- Open access
- Published: 04 March 2019

Organ transplantation in the modern era
- Dmitri Bezinover ORCID: orcid.org/0000-0003-4384-8899 1 &
- Fuat Saner 2
BMC Anesthesiology volume 19 , Article number: 32 ( 2019 ) Cite this article
14k Accesses
47 Citations
8 Altmetric
Metrics details
Peer Review reports
Organ transplantation (OT) is one of most successful advances in modern medicine. For patients with end stage disease, transplantation most often provides their only chance for survival. Even before the first transplant was performed, it was clear that OT could only be successful with a multidisciplinary approach. The history of OT has involved a series of breakthroughs in medicine that has influenced all aspects of health care. As you will see, for nearly a century, the contributions of specialists in anesthesiology and critical were largely underrepresented in the worlds literature.
Short history of organ transplantation
The earliest descriptions of OT can be found in ancient Greek, Rome, Chinese, and Indian mythology involving bone, skin, teeth, extremity, and heart transplantation [ 1 , 2 ]. In the sixteenth century, Italian surgeon Gasparo Tagliacozzi used skin transplant for plastic reconstruction. He was the first to describe what we now know is an immunologic reaction when the graft is obtained from a different person. It was only at the end of nineteenth century that OT research began to be both more systematical and better documented. The first animal models (usually dogs) were developed at this time. Early in the twentieth century, French surgeon Alexis Carrel (who later move to the US) developed a new method for vascular anastomoses. Dr. Carrel performed several successful kidney transplants in dogs, developed an approach for vessel reconstruction, and began the practice of cold graft preservation. In 1912 Dr. Alexis Carrel was awarded the Nobel Prize in Physiology or Medicine for his pioneering work [ 3 ]. The first human to human transplant was performed in 1933 in the Soviet Union by the Ukrainian surgeon U.U. Voronoy. The blood group mismatched graft was obtained six hours after the donor’s death and although the patient survived two days, the graft never produced urine [ 3 , 4 ]. Despite significant surgical developments, OT was not very successful due to a lack of knowledge in immunology.
The next significant breakthrough in OT came as a result of the work of the British biologist Sir Peter Brian Medawar. His specialty was immunology. During World War II, he worked in the Burn Unit of Glasgow Hospital and investigated problems associated with skin homograft transplantation. For his research on graft rejection and acquired immune tolerance, Dr. Medawar was awarded the Nobel Prize for Physiology or Medicine in 1960 and is considered the father of transplantation.
Between 1951 and 1952, Hume et al., performed nine kidney transplants at the Brigham Hospital in Boston [ 5 ]. Despite the use of cortisone for immunosuppression, all grafts were rejected. This problem was successfully overcome by Dr. Thomas Murray who, in identical twins, performed the first successful kidney transplant. The recipient survived 8 years with normal graft function. Dr. Murray received the Nobel Prize for Medicine in 1990. This first success sparked significant enthusiasm in researchers and clinicians in the field of OT. In 1963, after extensive experimental work in animal models, Dr. James Hardy performed the first lung transplant in Jackson, Mississippi. The patient survived for 18 days without any evidence of rejection. Internationally, over the next 10 years, a number of lungs were transplanted. They all had poor outcome related primarily to problems with the healing of surgical anastomoses. The first attempt at liver transplantation occurred in 1963 by Dr. Thomas Starzl, and in 1967, he completed the first successful liver transplant at the University of Colorado. One year later, the first European liver transplant was performed by Dr. Roy Calne in England. Also in 1967, Dr. Christiaan Barnard transplanted the first human heart in South Africa. The recipient was 53 years old and survived for 18 days. Over the next 12 months, more than 100 heart transplants were performed worldwide [ 6 ]. Unfortunately, overall survival was poor primarily due to the lack of effective immunosuppression.
In the 1950s, the first attempts at immunosuppression for kidney transplantation involved total irradiation and was met with some degree of success [ 7 , 8 ]. The use of chemical immunosuppression, initially with 6-mercaptopurine and then with combination of azathioprine and steroids, avoided the problems associated with irradiation and improved outcomes significantly. It was the discovery of cyclosporine in 1976, and its introduction in clinical practice in 1984, that dramatically changed the landscape of OT resulting in an increased one-year survival in both kidney and liver transplant recipients (95 and 75% respectively). Modern immunosuppressive agents (tacrolimus, sirolimis, mycophenolic acid, and everolimus), allow us to currently enjoy superior outcomes and a reduction in adverse immunosuppressive effects.
The next important milestone in the development of OT was the founding of the United Network of Organ Sharing (UNOS) in 1984. This organization manages all transplant activities in the US including the maintenance of a national transplant list for all types of transplantation, data collection, and coordination of educational activities. There are a number of organizations in Europe and Asia with similar responsibilities.
Despite significant contributions in the success of OT, the role of Anesthesia and Critical Care in OT has not always been recognized. As well-known as the names of the first transplant surgeons (Thomas Starzl, Ray Calne, and Russel Strong) are, it is unfortunate that few people are aware that Dr. Antonio Aldrete not only introduced the Postanesthesia Recovery Score and developed the first prototype of the needle for combine spinal/epidural anesthesia but also performed anesthesia for the first liver transplant. Dr. Aldrete was involved in more than 180 liver transplants and described his experience in many publications and lectures. Dr. Thomas Starzl recognized his work as extremely important for the success of transplantation but unfortunately his name is almost forgotten in the history of OT.
In 1992, a group of anesthesiologists and critical care specialists, under leadership of Dr. Yoogoo Kang from the University of Pittsburgh, proposed the creation of a multidisciplinary society to meet the educational needs of medical professionals involved in transplantation and improve the quality of care for transplant recipients. The first two meetings which focused on preoperative care, were held in Pittsburgh in 1984 and 1986. After the success of these first meetings, The International Society for Perioperative Care in Liver Transplantation was created in 1990. It was subsequently re-named The International Liver Transplantation Society (ILTS). At about the same time in Europe, Dr. John Farman founded the Liver Intensive Care Group of Europe (LICAGE). Most recently (2016) The Society for the Advancement of Transplant Anesthesia (SATA) was founded. Today, specialists in Anesthesia and Critical Care increasingly have leadership roles in national and international transplantation societies.
Specific contributions of anesthesia and critical Care in Organ Transplantation
Advances in anesthesia and critical care, primarily in preoperative evaluation and optimization, intraoperative management, and postoperative care have contributed significantly to the success of OT. The most important contributions have been made in:
Establishing evaluation and treatment protocols for transplant candidates with comorbidities including CAD, cirrhotic and alcoholic cardiomyopathy, porto-pulmonary hypertension and hepato-pulmonary syndrome, as well as recommendations for the management of hyponatremia
Introducing the use of perioperative ultrasound and intraoperative TEE monitoring
The management of coagulopathy, including recommendations on the use of viscoelastic testing and on transfusion component therapy
Evaluation and management of perioperative hemodynamic instability including post-reperfusion and vasoplegic syndromes
The management of infections in the immunosuppressed patient
Despite these contributions, transplant anesthesia as a subspecialty is rarely represented at national anesthesia meetings. The situation is similar with the major anesthesia journals. This is changing. Anesthesia and Perioperative Care for Solid Organ Transplantation is a new section in BMC Anesthesiology and was established to provide the opportunity for anesthesiologists and critical care specialists to present their work in the field of OT. The Section Editors, Drs. Saner and Bezinover have many years of experience in transplantation. They are experts in the field of perioperative care for these very challenging patients and are actively involved the transplant societies ILTS, LICAGE, and The Transplantation Society (TTS).
Challenges in organ transplantation
Many challenges remain in the field of OT and provide fertile ground for research. The primary challenge in transplantation today for all organ types is the disproportion between organ demand and organ availability. Strategies to overcome this problem include transplantation using extended criteria grafts (ECD), donation after cardiac death (DCD), the use of machine perfusion for graft preservation of inferior quality (or initially discarded) grafts, as well as the use of living donors and split liver grafts. Additional challenges involve perioperative patient care, graft survival, and optimization of immunosuppression protocols. There are several ongoing studies in these areas. There are, however, some specific challenges associated with transplantation of individual organs.
Kidney transplantation
There are several areas of research specifically aimed at increasing organ availability and survival to include: optimization of ex-vivo machine graft perfusion and protocols for using extended criteria grafts, preoperative candidate evaluation, graft and recipient matching, pretreatment of recipients (using ischemic preconditioning) and donors (using mild hypothermia) [ 9 ]. To help alleviate the shortage of kidneys for transplantation, UNOS has recently introduced a paired donation kidney transplant pilot program. This program helps people who have identified (incompatible) living donors find well-matched donors and receive a transplantation.
Liver transplantation
Several strategies have been developed to increase organ availability include living donor liver transplantation (LDLT), split liver transplantation, and utilization of ECD and DCD grafts. The regenerative ability of liver is well known, however in contrast to renal grafts, living donation of hepatic grafts is significantly more complicated and puts the donor at greater risk as well. Today, several countries have established LDLT programs with South Korea, Turkey, Japan, and the US being leaders in the field.
