN knowledge among undergraduate nursing students [ 33 , 34 ]. Evidence retrieval is a crucial prerequisite for evidence implementation, and ample database resources can significantly enhance the teaching of evidence retrieval in APPs-EBN courses for these students [ 35 ]. Several participants highlighted that database resources are essential for developing APPs-EBN courses for undergraduate nursing students.
“Provide them (undergraduate nursing students) with database resources to access relevant databases for retrieval.” (Participant 8 , Academic nurse) . “Sometimes , we use databases from other universities , because our university actually doesn’t have any databases about evidence-based nursing. It is necessary for university to support more database resources.” (Participant 5 , Academic nurse) .
The participants stated that universities and hospitals provide incentives for academic and clinical nurses, which could enhance the teaching engagement of these professionals.
“The clinical nurses who participated in this course (APPs-EBN course for undergraduate nursing students) have some corresponding incentives , including establishing some educational reform projects and funding.” (Participant 5 , Academic nurse) . “Perhaps there should be time support and performance rewards for nurses (academic and clinical nurses) to participate in this course (APPs-EBN course for undergraduate nursing students). Especially for clinical nurses , they should be provided more time support and performance rewards and honors for the engagement in EBNP education.” (Participant 8 , Academic nurse) . “It is necessary that both the academic and clinical institutions provide clear incentives. If you participate in APPs-EBN course for undergraduate nursing students , it will be beneficial for evaluating professional titles. In addition , it is basic to provide academic and clinical teachers more salary.” (Participant 10 , Clinical nurse) .
Mutual trust
Mutual respect was a key condition for developing of APPs-EBN course for undergraduate nursing students [ 26 ]. As participants said that, “It is important to establish a good relationship between academic and clinical nurses , as well as to have some communication during the teaching process.” (Participant 1 , Academic nurse) “Academic and clinical nurses definitely need to fully respect each other’s suggestions and skills , which is actually a very important prerequisite for partnerships.” (Participant 9 , Academic nurse) .
Leadership support
Leadership support was an important input in developing of APPs-EBN course for undergraduate nursing students. Academic and clinical nurses participating in teaching were more familiar with the characteristics of nursing undergraduate students. The leadership of academic and clinical institutions should provide these professionals with greater rights in developing of APPs-EBN course. “Because this (APPs-EBN course) is intended for students (undergraduate nursing students). It is necessary for leaderships of academic and clinical institutions to provide them (academic and clinical nurses) full freedom to design or optimize this course on their own. ” (Participant 9 , Academic nurse) .
In addition, the time for participating in the teaching of APPs-EBN course the requires the leadership-level support. Leaders should provide academic and clinical nurses with more opportunities to conduct EBNP.
“The support of leaders is essential. For example , if undergraduate nursing students come to a hospital for internships , nursing leaders need to provide them with sufficient support to conduct EBNP projects or participate in the application of clinical guidelines.” (Participant 8 , Academic nurse) . “It is necessary to have the support of the nursing teaching and research department , as this department could identity clinical nurses (with EBNP experience). In addition , the support of nursing leaders is also very important , they could arrange the scheduling and teaching tasks for clinical nurses.” (Participant 15 , Clinical nurse) .
Participants considered activities were essential part during the process of developing of APPs-EBN course for undergraduate nursing student. The effective activities included ongoing communication and share decision-making.
Ongoing communication
Ongoing communications between academic and clinical teachers were beneficial for them to jointly develop and optimize the course, and clarified the teaching tasks of both sides.
“Academic and clinical nurses need to engage in lesson preparation collaboratively. While academic nurses may primarily teach theoretical courses , clinical nurses should work with them to monitor the course’s progress and integrate clinical questions into practical sessions. Both groups should discuss and coordinate to define the teaching tasks effectively.” (Participant 1 , Academic nurse) . “Academic and clinical nurses may need to discuss with both sides about how to better integrate the theory knowledge into the practical course. Firstly , partnership lesson preparation is a part of the teaching process in which both sides are aware of each other’s teaching tasks…… Some partnership discussions and feedback are also important.” (Participant 9 , Academic nurse) .