Split liver transplantation also offers the possibility to perform two transplantations using one donor. Unfortunately, this option is limited due to the small size of the grafts and can be used only for children and smaller adults.
Other potential options to increase graft availability is the use of ECD, DCD and initially discarded grafts. Utilization of these organs (especially DCD) is not as high as could be due to their lower quality in comparison to donation after brain death organs. There are two major problems associated with transplanting DCD grafts: primary non-function of the transplanted organ [ 10 , 11 ] and intrahepatic biliary strictures (as a result of ischemic cholangiopathy) [ 12 ] due to prolonged warm ischemia time which is unavoidable with DCD donors. Nevertheless, utilization of these grafts is growing. It has been demonstrated that machine perfusion (both normo- and hypothermic) [ 13 , 14 , 15 ] during graft preservation can significantly increase their quality, resulting in successful transplants.
Hepatic replacement therapy is also an important area of research. There are a number artificial or bioartificial systems under investigation that may be used as a bridge to transplantation. Hepatocyte transplantation (cell suspension from unused hepatic tissue) also has demonstrated some promise [ 16 ]. Currently, these systems have limited efficacy and are topics of ongoing investigations. A bioengineered liver is a future concept and is currently under intensive development [ 17 ].
Pancreas transplantation
The first successful pancreas-kidney transplant was performed in 1966 by Drs. Richard Lillehei and William Kelly at the University of Minnesota. They performed the first singular pancreas transplant in 1968. The pancreas-kidney transplant procedure is very common today due to the high incidence of diabetic nephropathy associated with diabetes mellitus. Isolated islet transplantation is being performed with increasing frequency and is the topic of much ongoing research.
Intestinal transplantation
The first attempts at transplanting intestines were performed in 60s. These initial attempts, however, were not successful with the majority patients succumbing to rejection, infections, and surgical complications. Only after introduction of cyclosporine (and later tacrolimus) did intestinal transplantation become possible. The first successful intestine transplant was performed in 1988 by Dr. E. Deltz in Germany. Intestinal transplantation can be performed alone or as a part of multi-organ procedure. Despite significant improvements in survival, rejection and cytomegalovirus infections are still significant problems. The refinement of existing immunosuppressive protocols and the development of new drugs is a priority of research in this field.
Heart and lung transplantation
The use of both DCD cardiac and pulmonary grafts was started in the US in 1993. Even though DCD hearts and lungs have been successfully transplanted, [ 18 , 19 ], the risks associated with using these lower quality grafts is very high. Graft perfusion during preservation (usually normothermic but also hypothermic) of these organs has been demonstrated to be beneficial [ 18 , 20 , 21 , 22 ].
Other approaches currently in use for cardiac transplantation is acceptance of organs with mild coronary artery disease (CAD) and the use of previously grafted hearts.
Other areas under investigation include preventing and managing chronic rejection, preventing postoperative infection and malignancy, optimization of postoperative outcome, refining surgical techniques, and improving cardiac recovery assessment of donors after hypoxemic events.
On the horizon
Xenotransplantation is not new, however, renewed interest in this area is growing and may prove to be a solution for many problems associated with organ storage. In the early 90s, Dr. Thomas Starzl performed 2 baboon to human liver transplants. There remains many unsolved physiological, microbiological, and immunological problems associated with this type of transplantation currently under investigation.
Face, uterus, and extremity transplants have recently demonstrated with some success and will likely be performed with greater frequency in the future. Certainly, the long-term outcome of these patients has to be evaluated.
The new BMC Anesthesiology section, Anesthesia and Perioperative Care for Solid Organ Transplantation, was established to provide the opportunity for specialists involved in the care of transplant patients to submit their manuscripts on these topics. We would like to invite Anesthesiologists and Critical Care specialists, as well as all other specialists involved in OT, to submit manuscripts for consideration to this new section of BMC Anesthesiology.
Abbreviations
Coronary artery disease
Donation after cardiac death
Extended criteria grafts
International Liver Transplantation Society
Living donor liver transplantation
Liver Intensive Care Group of Europe
Organ transplantation
Society for the Advancement of Transplant Anesthesia
The Transplantation Society
United Network of Organ Sharing
Shayan H. Organ transplantation: from myth to reality. J Investig Surg. 2001;14:135–8.
Article CAS Google Scholar
Bergan A. Ancient myth, modern reality: a brief history of transplantation. J Biocommun. 1997;24:2–9.
CAS PubMed Google Scholar
Barker CF, Markmann JF. Historical overview of transplantation. Cold Spring Harb Perspect Med. 2013;3:a014977.
Article Google Scholar
Linden PK. History of solid organ transplantation and organ donation. Crit Care Clin. 2009;25:165–84 ix.
Hume DM, Merrill JP, Miller BF, Thorn GW. Experiences with renal homotransplantation in the human: report of nine cases. J Clin Invest. 1955;34:327–82.
Watson CJ, Dark JH. Organ transplantation: historical perspective and current practice. Br J Anaesth. 2012;108(Suppl 1):i29–42.
Murray JE, Merrill JP, Dammin GJ, Dealy JB Jr, Walter CW, Brooke MS, Wilson RE. Study on transplantation immunity after total body irradiation: clinical and experimental investigation. Surgery. 1960;48:272–84.
Hamburger J, Vaysse J, Crosnier J, ., Auvert J, Lalanne C, Hopper J: Transplantation of a kidney between nonmonozygotic twins after irradiation of the receiver. Good function at the fourth month. Presse Med 1959, 67:1771–1775.
Google Scholar
Niemann CU, Feiner J, Swain S, Bunting S, Friedman M, Crutchfield M, Broglio K, Hirose R, Roberts JP, Malinoski D. Therapeutic hypothermia in deceased organ donors and kidney-graft function. N Engl J Med. 2015;373:405–14.
Casavilla A, Ramirez C, Shapiro R, Nghiem D, Miracle K, Bronsther O, Randhawa P, Broznick B, Fung JJ, Starzl T. Experience with liver and kidney allografts from non-heart-beating donors. Transplantation. 1995;59:197–203.
D'Alessandro AM, Hoffmann RM, Knechtle SJ, Odorico JS, Becker YT, Musat A, Pirsch JD, Sollinger HW, Kalayoglu M. Liver transplantation from controlled non-heart-beating donors. Surgery. 2000;128:579–88.
Abt P, Crawford M, Desai N, Markmann J, Olthoff K, Shaked A. Liver transplantation from controlled non-heart-beating donors: an increased incidence of biliary complications. Transplantation. 2003;75:1659–63.
Dutkowski P, de Rougemont O, Clavien PA. Machine perfusion for 'marginal' liver grafts. Am J Transplant Off J Am Soc Transplant Am Soc Transplant Surg. 2008;8:917–24.
Fondevila C, Hessheimer AJ, Ruiz A, Calatayud D, Ferrer J, Charco R, Fuster J, Navasa M, Rimola A, Taura P, et al. Liver transplant using donors after unexpected cardiac death: novel preservation protocol and acceptance criteria. Am J Transplant Off J Am Soc Transplant Am Soc Transplant Surg. 2007;7:1849–55.
Compagnon P, Levesque E, Hentati H, Disabato M, Calderaro J, Feray C, Corlu A, Cohen J, Mosbah IB, Azoulay D. An oxygenated and transportable machine perfusion system fully rescues liver grafts exposed to lethal ischemic damage in a pig model of DCD liver transplantation. Transplantation. 2017;101:e205–13.
Dhawan A, Puppi J, Hughes RD, Mitry RR. Human hepatocyte transplantation: current experience and future challenges. Nat Rev Gastroenterol Hepatol. 2010;7:288–98.
Ko IK, Peng L, Peloso A, Smith CJ, Dhal A, Deegan DB, Zimmerman C, Clouse C, Zhao W, Shupe TD, et al. Bioengineered transplantable porcine livers with re-endothelialized vasculature. Biomaterials. 2015;40:72–9.
Dhital KK, Iyer A, Connellan M, Chew HC, Gao L, Doyle A, Hicks M, Kumarasinghe G, Soto C, Dinale A, et al. Adult heart transplantation with distant procurement and ex-vivo preservation of donor hearts after circulatory death: a case series. Lancet. 2015;385:2585–91.
Erasmus ME, van Raemdonck D, Akhtar MZ, Neyrinck A, de Antonio DG, Varela A, Dark J. DCD lung donation: donor criteria, procedural criteria, pulmonary graft function validation, and preservation. Transpl Int. 2016;29:790–7.
Loor G, Howard BT, Spratt JR, Mattison LM, Panoskaltsis-Mortari A, Brown RZ, Iles TL, Meyer CM, Helms HR, Price A, et al. Prolonged EVLP using OCS lung: cellular and acellular Perfusates. Transplantation. 2017;101:2303–11.