Share decision-making
Academic and clinical nurses shared decision-making to each other during the teaching process of APPs-EBN course for undergraduate nursing students, which was beneficial to APPs-EBN course for undergraduate nursing students [ 26 ]. For example, “Clinical nurses need to provide timely feedback to academic nurses on any suggestions they may have during the implementation of the course. Academic nurses should also observe if there are some problems that effect teaching quality that require optimization. In other words , adjustments need to be made through regular discussions and feedback between both sides , in order to optimize the course in a timely manner” (Participant 9 , Academic nurse) .
Participants described that APPs-EBN course for undergraduate nursing students may could form outputs.
EBNP projects
More EBNP projects could be conducted in the future. “In the future , academic and clinical nurses could establish partnerships channels , and more EBNP projects may generated.” (Participant 1 , Academic nurse) .
EBN manuals
EBN manuals may be the important output of APPs-EBN course for undergraduate nursing students. “If academic and clinical nurses collaborate to develop EBN course , they could create some manuals including case reports , teaching manuals or reference books to ensure teaching quality and homogeneity.” (Participant 5 , Academic nurse) .
Almost all the participants considered that six positive outcomes were short-term and long-term goals of APPs-EBN course for undergraduate nursing students.
Improved EBN awareness
Improving EBN awareness among undergraduate nursing students was a crucial learning objective of APPs-EBN course for undergraduate nursing students. As a participant mentioned, “Improving EBN awareness among undergraduate nursing students and ensuring they recognize its significance and value is crucial.” (Participant 9 , Academic nurse) .
Improving EBN awareness among undergraduate nursing students would be beneficial for them to conduct EBNP in future clinical nursing work. “They (undergraduate nursing students) should understand the process of EBN. For example , they know what the meaning of evidence transformation. When they work in clinical nursing , they may encounter some clinical problems. At that time , they could conduct evidence retrieval instead of judging just based on experience.” (Participant 7 , Academic nurse) .
Improved EBN competence
Undergraduate nursing students could master the basic knowledge and skills of EBP through participating in APPs-EBN course.
“Undergraduate nursing students are able to develop PICO questions for clinical questions and conduct evidence implementation projects.” (Participant 8 , Academic nurse) . “Through this course , students (undergraduate nursing students) will master some EBN basic knowledge and technical skills , and then be able to apply these methods and competences in practice.” (Participant 2 , Academic nurse) .
Increased EBN projects
The EBN knowledge and skills would be improved for undergraduate nursing students after participating in APPs-EBN course. Undergraduate nursing students may conduct more EBNP projects in clinical nursing in the future.
“They (nursing undergraduate students) will have the skills to conduct EBNP projects in the future , especially the project of evidence implementation. This is the EBNP skill they need to possess after working in clinical nursing in the future.” (Participant 9 , Academic nurse) . “The long-term goal is that undergraduate nursing students can conduct EBNP projects in clinical nursing in the future , and to improve their existing clinical nursing practices.” (Participant 5 , Academic nurse) .
Improved quality of nursing care
Participants considered that undergraduate nursing students would conduct EBNP projects in clinical nursing, which was beneficial for improving patient satisfaction and quality of nursing care.
“Maybe these (EBNP) projects will bring some benefits to patients and improve the quality of nursing care.” (Participant 9 , Academic nurse) . “In the long-term goal , it may be that undergraduate nursing students could apply the methods of EBN into clinical nursing in clinical nursing in the future. These results of EBNP projects may improve the quality of nursing care and patients’ satisfaction.” (Participant 6 , Academic nurse) .
Improved professional identity
Participants mentioned that undergraduate nursing students would have professional identity improvement after conducting EBNP projects. “After conducting EBNP projects , many of undergraduate nursing students actually have a sense of feedback and value. Therefore , it may also enhance their professional identity and their own sense of value” (Participant 9 , Academic nurse) .