Sage E, Mussot S, Trebbia G, Puyo P, Stern M, Dartevelle P, Chapelier A, Fischler M. Foch lung transplant G: lung transplantation from initially rejected donors after ex vivo lung reconditioning: the French experience. Eur J Cardiothorac Surg. 2014;46:794–9.
Messer S, Large S. Resuscitating heart transplantation: the donation after circulatory determined death donor. Eur J Cardiothorac Surg. 2016;49:1–4.
Download references
Acknowledgements
No funding was received for preparation of this papier.
Availability of data and materials
Not applicable.
Author information
Authors and affiliations.
Department of Anesthesiology and Perioperative Medicine, Penn State College of Medicine, The Pennsylvania State University- Milton S. Hershey Medical Center, 500 University Drive, Hershey, PA, 17033-0850, USA
Dmitri Bezinover
Department of General-, Visceral- and Transplantation Surgery, Essen University Medical Center, Hufelandstr 55, 45147, Essen, Germany
You can also search for this author in PubMed Google Scholar
Contributions
DB performed historical research and was a major contributor in writing the manuscript. FS was a major contributor in writing the manuscript. Both authors read and approved the final manuscript.
Corresponding author
Correspondence to Dmitri Bezinover .
Ethics declarations
Ethics approval and consent to participate, consent for publication, competing interests.
The authors are section editors for BMC Anesthesiology.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License ( http://creativecommons.org/licenses/by/4.0/ ), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated.
Reprints and permissions
About this article
Cite this article.
Bezinover, D., Saner, F. Organ transplantation in the modern era. BMC Anesthesiol 19 , 32 (2019). https://doi.org/10.1186/s12871-019-0704-z
Download citation
Received : 06 February 2019
Accepted : 25 February 2019
Published : 04 March 2019
DOI : https://doi.org/10.1186/s12871-019-0704-z
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
BMC Anesthesiology
ISSN: 1471-2253
- General enquiries: [email protected]
Thank you for visiting nature.com. You are using a browser version with limited support for CSS. To obtain the best experience, we recommend you use a more up to date browser (or turn off compatibility mode in Internet Explorer). In the meantime, to ensure continued support, we are displaying the site without styles and JavaScript.
- View all journals
- Explore content
- About the journal
- Publish with us
- Sign up for alerts
- Published: 05 May 2021
Organ donation and transplantation: a multi-stakeholder call to action
- Raymond Vanholder ORCID: orcid.org/0000-0003-2633-1636 1 , 2 ,
- Beatriz Domínguez-Gil 3 ,
- Mirela Busic 4 ,
- Helena Cortez-Pinto 5 , 6 , 7 ,
- Jonathan C. Craig 8 ,
- Kitty J. Jager 9 ,
- Beatriz Mahillo 3 ,
- Vianda S. Stel 9 ,
- Maria O. Valentin ORCID: orcid.org/0000-0003-4381-1332 3 ,
- Carmine Zoccali 10 , 11 &
- Gabriel C. Oniscu ORCID: orcid.org/0000-0003-1714-920X 12 , 13
Nature Reviews Nephrology volume 17 , pages 554–568 ( 2021 ) Cite this article
26k Accesses
107 Citations
29 Altmetric
Metrics details
- Renal replacement therapy
- Social sciences
Although overall donation and transplantation activity is higher in Europe than on other continents, differences between European countries in almost every aspect of transplantation activity (for example, in the number of transplantations, the number of people with a functioning graft, in rates of living versus deceased donation, and in the use of expanded criteria donors) suggest that there is ample room for improvement. Herein we review the policy and clinical measures that should be considered to increase access to transplantation and improve post-transplantation outcomes. This Roadmap, generated by a group of major European stakeholders collaborating within a Thematic Network, presents an outline of the challenges to increasing transplantation rates and proposes 12 key areas along with specific measures that should be considered to promote transplantation. This framework can be adopted by countries and institutions that are interested in advancing transplantation, both within and outside the European Union. Within this framework, a priority ranking of initiatives is suggested that could serve as the basis for a new European Union Action Plan on Organ Donation and Transplantation.
Differences in the frequency of transplantation between countries in the European Union suggest that there is room for improvement, wherein countries with low transplantation rates could learn from the experience of countries that are doing well.
Efforts to increase transplantation rates require a variety of strategies, including approaches to increasing living and deceased donation, improving coordination of the donation and intensive care unit processes, increasing graft quality and optimizing expanded donation criteria.
Education should cover the complete spectrum of society (the general population, patients and medical professionals) with specific outreach methods to under-represented communities and individuals who are health illiterate.
Infrastructural and financial barriers to transplantation should be banned.
Similar content being viewed by others
The paradox of haematopoietic cell transplant in Latin America

Cost-effectiveness of transplanting lungs and kidneys from donors with potential hepatitis C exposure or infection

Validation of a survival benefit estimator tool in a cohort of European kidney transplant recipients
Introduction.
Organ transplantation improves patient survival and quality of life and has a major beneficial impact on public health and the socio-economic burden of organ failure. In the European Union (EU), a relatively coherent and structured approach to transplantation exists, with well-developed national programmes, international schemes to facilitate organ sharing and well-defined exchange policies 1 , making Europe a leader in the field. Between 2009 and 2015, the EU operated a successful Action Plan to promote organ donation and transplantation 2 . However, transplantation rates today differ markedly between EU countries, suggesting that there remains room for improvement. To address the differences, the European Commission convened a Thematic Network coordinated by the European Kidney Health Alliance ( EKHA ), tasked with providing guidance to increase organ donation and transplantation and presenting key action points that would increase the prevalence of patients living with a functioning transplant throughout Europe. This thematic network culminated in the publication of a joint statement that recommends strategies to promote transplantation and donation in the EU and, by extension, throughout Europe 3 . Although the focus of this statement is on adult and paediatric transplantation of solid organs, many recommendations are also applicable to tissue transplantation (for example, cornea).
This Roadmap summarizes and builds on the Joint Statement and the experience gained from implementation of the earlier Action Plan to recommend strategies through which transplantation activities and the number of individuals living with a functioning transplant in Europe can be enhanced. We outline the challenges posed by the development and implementation of a EU-wide transplantation strategy and propose 12 key areas in which specific measures should be considered to promote transplantation, providing an overall framework that can be adopted by countries and institutions to improve rates of donation and transplantation (Fig. 1 ). These areas were selected and defined by a group of experts, including members of professional organizations, and authorities from national health-care bodies. As the Joint Statement is a product of a European Commission initiative, most of the recommendations herein are aimed at improving the current status of transplantation within the EU, but importantly these recommendations are also relevant to the 17 EU-associated countries and to regions elsewhere in the world, with some adaptations to local conditions if required.
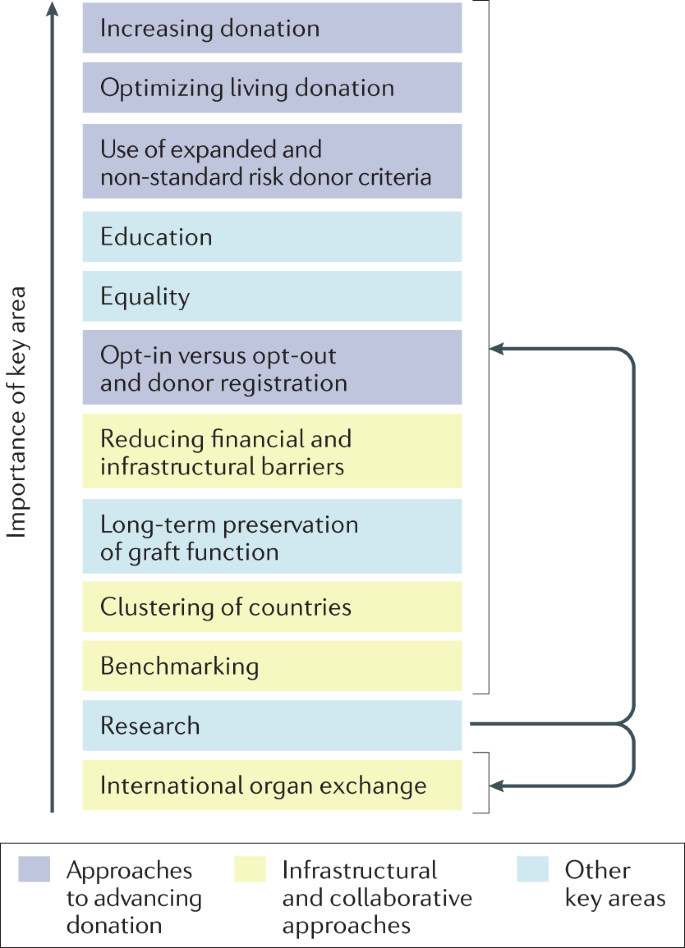
These topics have been ranked in order of priority; however, this ranking should be considered with caution as it represents a subjective judgement by the authors of this Roadmap, possibly biased by confounding factors such as region of residence, precise involvement and responsibility in transplantation activity, personal opinion and extent of solid evidence base. Furthermore, given the variations discussed in the Roadmap, the ranking of these topics may vary between different countries or stakeholders. In addition, the topics are highly interdependent (as illustrated by colour coding) and cannot be considered in isolation. Research is linked to all topics.
Current status of transplantation in Europe
Non-communicable (chronic) diseases (NCDs) impose a substantial burden on health-care systems, economies, quality of life, employment status and social activities. In Europe, NCDs are responsible for 77% of the disease burden and 86% of deaths 4 , many of which are in young individuals 5 . Changes in population demographics and the growing prevalence of risk factors have contributed to an increase in the demand for organ replacement therapies. Artificial organ support is an option in some instances, but is only available on a large scale for kidney failure in the form of dialysis. Hence, transplantation is for many patients the only solution to restoring organ function and preventing premature death. The WHO has urged countries to progress towards self-sufficiency in transplantation, first by preventing NCDs and their progression to end-stage organ failure, but also through the provision of sufficient numbers of life-saving transplants to match their need 6 , 7 . The WHO further emphasizes that deceased donation should be developed to its maximum therapeutic potential.
More than 34,285 solid organ transplantations were performed in the EU in 2019, 85% of which were kidney (21,235) and liver (7,900) transplants. Cardiothoracic transplantation represented 13% of activity with 2,269 hearts and 2,136 lungs transplanted, whereas pancreas (2%), small bowel and multi-visceral transplants represented only a small fraction (Table 1 ; Fig. 2 ). Although the total number of annual transplantations rose by 4,540 between 2010 and 2017, the number of annual transplantations from 2017 to 2019 increased by only 161, indicative of a stagnation in transplantation activity, possibly related to the end of the EU Action Plan in 2015 (Fig. 2 ).
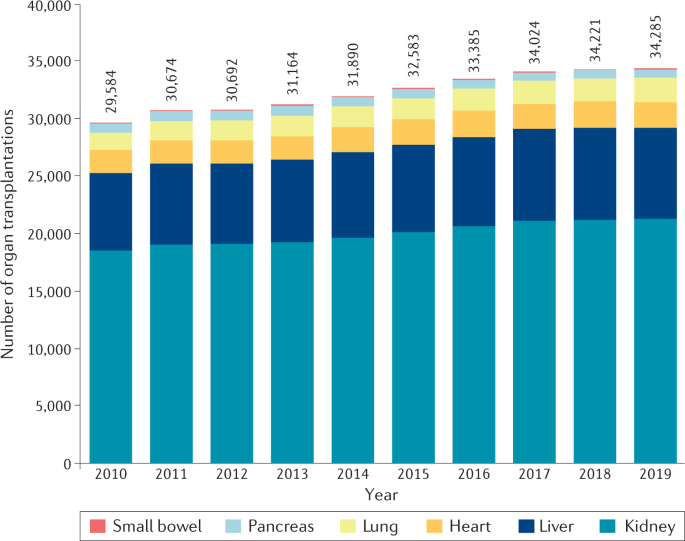
As Croatia was not part of the EU in 2010–2011, the data for transplantations performed in Croatia were added to the data for the 27 EU member states for those years. The absolute total number of transplantations for each year is provided. The corresponding number per million population increased from 59 (2010) to 67 (2019). The EU Action Plan on Organ Donation and Transplantation was operational between 2009 and 2015. The marked rise in yearly transplantation rate observed particularly in the last years of the EU Action Plan on Organ Donation and Transplantation (2012–2015) seems to have levelled off in the years 2016–2019. Data were calculated based on data from the Transplant Newsletter 135 .
Transplantation of organs from deceased donors remains the most prevalent form of transplantation throughout the EU. Although deceased donor transplantation occurs most frequently from donors declared dead by neurological criteria (donation after brain death; DBD), donation after death declared by circulatory criteria (donation after circulatory death; DCD) contributes to transplant activity in a number of countries 8 (Table 2 ; Fig. 3 ). However, substantial variability exists in the use of DCD transplantation between EU member states. DCD is not permitted in a number of European countries because of legislative and ethical obstacles 9 , 10 , and practiced in only a few cases in many other countries 8 . In 2019, 28 of 35 European countries had an active DCD programme compared with just 10 in 2011 (ref. 10 ), but in several of these countries the DCD activity was marginal (Fig. 3 ). In 2019, DCD contributed to 17.8% of deceased donation transplantations in the EU. Living donation (almost exclusively kidney and liver), which is particularly beneficial to paediatric recipients, represents a considerable proportion of transplant activity in some but not all European countries 8 (Tables 1 , 2 ; Figs 3 , 4 ).
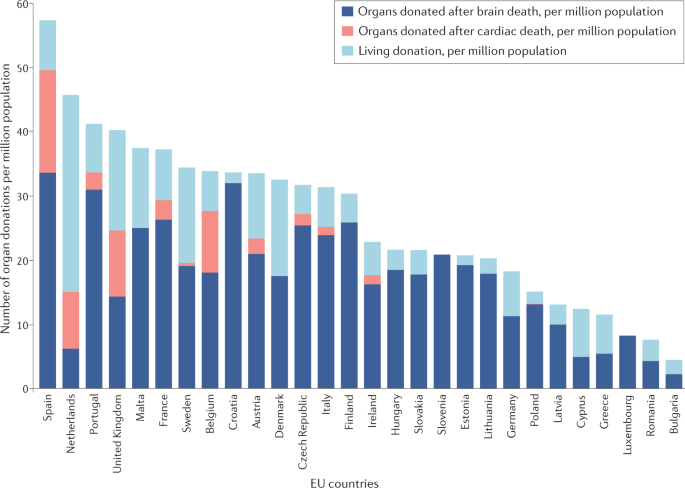
Substantial differences exist between EU countries in terms of their overall rates of donation but also in terms of the specific types of donation. Only 11 of the 28 countries (39%) use notable quantities of organs donated after cardiac death. Although all EU countries perform transplantation after living donation, substantial differences in the rates of living donor transplantation exist between countries. Data were calculated based on data from the Transplant Newsletter 135 .
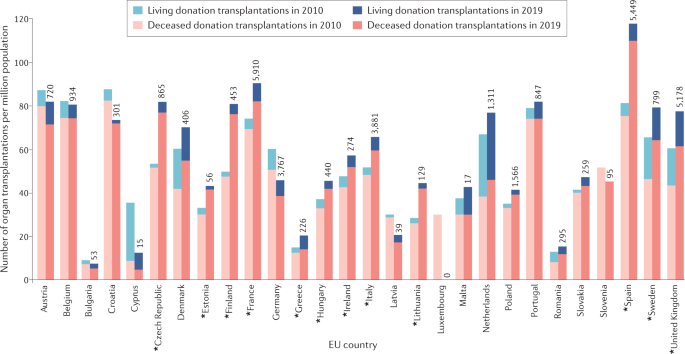
Of 28 countries, 12 (43%) showed an increase in transplantation activity of >20% (asterisks). Although most countries tended to increase or stagnate their rates of transplantation, a few show a decrease. Also shown are the absolute numbers of transplants (from deceased plus living donors) in 2019. Data were calculated based on data from the Transplant Newsletter 135 .
The number of organ transplant procedures for the EU as a whole was 67.2 per million population in 2019, with marked differences between countries 8 , 11 (Fig. 3 ), reflecting differences in local health-care processes, efforts to develop living and deceased organ donation, available infrastructure and expertise, and economic factors 12 . Most EU member states have seen an upward trend in transplantation rates over the past decade, but some countries have seen a substantial decrease (Fig. 4 ). These decreases are in some cases influenced by external factors, such as public mistrust 13 , and have negative consequences on patient outcomes 8 , 11 .
For most vital organs (liver, heart, lungs), transplantation is the only life-saving therapy. For patients with kidney failure (also known as end-stage kidney disease), which is rapidly rising in the ranked order of fatal diseases 14 , kidney transplantation offers not only a better survival and quality of life than dialysis 15 , 16 , 17 , but can be life-saving when vascular access options are lost. Yet, by the end of 2019, more than 58,000 patients were waiting for an organ transplant in the EU (Fig. 5 ). Yearly, 3–4% of those on the waiting list die before being transplanted, representing 10–11 patient deaths daily 8 . This figure is probably an underestimate, owing to incomplete data reporting in some countries. The mismatch between the need for transplants and donor supply, which excludes patients from lifesaving treatment, is exacerbated by the rising prevalence of health problems, such as diabetes mellitus and obesity, which reduces the donor pool; the presence of major public health challenges, such as the current COVID-19 pandemic; and improvements in critical care processes or car safety, which prevent deaths but also reduce the pool of deceased organ donors. The problems associated with access to donor organs are further illustrated by the small proportion of patients who receive a pre-emptive kidney transplant, which in most countries represents <10% of patients starting kidney replacement therapy 18 , necessitating a variable period on dialysis with a negative impact on survival and high associated costs 19 .