This study aimed to explore the academic and clinical nurses’ perceptions on APPs-EBN course for undergraduate nursing students based on practice-academic partnership logic model. In this study, the specific contents of inputs, activities, outputs, and outcomes could further enriching the theoretical framework for developing APPs-EBN education and provide the details for developing of APPs-EBN course for undergraduate nursing students [ 22 ].
The specific content of inputs in this study validates and supplements the results of this scoping review (including key stakeholder commitment, shared mission, time, instructional design, mutual trust, leadership support) [ 22 ]. The results of this study indicated the significance of EBN training and incentives in facilitating the implementation of APPs-EBN course for undergraduate nursing students, which was similar with existing study conducted by Dr. Chen [ 20 ]. Notably, most academic nurses a lack of nursing care experience, leading to a limited understanding of specific process and challenges associated with EBNP projects [ 36 ]. Some clinical nurses a lack of theoretical knowledge of EBN, others were inadequately prepared to engage in teaching EBN courses [ 5 , 31 , 37 , 38 , 39 ], potentially impacting the learning outcomes of undergraduate nursing students participated in EBN courses [ 40 , 41 ]. Therefore, strengthening the training of academic nurses in EBNP and clinical nurses in EBN theoretical knowledge was crucial for improving their basic knowledge, competences, and teaching quality of EBN course.
Developing and conducting of an APPs-EBN course for undergraduate nursing students requires active participation from both academic and clinical nurses in the teaching of APPs-EBN course [ 31 , 42 ]. Sufficient incentives have promoting effect on the participation of academic and clinical nurses in the teaching of APPs-EBN course, which similar with the results of existing research [ 20 , 43 ]. Academic and clinical institutions should develop incentives such as professional title promotion and performance rewards for academic and clinical nurses to promote partnerships in developing and implementing APPs-EBN course for undergraduate nursing students. Effective incentives may help academic and clinical nurses overcome obstacles related to develop APPs-EBN course for undergraduate nursing students, such as lack of time [ 20 ].
The results of this study indicated that developing and conducting APPs-EBN course for undergraduate nursing students needed academic and clinical nurses conduct activities of ongoing communication and share decision making, which was consistent with the results of a scoping review [ 22 ]. Academic and clinical nurses participate in developing APPs-EBN course and conduct ongoing communication and shared decision making through meetings or group discussions during the stages of course planning, course commencement, and evaluation are crucial for refining APPs-EBN course [ 44 ]. Continuous activities between both sides can also promote partnerships between academic and clinical nurses, which may strengthen the connection between academic and clinical sides [ 20 ].
EBNP projects and EBN manuals were the outputs in this study, which was similar with the results of the EBNP quality improvement initiative from the perspective of APPs-EBN [ 45 ]. After conducting APPs-EBN course for undergraduate nursing students, academic and clinical nurses would establish stable cooperative relationships and more nursing undergraduate students have the awareness and ability to conduct EBNP projects. This may lead to more EBNP projects conducted by academic nurses, clinical nurses, and nursing undergraduate students in the future [ 20 ]. In addition, academic and clinical nurses could create EBN manuals related to APPs-EBN courses for undergraduate nursing students based on teaching experiences and insights gained from conducting this course. EBN manuals may provide a theoretical foundation, enabling more nursing schools domestically and internationally to conduct APPs-EBN course for undergraduate nursing students.
Conducting APPs-EBN course for undergraduate nursing students could yield various positive outcomes, aligning with the results of the scoping review [ 22 ]. Short-term goals of APPs-EBN course for undergraduate nursing students may include improved EBN awareness and improved EBN, as high-quality EBN education stands as a crucial measure to attain these goals [ 8 ]. Undergraduate nursing students who possess awareness of and competence in EBN are better prepared to incorporate EBN methodologies into nursing practice. This preparation is crucial for advancing long-term goals such as increasing EBN projects, enhancing the quality of nursing care, and strengthening professional identity [ 46 , 47 ]. Therefore, it is recommended that nursing educators to provide comprehensive inputs and actively participate in activities when conducting APPs-EBN course for undergraduate nursing students. This approach could lead to the generation of outputs and realization of desired outcomes.