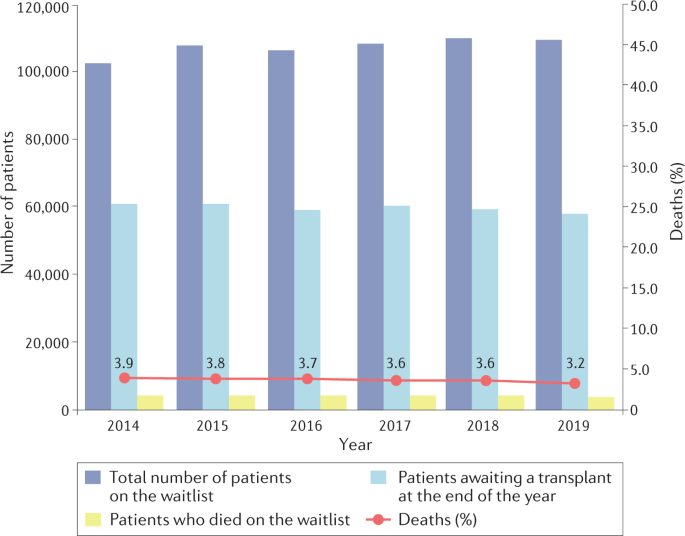
The percentage of deaths (red line) is calculated as the ratio of those who died that year while waitlisted to the total number active on the waiting list that year multiplied by 100. There was a 7% increase in the number waitlisted over this 5-year period. The percentage of deaths remained relatively stable between 3–4%. Data were calculated based on data from the Transplant Newsletter 135 .
Of note, NCDs also present a considerable health economic burden through a life-long need for consultations, medication, surgery, imaging, interventions and hospitalization. It is difficult to quantify the economic impact of organ transplantation in the absence of large-scale artificial organ treatment as an alternative option. However, for kidney failure, for which dialysis consumes at least 2% of health expenditure for only 0.1–0.2 % of the general population 1 , transplantation is by far the most cost-effective kidney replacement option, particularly from the second year post-transplantation 20 , 21 . Economic evaluations for other solid organ transplants are less straightforward. Costs associated with liver transplantation can be substantial, particularly in the context of biliary complications that can increase the duration of hospitalization and the need for diagnostic studies and further therapeutics 22 . Nevertheless, liver transplantation has been reported to be cost effective 23 in comparison with the rapidly rising costs of non-transplanted liver disease (including costs of medication, radiological procedures, and repeated and prolonged hospital admissions) 24 . Heart failure is a leading cause of morbidity and mortality worldwide and places a huge burden on health-care systems; available data suggest that heart transplantation is also cost-effective in eligible adult and paediatric recipients 25 , 26 .
Unemployment among patients with chronic NCDs generates pressure not only on social security but also on productivity and buying power 27 . Transplantation can interrupt this vicious circle, although pro-active mechanisms are needed to promote socio-economic (re)integration of individuals following transplantation, as 40–80% of transplanted patients remain unemployed or permanently disabled 28 , 29 , 30 .
Finally, patients with NCDs also experience a heavy burden of polypharmacy, diet restrictions, comorbidities, and time spent in hospital and travelling to medical appointments. Transplantation restores not only organ function but also quality of life 20 , 31 . For children, transplantation also leads to improvement in development, growth, education and mental health in the recipient and in quality of life for the carer 32 .
The benefits of transplantation prompted the EU to launch the Action Plan on Organ Donation and Transplantation, which aimed to increase organ availability, enhance efficiency and accessibility of transplant procedures, and improve the quality and safety of organs intended for transplantation. It was implemented from 2009 to 2015 (refs 2 , 33 ). At the end of 2019, a 16% overall increase in transplantation rate was observed compared with 2010 8 (Table 1 and Fig. 2 ). This increase varied for different types of transplants (for example, 42% increase for lung transplantation, 17% for liver and 15% for kidney transplantation) and was primarily a result of a substantial increase in DCD 8 , suggesting that DBD and living donation may also benefit from further stimulatory interventions. Moreover, the initial rise in transplantation rate observed after 2012 seems to have somewhat levelled off in the past few years (Fig. 2 ), suggesting that the effect of the EU Action Plan has lost some momentum and that a new plan may be needed.
Data specific to kidney transplantation show that implementation of the Action Plan was associated with a rise in the total number of kidney transplantations and in the percentage of patients living with a functioning kidney graft in the EU (Supplementary Table 1 ). However, marked differences between countries are evident, underscoring the need for further action to boost transplantation rates in some regions.
Topics for action
Variations in transplantation practices and policies between European countries have led to differences in access to transplantation; in some instances, patients who may benefit from transplantation are not considered eligible (for example, owing to age or the presence of comorbidities or mental health issues) 34 . The optimal approach to increasing transplantation rates is to set well defined, ambitious goals, such as an aggregated increase in the number of EU transplantations by 10% in 10 years, complemented by specific development plans that detail the elements required to support individual countries or groups of countries according to the local conditions. This strategy should be followed by an implementation plan at a national level with internal and external auditing. Several organizations, such as the Council of Europe, have previously formulated recommendations and resolutions to increase transplantation at the institutional level (summarized in Supplementary Table 2 ). This Roadmap is complementary to those efforts and extends these initiatives by outlining a comprehensive multinational policy approach 33 , 35 , 36 . Barriers to transplantation 37 , 38 , which are often psychological and practical in nature, may be avoided through appropriate education and regulation 2 (Box 1 ).
Lessons can also be learned from countries that are performing well. For example, measures taken by Spain to increase rates of deceased organ donation 39 , 40 , 41 over recent decades have had remarkable success 8 (Supplementary Figure 1 ). These measures have included a strong emphasis on coordinating the donor process, use of a pyramidal structure to coordinate processes from local to regional and national offices, engagement of the critical care community, benchmarking, provision of guidance and continuous professional training, and the increased use of living donation, expanded donor criteria and DCD organs 39 , 40 , 41 . Regions such as Croatia, Northern Italy, the UK and France, which adapted the Spanish model to their local circumstances, also saw an increase in transplantation rates 42 , enabling these regions to focus on equality of access and approaches to optimizing outcomes and education. Other countries, such as the Netherlands, have also increased their transplantation rates substantially, largely through increasing rates of living donation (Supplementary Table 1 ).
Herein we summarize 12 key domains that informed the Joint Statement commissioned by the European Commission 3 and in which action could enable further increases in the number of donations, transplantations and patients living with a functioning transplant. These topics form the basis of a Roadmap that is intended for use by the EU, EU health-care authorities, patient associations and professional societies to guide the implementation of measures to stimulate organ donation and transplantation. Beyond increasing rates of organ donation and transplantation, the involved communities should do their utmost to maximize the longevity of transplanted organs, which is an absolute priority for the recipients 43 , 44 . To guide implementation of strategies that address each of these areas, we have ranked the 12 key topics in order of importance (Fig. 1 ). Of note, however: this ranking should be considered with caution given that it is largely opinion based, given the variation in the extent to which each of these areas may need to be addressed differently in different countries, and the interdependent nature of the areas, such that they can only be considered and implemented together. The highly integrated nature of these areas renders it near impossible to disaggregate and quantify the potential impact of individual interventions within a topic. However, all examples provided within this Roadmap refer to countries with a high transplantation rate (>60 per million population per year).
Box 1 Non-medical barriers to transplantation
Barriers at the patient level
Attitude, role perception, motivation
Distrust of health-care professionals
Lack of knowledge
Fears and concerns
Fear of rejection or graft failure
Fear of surgery
Fear of medication or adverse effects
Previous negative experiences (self or others)
Fear for the living donor’s health
Sociocultural background
Religious reasons that oppose transplantation
Unsuitable living circumstances
Shortcomings in patient efforts or investments
Reluctance to ask potential living donors
Lack of social support
Lack of adherence or hygiene
Barriers at the level of the health-care professional
Lack of knowledge and expertise
Difficulty in selecting patients
Lack of communication skills
Barriers at the level of the health-care system
Financial barriers
Lack of support staff
Competition with other treatment modalities
Patient doing well on other treatment modalities
Adapted with permission from refs 2 , 136 , the European Kidney Health Alliance.
Increasing donation
Increasing the number and quality of donated organs is a key element in increasing donation rates. Several strategies exist to facilitate this donation process.
Maximizing the role of donor coordinators
Proper coordination of the donation process is a key element in increasing donations and optimizing outcomes. The European models that have been most successful centre around the involvement of efficient donor coordinators, who are independent of the transplantation team, and are based in each hospital that has potential for deceased donation. These coordinators have key roles in the steps leading to the traditional model of deceased donation — a process that involves potential donor selection, maintenance of the haemodynamic status of the donor and organ perfusion, diagnosis of death and communication with the family. These individuals are trained in recognizing donation opportunities in end-of-life care pathways and in providing grieving families with the psychological support required to make the often difficult decision to agree to donation. Critical to the overall success of these programmes has been the appointment of professionals who develop a proactive programme for the identification of possible donors, in close cooperation with the critical care community. Donor coordinators should receive continuous training, with special attention given to the skills required to communicate with grieving relatives and organize organ handling with minimal delay. Local networks should be supported by national and regional cells that focus more on policy and technical aspects 39 . Regular internal and external audits should be used to identify areas for improvement 39 .
Optimizing the role of intensive care professionals
Engagement with intensive care professionals is particularly important to ensure that deceased donation is always considered as an option for patients receiving end-of-life care, provided that it is appropriate and consistent with the potential donor’s wishes and values 45 , 46 . Optimizing the role of intensive care professionals in the donation process requires a number of steps, including the identification of intensivists who will champion donation in their unit and in their hospital or region as a whole as well as lead education efforts; training of all intensive care staff in approaches to identifying possible organ donors on the basis of simple triggers (that is, the identification of individuals who have died or are likely to die imminently in a condition compatible with organ donation); maintenance of organ viability until donation; ensuring timely referral to donor coordinators; and ensuring an appropriate and consistent approach to the families of potential donors 46 .
Minimizing the duration of the donation process
The time between consideration of donation opportunities and initiation of the actual donation procedure can vary considerably and can exceed 24 h sometimes substantially 47 . Hesitation in donor identification and donor handling by medical staff as well as indecision of families owing to socio-cultural, religious or educational barriers 48 all affect the duration of the donation process, as do organizational factors such as the length of the process before an organ is offered to a potential recipient, the need for additional tests and lack of timely access to surgical theatres. These delays may have adverse effects on donation by increasing the risk of donor organ deterioration or withdrawal of family consent, leading to the loss of otherwise transplantable organs. Therefore, national programmes should focus on approaches to facilitating the identification of all possible donors, the early notification of donor coordinators and work with families to reduce the rate of donation refusal 49 , thus avoiding donor loss.
Optimizing living donation
Transplantation of a kidney from a living donor offers markedly better chances for graft and patient survival than transplantation of a kidney from a deceased donor 50 , whereas living donor liver transplantation involves a similar hospital stay and survival rates to deceased donor transplantation 51 . Although practiced in almost every EU country, living donation has a variable contribution to overall transplantation activity. It is markedly low in many countries, even in those with well-established transplantation programmes, with the Netherlands and Iceland as notable exceptions (Figs 3 , 4 , Supplementary Table 1 ). Living donation remains the method of choice for infants and children, in particular for those with kidney failure, because it enables pre-emptive transplantation and avoids the need for dialysis. In the Netherlands, kidney transplantation is largely driven by living donation, making it a country with one of the highest proportion of patients on kidney replacement therapy living with a functioning transplant in the EU (Supplementary Table 1 ).
Donor safety remains paramount and should be the primary focus of any living donation programme. However, it is equally important to demystify the risks of living donation, through a uniform process of information (for both the donor and recipient) and evaluation (via an online approach if convenient) to ensure that all essential information is conveyed and understood 52 (see below and Supplementary Box 1 ). This approach will encourage expansion of living donation programmes, increasing access to transplants for patients from ethnic minorities and economically challenged backgrounds who are often disadvantaged overall in transplantation programmes (see below). Living kidney donors may have a low but increased risk of developing hypertension 53 or kidney failure 54 , and therefore robust living donor programmes should carefully select donors, include an adequate follow-up, and if needed, preventive treatment. Moreover, and in contrast to the experience of many organ donors 55 , the donation process should be financially neutral. Processes therefore need to be in place to ensure that living donors do not face out-of-pocket costs and lost wages, or difficulty securing health or life insurance 56 .
Approaches to broadening donor and recipient criteria, including the involvement of emotionally related and unrelated altruistic donors and organ-sharing schemes , enable the expansion of living donation programmes. Although sharing schemes exist in a number of EU countries such as in the Netherlands and Spain, they remain non-existent or very limited in others 8 , 57 , 58 . Of note, a number of European and cross-border organ-sharing initiatives have been implemented to redress this situation 59 , 60 .
The implementation of initiatives to encourage living donation raises organizational and ethical questions, which have been addressed in a reference toolkit developed by the European Commission and National Agencies 61 . Any common ethical framework for unrelated living donation should be regulated at an EU level to alleviate any concern that pressure may be exerted on the candidate donor to benefit an irreversibly sick person and alleviate the associated societal costs 62 .
Use of expanded donor criteria
The term ‘expanded criteria donor’ is commonly applied to donors whose clinical–demographic characteristics would have an impact on the quality of the organ and its expected longevity. The traditional definition of an expanded criteria kidney donor includes age >60 years or age >50 years with at least two of the following: a history of hypertension, serum creatinine level >1.5 mg/dl (132.6 µmol/l) or death from cerebrovascular accident 63 . However, this dichotomous definition has increasingly been replaced by risk scores to guide the categorization and use of all organs (liver, kidney, pancreas) 64 , 65 , 66 . The increased use of expanded criteria donor organs and the changing profile of the potential donor pool has led to the increased use of organs from donors with a high comorbidity burden (for example, donors with diabetes mellitus). For patients with kidney failure, these organs can improve survival compared with remaining on dialysis 67 . Dual kidney transplantation (whereby both kidneys from a donor are transplanted into a recipient) can also allow the use of organs from marginal (for example, older) donors 68 .
DCD organs have in the past been considered to yield inferior post-transplant results compared with those achieved with DBD donor organs. However, increased experience has led to the attainment of appropriate post-transplantation outcomes with DCD organs 69 , 70 . Efforts can be required to overcome the legal and ethical barriers to DCD transplantation, such as the absence of a legal framework regulating the cessation of therapy, and to increase the confidence of transplantation professionals in the outcomes obtained with the use of DCD organs. Advances in organ perfusion protocols may be required to better preserve DCD organ quality and prevent the unnecessary discarding of suitable organs 71 , 72 , 73 ; however, the role of in situ and ex situ preservation strategies and the type of organs that require these interventions require further study 73 .
Non-standard risk donors are defined as those with specific conditions or diseases (for example, infections or malignancies) that can potentially affect the safety of the transplant recipient. Transplantation of these organs can be appropriate provided that an individualized risk-assessment is performed and that recipients are properly selected 74 . Examples of this scenario include the use of organs with unusual anatomy but appropriate functionality (Supplementary Box 2 ), transplantation of HIV-infected grafts into recipients with HIV 75 , or transplantation of hepatitis C virus (HCV)-infected grafts into HCV-negative recipients — a process that is now possible with the use of direct-acting antiviral agents 73 , 76 . For heart transplantation alone, full use of all available organs from HCV-positive donors would increase the transplantation rate by about 3% 77 . Thus, the combined use of all available donor expansion measures could increase transplantation rates substantially.
EU countries that provide a legal framework for euthanasia are the Netherlands, Luxembourg, Belgium and as of June 2021, Spain. Organ donation after euthanasia in those countries is medically possible and thus represents a further option to provide these patients with the opportunity of organ donation and to expand the donor pool 78 , 79 .
Despite satisfactory outcomes 10 , 69 , 70 , many expanded and non-standard criteria donor organs remain underused in European countries 8 , 10 , 80 , 81 . An analysis from the USA demonstrated that the transplanted counterparts of >15% of unilaterally discarded donor kidneys showed a death-censored 5-year survival >85% 82 . Thus, discarded organs have the potential to contribute substantially to the donor organ pool and their use should be supported through the provision of information to health professionals about the benefit of using them and to the potential recipient, highlighting the benefits and risks of alternative choices. The rate of organ discard in Europe might be reduced by the application of risk score systems to guide the identification of suitable organs and appropriate recipients 83 .
Several countries have implemented educational tools to promote organ donation and transplantation (Supplementary Box 1 ). A more harmonized approach across the EU could result in further structural improvements.
Improving communication skills of health-care professionals
Communication training should in particular focus on professionals involved in the early stages of the deceased donation process — such as emergency and intensive care physicians and donor coordinators 45 , 84 . Communication training should cover both sides of the donation and transplantation process; donor coordinators and professionals in intensive care should be trained in approaches to communicating with the families of possible donors, whereas transplantation professionals should be trained in approaches to communicating with potential recipients in an informative and efficient way. Information on the benefits and practical aspects of transplantation should be embedded in the curricula of all health practitioners, from medical students to postgraduate teaching of specialists and general practitioners (Supplementary Box 1 ). Specific involvement of health-care professionals trained in patient education as part of the treating team is extremely helpful.
Education of the public
Insufficient public awareness of organ donation and transplantation 85 , 86 , including the concept of brain death 87 , necessitates continuous education. A highly efficient strategy involves use of mass and social media, and requires the building of active partnerships with journalists 41 . Education activities in schools and use of flyers or web-based tools may help to increase awareness. In Croatia, information pamphlets with answers to frequently asked questions are made available to the public, whereas in Finland, an online educational tool is provided to educate patients and the general public about kidney transplantation (Supplementary Box 1 ). The EKHA “Gift of life” campaign 88 offers advice to policy makers and citizens on approaches to promoting organ donation. This campaign stresses the need for a coordinated European approach based on appropriate legal and structural frameworks to allow individuals and professional nephrology and patient societies to promote kidney transplantation at the national policy level in an equitable way throughout Europe with respect to the local cultural background 88 . Such initiatives that focus on organ donation as a whole would further public education about the benefits and processes of transplantation.