Strength and limitation
The participants involved in this study came from four distinct regions in China, all of them with different educational features. This diversity contributes to the universality of the results of this study.
The limitation of this study was that not all participants have experience in APPs-EBN. This is primarily from the scarcity of nursing colleges in China providing EBN courses for undergraduate students. Consequently, it becomes challenging to recruit academic and clinical nurses with sufficient experience in APPs-EBN to participate in this study. In addition, all of the clinical nurses in this study have master’s degree, primarily because the study was conducted in China. Most nursing schools at various universities in China have developed EBN courses only for graduate students, while undergraduate nursing students typically do not receive systematic EBN course [ 48 ]. In the future, it would be beneficial to target recruitment towards both academic and clinical nurses with adequate experience in APPs-EBN and varying education levels for further interviews. This approach aims to garner additional insights and refine the theoretical framework and specific APPs-EBN course.
In addition, the interviews were conducted through online videoconferencing meetings or face-to-face meetings due to the limitations of time and space. For the online videoconferencing meeting, we turned on the camera during the online interview and recorded it with the informed consent of the participants. However, the continuity and fluency of the interview were affected to some certain extent due to network interruption.
Conclusions
Developing and conducting of APPs-EBN course for undergraduate nursing students involves investing inputs (Key stakeholder commitment, Shared mission, EBN training, Time, Instructional design, Incentive, Mutual trust, Leadership support) and conducting activities (Ongoing communication and Share decision-making) may lead to outputs (Educational resource) and outcomes (Improved EBN awareness, Improved EBN competence, Increased EBN projects, Improved quality of nursing care, Improved professional identity).
Data availability
All the original data were shown in the results section of the maunscript.
Melnyk BM, et al. Evidence-based Practice Culture and Mentorship Predict EBP implementation, nurse job satisfaction, and intent to stay: support for the ARCC(©) model. Worldviews Evid Based Nurs. 2021;18(4):272–81.
Article PubMed Google Scholar
Alqahtani N, et al. Nurses’ evidence-based practice knowledge, attitudes and implementation: a cross-sectional study. J Clin Nurs. 2020;29(1–2):274–83.
Dagne AH, et al. Implementation of evidence-based practice and associated factors among nurses and midwives working in Amhara Region government hospitals: a cross-sectional study. Reprod Health. 2021;18(1):36.
Article PubMed PubMed Central Google Scholar
Wu Y, et al. Do educational interventions aimed at nurses to support the implementation of evidence-based practice improve patient outcomes? A systematic review. Nurse Educ Today. 2018;70:109–14.
Yoo JY, et al. Clinical nurses’ beliefs, knowledge, organizational readiness and level of implementation of evidence-based practice: the first step to creating an evidence-based practice culture. PLoS ONE. 2019;14(12):e0226742.
Article CAS PubMed PubMed Central Google Scholar
Lv Y, Geng L, Zeng Y, Wang H. Qualitative study on the difficulties experienced by nursing managers during evidence-based nursing practice. J Nurs Sci (China). 2021;36(11):60–2. https://doi.org/10.3870/j.issn.1001-4152.2021.11.060 .
Article Google Scholar
Zhao J, et al. Evidence-based practice implementation in healthcare in China: a living scoping review. Lancet Reg Health West Pac. 2022;20:100355.
PubMed PubMed Central Google Scholar
González LMP, Fonseca DA, Bermeo RNZ. Evidence-based practice competences in nursing students at a university in Colombia. Nurse Educ Today. 2021;107:105094.
Hou R. (2013). The Construction of Access Indicator System of Undergraduate Nursing—Students’Clinical Teacher in Henan Province. (Master) Zhengzhou University (China).
Institute of Medicine Committee on the Robert Wood Johnson Foundation Initiative on. The future of nursing, a.t.I.o.M. The future of nursing: leading change, advancing Health. National Academies Press (US); 2011.
Mthiyane GN, Habedi DS. The experiences of nurse educators in implementing evidence-based practice in teaching and learning. Health SA. 2018;23:1177.
Xu J, Guan Y, Shi H, Zhang Y, Zheng J, Wu C. Evidence-based practice education in undergraduate nursing students: a scoping review. Chin Jouranl Nurs Educ (China). 2022;19(3):277–83. https://doi.org/10.3761/j.issn.1672-9234.2022.03.01613 .
Keib CN, et al. Changes in nursing students’ perceptions of research and evidence-based practice after completing a research course. Nurse Educ Today. 2017;54:37–43.
Kim JS, Gu MO, Chang H. Effects of an evidence-based practice education program using multifaceted interventions: a quasi-experimental study with undergraduate nursing students. BMC Med Educ. 2019;19(1):71.
Cardoso D et al. The Effectiveness of an Evidence-Based Practice (EBP) Educational Program on Undergraduate Nursing Students’ EBP Knowledge and Skills: A Cluster Randomized Control Trial. Int J Environ Res Public Health, 2021. 18(1).
Rholdon R, et al. An embedded EBP project: Effect on student nurses’ practice, attitude, and knowledge. Teach Learn Nurs. 2021;16(2):110–5.
Chen Q et al. Differences in evidence-based nursing practice competencies of clinical and academic nurses in China and opportunities for complementary collaborations: a cross-sectional study. J Clin Nurs, 2022.
Ramis MA, et al. Theory-based strategies for teaching evidence-based practice to undergraduate health students: a systematic review. BMC Med Educ. 2019;19(1):267.
Beal JA. Academic-service partnerships in nursing: an integrative review Nurs Res Pract, 2012. 2012: p. 501564.
Chen Q et al. Academic and Clinical Nurses’ Perceptions and Experiences on Academic-Practice Partnership in Evidence-Based Practice: An Interpretive Description Journal of Nursing Management, 2023. 2023.
McClinton TD. A guided search: formulating a PICOT from assigned areas of inquiry. Volume 19. WORLDVIEWS ON EVIDENCE-BASED NURSING; 2022. pp. 426–7. 5.
Xia Y, et al. Academic-practice partnerships in evidence-based nursing education: a theory-guided scoping review. Nurse Educ Pract. 2023;73:103839.
Zhao Q, et al. Non-pharmacological interventions to prevent and treat delirium in older people: an overview of systematic reviews. Int J Nurs Stud. 2023;148:104584.
Rycroft-Malone J, et al. Collaboration and co-production of knowledge in Healthcare: opportunities and challenges. Int J Health Policy Manag. 2016;5(4):221–3.
De Geest S, et al. Academic service partnerships: what do we learn from around the globe? A systematic literature review. Nurs Outlook. 2013;61(6):447–57.
MacPhee M. Developing a practice-academic partnership logic model. Nurs Outlook. 2009;57(3):143–7.
Blum ER, Stenfors T, Palmgren PJ. Benefits of massive Open Online Course participation: deductive thematic analysis. J Med Internet Res. 2020;22(7):e17318.
Buus N, Perron A. The quality of quality criteria: replicating the development of the Consolidated Criteria for Reporting Qualitative Research (COREQ). Int J Nurs Stud. 2020;102:103452.
Su JJ, et al. Defining compassionate nursing care. Nurs Ethics. 2020;27(2):480–93.
Lasater K, Atherton IM, Kyle RG. Population health as a ‘platform’ for nurse education: a qualitative study of nursing leaders. Nurse Educ Today. 2020;86:104313.