Additional barriers that exist in economically or socially disadvantaged groups, including those with a low level of educational attainment, refugees, migrants and under-represented communities, should be specifically addressed with the help of patients, patient organizations, and minority communities, to understand attitudes and develop strategies and ensure equitable access to transplantation (see later) 39 . This aspect is particularly important as patients from these groups are generally over-represented on the transplant waiting list and under-represented in the donor population. Limited willingness to donate exacerbates the challenge of finding suitable HLA matches for kidney transplant candidates, prolonging the wait-list time, increasing the risk of mismatch, and jeopardizing long-term outcomes 89 .
Patient education and information
Limited health literacy (discussed below) and patient disinformation also deter transplantation 90 . The information provided by physicians and nurses to candidate organ recipients should discuss all treatment options, especially for kidney transplant candidates, for whom dialysis is a readily available but in many cases a less desirable alternative. Information about deceased and living donation 2 should be provided, as often no information is offered about the two options (Supplementary Table 3 ). Education about organ replacement options should be provided as patients approach organ failure and be delivered in a tailored way either in hospital, in outpatient clinics or at home (Supplementary Box 1 ). Patient records should include an explicit statement on the suitability of the patient for transplantation, including the views of the patient and, particularly in the case of living donation, the views of their next of kin. To improve long-term patient outcomes 91 , 92 , education should include lifestyle advice, particularly approaches to addressing excess weight, smoking, excessive alcohol intake and hypertension and to promoting a healthy diet and exercise.
In 2017, EKHA distributed a questionnaire to determine the satisfaction level of patients from six EU countries with the information that had been provided to them about the different types of kidney replacement therapy in the period preceding the start of those therapies 2 (Supplementary Table 3 ). Patient dissatisfaction with the quality of information provided about transplantation ranged from 11% (the Netherlands) to 45% (Greece). These data confirmed findings from a previous analysis 93 of data collected from 2010 to 2011, suggesting little change since then, and underscoring the need for streamlined European education for all transplant candidates. A centralized quality check on information delivery and patient satisfaction might encourage excellence. Not surprisingly, dissatisfaction about the information provided coincides with low application of a given practice, suggesting a self-fulfilling circle (for example, in the Netherlands, which has a high transplantation rate, patient satisfaction is also very high; however, proportionally more patients received only information on living donation, which very likely occurred because that is the preferred mode of donation in that country).
Achieving equality in transplantation requires that all suitable candidates — irrespective of their ethnicity, race, sex, education, socio-economic status, religion, health literacy, or language barriers — have an equal probability of receiving a transplant. However, inequalities are rife in medical practice 94 and deserve specific attention. Approaches to removing barriers to transplantation can in many instances be adapted to the specific needs of minority patient groups, as exemplified by the implementation of measures to increase access to transplantation for Jehovah’s Witnesses in Croatia (Supplementary Box 3 ). However, despite the existence of legal frameworks designed to prevent discrimination and ensure equitable access to health care and transplantation, in practice, access to transplantation remains extremely problematic for certain populations, especially for minority groups and immigrants, including undocumented migrants. These individuals face considerable barriers in access to health care, in particular to chronic therapies, including transplantation services. These barriers can arise from willing or unwilling institutional discrimination, the bias and prejudices of health professionals, as well as from non-familiarity of migrants with the medical model of the host country 94 , 95 . Educational approaches developed for the general public may not be appropriate for these communities, and specific efforts are required to ensure that these approaches reach affected individuals and are developed with input from the relevant populations. Comorbidities, such as diabetes, can be more prevalent in some ethnic minority populations, and negatively affect donation and transplantation rates 96 . Inequities among migrant populations are also closely linked to socio-economic status, exemplified by the well-documented associations between socio-economic status, waitlist placement and receipt of a transplant 97 . In the USA, African Americans, Hispanics and individuals of Asian ancestry are less likely than white Americans to receive a deceased donor kidney transplant 89 . In the UK, individuals of Asian and African Caribbean ancestry comprise 8% of the general population but 23% of the kidney transplant waitlist 98 , 99 . In the USA, the fact that the proportion of waitlisted patients vastly exceeds the number of available organs from donors of the same ethnicity has prompted adaptations of the kidney transplant allocation system, for example, by calculating the wait time from the start of dialysis instead of start of waitlisting, and by prioritizing the most sensitized patients 89 . These measures have reduced disparities in access to transplantation by increasing the proportion of actively waitlisted patients from under-represented communities and by decreasing inactive waitlisting of these individuals. These observations indicate that international and national authorities as well as professional organizations should provide regulations or recommendations to avoid discrimination in the selection process of donors and recipients for transplantation.
Disparities in access to transplantation among under-represented communities can also arise from a lower awareness of donation and transplantation processes, religious or cultural distrust of local medical professionals, fear of racism, linguistic obstacles, a lack of awareness of service availability, financial constraints, and a lack of perception of mainly asymptomatic chronic illnesses, such as kidney failure 95 , 100 . Given the importance of ethnicity as a determinant of tissue compatibility between donor and recipient, educational programmes aimed at increasing outreach to under-represented populations and at overcoming cultural or linguistic barriers are of critical importance. Although tissue matching is less important a determinant for liver or cardiothoracic transplantation than for kidney transplantation, the cultural and societal concerns are also evident in this setting.
Other subgroups, such as infants and highly sensitized individuals, also experience barriers to transplantation. Dedicated transplantation programmes, such as those that focus on identifying donor organs of appropriate size or on detecting appropriate donors using specific cross-matching methods, are needed 101 .
Finally, women are more likely to become a living donor than to receive a living organ donation 102 . Moreover, transplant recipients — irrespective of whether the organ is from a living or deceased donor — are predominantly male, especially for kidney transplants 103 . Although this inequality in access to transplantation might reflect a sex bias in the incidence of pathologies necessitating transplantation 104 , psychological and socio-economic factors also contribute to this disparity 105 , and could be prevented by addressing aspects of the transplantation system, such as inequalities in selection for waitlisting or unbalanced prioritization scores, that disadvantage women 105 .
Opt-in versus opt-out and donor registration
Considerable variation in legal frameworks for donation exists across the EU. Several EU and EU-associated countries, including Ireland, Germany, Denmark, Estonia and Switzerland, use opt-in legislation whereby consent for donation needs to be specifically sought from the donors and/or their families. Other countries apply an opt-out system (that is, consent for donation is presumed, unless the potential donors have officially registered their refusal). The Netherlands has in the past few years transitioned to an opt-out system, whereas the German government was unsuccessful in making this step. Most European countries that use an opt-out system apply a ‘soft approach’, allowing for objections by family members but supported by moral and legal leverage provided by the policy acceptance of the opt-out approach.
Compared with opt-in systems, opt-out systems are associated with higher donor rates ranging from 23.3% to 61.5% according to some studies 106 , 107 . However, a 2019 study of 35 countries found no difference in transplantation rates between opt-out and opt-in systems 108 . Multivariate analyses performed as part of that study showed that opt-out systems were independently predictive of lower rates of living donation. The divergent findings of studies that have compared opt-in and opt-out policies may be attributable to residual confounding resulting from differences in definitions, the selection of countries analysed, the period of analysis, or the choice of adjustment factors. Although there seems to be a gradual shift towards the use of opt-out systems, available data suggest that this approach as such is not sufficient to increase transplantation rates, and thus the adoption of opt-out legislation should be accompanied by other measures 109 , such as all those outlined in this Roadmap. In addition, simplified donor registration procedures such as those applied in Italy (Supplementary Box 4 ) offer an approach to encouraging donation without imposing judicial pressure 110 .
Financial and infrastructural barriers
Clinical activity related to transplantation should be subject to fair remuneration. Insufficient reimbursement to hospitals for deceased donation and organ retrieval is a major issue in some countries and may adversely affect donation rates. In many countries, the reimbursement for different kidney replacement therapies is disproportionate, such that dialysis is financially more rewarding than transplantation for care providers.
In the USA, for example, patients who receive dialysis at units managed by for-profit organizations have a lower chance of undergoing transplantation than patients treated at not-for-profit units 111 , 112 . Although difficult to extrapolate these findings to the EU, this suggests that the current imbalance in financial yield between different kidney replacement therapies can jeopardize transplantation rates, but also that differences in economic models governing health care should be considered by health-care administrations to incentivize transplantation over other approaches. For example, additional reimbursement could be given to units that have achieved high rates of transplantation among their population of patients with end-stage organ failure (Supplementary Box 5 ).
Furthermore, expansion of transplantation programmes should be supported by investment in adequate infrastructure. Recommendations for optimal infrastructure requirements and staffing of transplantation and intensive care units — including optimal numbers of surgeons, operating theatres, intensive care facilities, appropriate hospitalization and outpatient follow-up facilities, and well-trained nursing and medical staff — are all urgently needed.