Pedregosa S, et al. Effective academic-practice partnership models in nursing students’ clinical placement: a systematic literature review. Nurse Educ Today. 2020;95:104582.
Sukkarieh-Haraty O, Hoffart N. Integrating evidence-based practice into a Lebanese nursing baccalaureate program: challenges and successes. Int J Nurs Educ Scholarsh, 2017. 14(1).
Li S, Cao M, Zhu X. Evidence-based practice: knowledge, attitudes, implementation, facilitators, and barriers among community nurses-systematic review. Med (Baltim). 2019;98(39):e17209.
Wakibi S et al. Teaching evidence-based nursing practice to student nurses in developing countries: strategies for novice nurse educators. Int J Nurs Educ Scholarsh, 2020. 17(1).
Alving BE, Christensen JB, Thrysøe L. Hospital nurses’ information retrieval behaviours in relation to evidence based nursing: a literature review. Health Info Libr J. 2018;35(1):3–23.
Orta R, et al. Knowledge and competency of nursing Faculty regarding evidence-based practice. J Contin Educ Nurs. 2016;47(9):409–19.
Saunders H, et al. Practicing Healthcare professionals’ evidence-based practice competencies: an overview of systematic reviews. Worldviews Evid Based Nurs. 2019;16(3):176–85.
Camargo FC, et al. Competences and barriers for the evidence-based practice in nursing: an integrative review. Rev Bras Enferm. 2018;71(4):2030–8.
Cleary-Holdforth J. Evidence-based practice in nursing and midwifery: we are talking the talk, but are we walking the Walk? Worldviews Evid Based Nurs. 2020;17(2):94–7.
Lam CK, Schubert CF, Herron EK. Evidence-based practice competence in nursing students preparing to transition to practice. Worldviews Evid Based Nurs. 2020;17(6):418–26.
Lam CK, Schubert C. Evidence-based practice competence in nursing students: an exploratory study with important implications for educators. Worldviews Evid Based Nurs. 2019;16(2):161–8.
Gilliss CL, et al. Academic/clinical nursing integration in academic health systems. Nurs Outlook. 2021;69(2):234–42.
Speroni KG, McLaughlin MK, Friesen MA. Use of evidence-based Practice Models and Research Findings in Magnet-designated hospitals across the United States: National Survey results. Worldviews Evid Based Nurs. 2020;17(2):98–107.
Amaral C, et al. Patient Safety Training Programs for Health Care professionals: a scoping review. J Patient Saf. 2023;19(1):48–58.
PubMed Google Scholar
Otts JA, et al. Academic-practice Partnership to prevent and manage pressure injuries: an evidence-based Quality Improvement Initiative. J Wound Ostomy Cont Nurs. 2023;50(6):463–73.
Fu L, et al. Evidence-based practice competency and related factors among nurses working in Public hospitals. Inquiry. 2020;57:46958020927876.
André B, Aune AG, Brænd JA. Embedding evidence-based practice among nursing undergraduates: results from a pilot study. Nurse Educ Pract. 2016;18:30–5.
Jiao Y. Study on the status quo of evidence-based nursing quality of clinical undergraduate nurses and the construction of training contents (Master). Shanxi Medical University (China); 2017.
Download references
Acknowledgements
Not Application.
This work was supported by the Natural Science Foundation of Hunan Province (No.2022JJ40642) and the National Natural Science Foundation of China (No. 72104250).
Author information
Authors and affiliations.
School of Nursing, Shandong Xiehe University, Jinan, China
Guiyun Wang
Xiangya School of Nursing, Central South University, Changsha, China
Yuting Xia, Qirong Chen & Xirongguli Halili
The Third Xiangya Hospital, Central South University, Changsha, China
You can also search for this author in PubMed Google Scholar
Contributions
Study design: YX, HH, QC; Literature searching: YX, XH; Quality Appraisal: YX, HH, QC; Data extraction: YX, GW, QC; Study supervision: QC, GW, HH; Manuscript drafting: YX; Critical revisions for important intellectual content: YX, QC, HH, GW.
Corresponding authors
Correspondence to Yuting Xia or Hui Huang .
Ethics declarations
Ethics approval and consent to participate.
This study was approved by the Ethics Committee of school of nursing of Central South university, China (review number: E202313). Detailed explanations were provided concerning the recording procedures, and the interviewees were requested to sign an informed consent form before the interviews officially commenced, including the recording process.
Consent for publication
Competing interests.
The authors declare no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Supplementary Material 1
Rights and permissions.
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/ .
Reprints and permissions
About this article
Cite this article.
Wang, G., Xia, Y., Chen, Q. et al. Exploring academic and clinical nurses’ perspectives on evidence-based nursing course for undergraduates from perspectives of academic-practice partnerships: a qualitative study. BMC Nurs 23 , 657 (2024). https://doi.org/10.1186/s12912-024-02223-1
Download citation
Received : 16 April 2024
Accepted : 02 August 2024
Published : 15 September 2024
DOI : https://doi.org/10.1186/s12912-024-02223-1
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Academic-practice partnerships
- Evidence-based nursing
- Undergraduate nursing students
- Perceptions
BMC Nursing
ISSN: 1472-6955
- General enquiries: [email protected]

COMMENTS
The importance of evidence based practice is to enable nurses to provide high quality care, improve outcomes for patient and families and to run a more efficient health service. Therefore other agencies within the health service will benefit when interventions and care is based on research (Burns & Grove 2007).
Nursing EBP Topics You Can Use in Your Essay. Here are some of the latest evidence-based practice nursing research topics that you can use in your essay or explore further in your own research: The impact of telehealth on patient outcomes in primary care; The use of music therapy to manage pain in post-operative patients
Top 5 Benefits To The Nurse. 1. Evidence-based practice in nursing provides nurses with scientifically supported research to help them make well-educated decisions. 2. EBP in nursing helps nurses stay up-to-date about new nursing interventions and protocols used in patient care. 3.
Evidence-Based Practice (EBP) in nursing is a method of making clinical decisions based on the best available current research, clinical expertise, and patient preferences. This approach integrates the most relevant and up-to-date scientific evidence with clinical expertise and patient values to provide the highest quality of care.
5 min read • June, 01 2023. Evidence-based practice in nursing involves providing holistic, quality care based on the most up-to-date research and knowledge rather than traditional methods, advice from colleagues, or personal beliefs. Nurses can expand their knowledge and improve their clinical practice experience by collecting, processing ...
"First of all, evidence-based practice is the use of hospital protocols, guidelines and training manual for health care service especially when we give patient care and do procedures. It is a matter of reading books and search for research findings. ... Worldviews on Evidence-Based Nursing. 2014 Oct; 11 (5):274-83. doi: 10.1111/wvn.12051 ...
Evidence-based practice is now widely recognized as the key to improving healthcare quality and patient outcomes. Although the purposes of nursing research (conducting research to generate new knowledge) and evidence-based nursing practice (utilizing best evidence as basis of nursing practice) seem quite different, an increasing number of research studies have been conducted with the goal of ...
Table 1: Developing evidence‐based practice guidelines and a nursing illustration (adapted from Proctor and Rosen, 2004) Step Illustration Step 1: Locate evidence‐based interventions relevant to the outcomes of interest. The nurse is interested in helping patients to manage their asthma better. Three
Evidence-based practice (EBP) is firmly established as an essential component of nursing practice. Despite being present in some form in all nursing roles, its presence is arguably more prominent in professional nursing settings (RN). The RN's responsibilities include planning patients' care, analyzing their medical history, and ...
7. Offer suggestions for future research on evidence-based practice in nursing. EBP Research Paper Literature Review Writing- Evidence-Based Practice (EBP) Evidence-based practice (EBP) is an approach to nursing that focuses on using evidence to guide clinical decisions. EBP is effective in improving patient outcomes and reducing healthcare costs.
The problems with the uptake and effective implementation of EBP led to the emergence of the EIP concept. This concept is based on the premise that healthcare practice should, as a matter of principle, be informed by, rather than based on, evidence (Nevo and Slonim-Nevo, 2011). This implies that other forms of evidence (for example, patient experiences, the nurse's expertise and experiences ...
Development of literature-based models for Bachelor's degree essays and evaluation of students' experiences. Qualitative Action ... Educational interventions on evidence-based nursing in clinical practice: a systematic review with qualitative analysis. Nurse Educ Today. 2016; 43:50-59. doi: 10.1016/j.nedt.2016.04.023. [Google Scholar] 10. ...
The impact of evidence based practice has been brought into nursing through education, practice, and science over the last decade. Evidence based practice provides quality care to patients that is effective, safe, and efficient. Evidence based practice promises moving care to a high level of producing the intended health outcome for the patients.
Evidence-Based Nursing should therefore be exceptionally useful, and its target audience of practitioners is a refreshing move in the right direction. The worlds of researchers and practitioners have been separated by seemingly impenetrable barriers for too long. 4. Tiptoeing in the wake of the movement for evidence-based medicine, however, we ...
EBP is a process used to review, analyze, and translate the latest scientific evidence. The goal is to quickly incorporate the best available research, along with clinical experience and patient preference, into clinical practice, so nurses can make informed patient-care decisions (Dang et al., 2022). EBP is the cornerstone of clinical practice.
Background Evidence-based practice (EBP) is imperative for ensuring patient safety. Although teaching strategies to enhance EBP knowledge and skills are recommended, recent research indicates that nurses may not be well prepared to apply EBP. A three-level hierarchy for teaching and learning evidence-based medicine is suggested, including the requirement for interactive clinical activities in ...
In order to make a decision about implementing evidence into practice, nurses need to be able to critically appraise research. Nurses also have a professional responsibility to maintain up-to-date practice.1 This paper provides a guide on how to critically appraise a qualitative research paper. Qualitative research concentrates on understanding phenomena and may focus on meanings, perceptions ...
Evidence-based practice is "integrating the best available evidence with the healthcare educator's expertise and the client's needs while considering the practice environment.[1] One of the roles of the NPD practitioner in the 2022 edition of the Nursing Scope and Standards of Practice is a champion for scientific inquiry. In this role, the NPD practitioner promotes a spirit of inquiry ...
The main goal of lifelong learning is to enable health professionals to be up to date with the rapid development of evidence-based information. Lifelong learning is an essential part of professionalism for health care professionals (Novak et al., 2014). Lifelong learning entails the ability to deal with issues through inquiry, seeking resources ...
In this essay, it will be discussed how lifelong learning and the ability to use evidence-based practice as a nurse is essential to develop professionally. I will be focussing on learning styles and theories that can help with lifelong learning. Likewise, I will discuss the importance of developing emotional intelligence as a student nurse.
According to Frewin and Court (2009), evidence-based practice is a systematic research that envisages the integration of external clinical evidence in exercising individual clinical expertise. Barclay, (2012) defined clinical expertise as the cumulative clinical skills, education and experience at the disposal of a clinician.
Models of Evidence-Based Practice. Multiple models of EBP are available and have been used in a variety of clinical settings. 16-36 Although review of these models is beyond the scope of this chapter, common elements of these models are selecting a practice topic (e.g., discharge instructions for individuals with heart failure), critique and syntheses of evidence, implementation, evaluation ...
Aim To explore nurses' perceptions of evidence-based nursing courses for undergraduates through academic-practice partnerships. Design A deductive thematic analysis based on the practice-academic logic model. Methods Fifteen academic and clinical nurses were interviewed between November and December 2023, either online or through face-to-face meetings. Each interview lasted 20-30 min. The ...