Long-term preservation of graft function
Long-term preservation of graft function is the most important outcome for transplant recipients 43 . Maintenance of graft function entails avoidance of damage by rejection, medication, complications, comorbidities, or damage to other organs (for example, avoiding kidney damage in heart or liver transplant recipients due to immunosuppressive medication), but also requires specific attention to fatal outcomes or complications that might jeopardize future transplantation procedures (such as opportunistic infections, malignancy, cardiovascular disease, post-transplantation diabetes mellitus) 50 , 113 . In the first 10 years after transplantation mortality is substantially higher than that of the general population, at around 40% 114 , with a similar percentage of fatalities over the subsequent 10 years 50 , 115 . In addition, at least 15% of survivors lose function of the transplanted organ per decade 116 . Of note, despite a consistent improvement in kidney graft survival in the first 5 years post-transplant between 1986 and 2015, graft survival after the fifth year of transplantation has not substantially changed over time 116 .
Several aspects of the transplantation process should be addressed to maximize the likelihood of transplant survival. Cold ischaemia time is an important modifiable risk factor for poor transplant outcomes 117 , 118 , 119 , and it is imperative that transplantation logistics are constantly reviewed and improved to keep cold ischaemia time as short as possible. Controlling organ fibrosis may be one of the few solutions to preventing long-term graft loss, but therapeutic solutions to tackle this problem are scarce 120 . For recipients of kidney transplants experiencing graft loss, timely and uncomplicated transition onto dialysis is essential, as mortality is high in the period of dialysis (re-)initiation 121 . Non-adherence to medication is a major contributor to graft loss 122 , 123 and interventions that augment adherence increase graft survival 124 . Monitoring markers of immunosuppression can also help to individualize immunosuppressive therapy to maximize drug efficacy and minimize toxicity 125 , 126 .
A critical consideration for paediatric transplant recipients is their transition to adult transplantation clinics. This transition period can be associated with reduced compliance related to the change in environment, as differences in the approach and philosophy of adult transplantation clinics may be perceived as inhospitable by adolescents who are often psychologically and socially vulnerable 127 .
A significant number of graft-survival years are lost when young donor kidneys are transplanted into older recipients and vice versa 128 . Matching the life expectancy of the intended recipient with the projected life span of the transplant is likely to maximize graft survival and cost savings 128 . Complex algorithms are required to ensure optimal matching and account for differences in population demographics. Other factors that affect long-term organ function, such as the presence of low-level preformed donor-specific HLA antibodies require further study 129 . The role of lifestyle factors and the possible role of tailored medication also deserve further consideration.
Clustering of countries
Some countries have a strong track record in living donation and others in deceased donation, but few do both well. Similarly, some may be more successful than others at transplanting specific organs. Several countries could benefit from improving their donor coordination and recruitment processes and/or from adopting or improving expanded donation criteria. Specific scenarios should be developed according to the areas that require improvement, with countries grouped according to these characteristics. Even countries that perform well overall have room for further improvement, as exemplified by Spain, which manages to improve every year upon already high transplantation rates (Supplementary Figure 1 ).
Clustering of countries with similar needs and characteristics can streamline the development of action plans that enable different strategies for each cluster. These action plans should also account for country-specific measures and include in-depth consultation with the local transplant communities, including National Competent Authorities, transplant physicians, coordinators, regulators and authorities with representatives of other countries and the EU, enabling rapid dissemination and implementation of good clinical practice. This clustering approach could group countries with specific characteristics, for example, those needing to increase living donation compared with rates of deceased donation, or those where expanded donation criteria or donation overall could be enhanced.
Benchmarking
The optimization of transplantation programmes necessitates continuous assessment with external audits and comparison of their efficiency with peer programmes 130 . A uniform registration process and quality control system for organ donation and transplantation throughout Europe is necessary to enable this benchmarking. Transparency of hospitals in reporting their performance for access to and outcomes of transplantation is essential 112 . It is imperative that pan-European transplant registries are established for each organ, to enable benchmarking and ensure that comparable results are achieved across the EU. These comparisons would inform the specific areas for development and address local factors to ensure equitable access to transplantation and to optimize outcomes across Europe. Initiatives that enable comparisons of organ donation and transplantation rates between countries, similar to that developed by the Council of Europe Committee on Organ Transplantation, can help to stimulate countries that are seeking to achieve best practices 131 . Studying the approaches of the best performers will identify a number of critical factors for success, which can then be implemented elsewhere 132 .
Specific frameworks that promote and guide appropriate evidence-based decision making in the context of transplantation should be facilitated and supported. Recommendations might include but should not be limited to criteria for acceptance of patients on the waiting list; adequate follow-up post-transplantation; criteria for DCD transplantation; standards for transplant centres to achieve a well-functioning programme supported by adequate infrastructure; and optimal conditions for donor organ recovery. The application of European recommendations should be based on a continuously audited pan-European platform but allow adaptations according to the situation of individual countries. In Spain, benchmarking of different elements of the transplantation process is one of the cornerstones of its success 39 .
Despite substantial national and trans-national progress over the past five decades, several fundamental questions in the field of transplantation remain unsolved. These range from the basic patho-physiology, immunology and molecular biology of the transplantation process and the response of the host to the donor organ, to clinical aspects and those relating to organizational, societal, psychological and quality of life issues. Transplantation research deserves specific attention for funding and support. Patients, medical professionals and society as a whole will benefit from research streamlined to focus on a number of areas and topics of prime interest (Box 2 ), with the aim of better shaping future priorities, developments and policy actions in the field.
Box 2 Suggested research topics
Approaches to improving organ quality and assessment, and increasing organ availability
Studies on novel preservation methods and new technologies for testing organ quality
Establishing pan-European registries that include follow-up data
Exploring alternative sources of organs (hybrids, xenotransplantation)
Studies of factors that affect outcomes of expanded donation criteria and donation after circulatory death
Comparison of strategies for increasing donor availability
Identification and prevention of factors leading to delayed graft function
Studies on non-HLA incompatibility
Development of strategies to combat acute and chronic rejection
Development and assessment of methods to improve transplantation rates in children, elderly individuals and highly sensitized patients
Studies of barriers to transplantation and measures to correct those; comparisons between countries
Socio-economic and societal impact of transplantation
Health-economic comparison of transplantation programmes in different EU countries
Identification of approaches to decrease the societal cost of transplantation
Studies of the ecological footprint of kidney transplantation compared with dialysis
Studies of factors preventing reemployment after transplantation
Extending the life of the transplant and reducing graft loss
Defining surrogate end points for post-transplantation outcomes
Identification of biomarkers of acute and chronic rejection, graft failure and negative outcomes at large
Detection of mechanisms causing graft dysfunction via development of fibrosis and ways of preventing this evolution
Prevention of post-transplantation malignancy and cardiovascular disease
Prevention and adequate treatment of infections after transplantation
Strategies to improve outcomes for patients with a failing kidney transplant who are transitioning to dialysis
Benchmarking, professionalism and governance
Comparisons of different types of machine perfusion related to different organs for preservation, especially donation after circulatory death
Certification of skills of professionals and professional regulation
Benchmarking of transplantation outcomes (based on registry data)
Study of barriers to transplantation in different countries
Patient priorities
Studies on patient-reported outcomes
Studies of mechanisms that determine treatment choice (transplantation compared with alternatives such as dialysis) and suggestions as to how valid patients can be encouraged to undergo transplantation
Comparative studies of educational programmes (for the general population, patients, students, professionals) and development of best practices
Adapted with permission from ref. 136 , the European Kidney Health Alliance.
International organ exchange
Several EU countries do not have an efficient system to enable the internal offering and sharing of donated organs, nor do they collaborate in wider, usually transnational programmes for deceased donor organ exchange (such as Eurotransplant, Scandiatransplant or the South Alliance for Transplantation). At a minimum, each country should have a national sharing scheme between the local transplant centres whereby an optimal match between donor and recipient and rapid organ removal and transfer to the receiving centre are assured. Furthermore, gradual incorporation into one of the existing international exchange systems should be encouraged as an approach to boost transplantation activity 42 , as exemplified by Croatia in the early 2000s, or more recently by Hungary 133 . Such programmes enable expansion of the donor pool and provide a transparent, equitable and defensible method with which to match the most appropriate donor–recipient pairs as rapidly as possible and thereby improve donor outcomes. In Switzerland, which in essence operates an individual national procurement and offering system (Swisstransplant), close to 6% of the heart transplants and 3% of the lung transplants originate from cross-border organ sharing 134 .
In 2012 the FOEDUS-EOEO platform was launched. FOEDUS-EOEO is an IT-based system that allows European countries to connect with allocation offices ensuring that the organs that cannot be matched within the national or collaborative supra-national systems are available internationally. This type of broad international collaboration is especially beneficial for children and adolescents 11 but also for other vulnerable recipients within a small donor pool (for example, highly sensitized patients).
Conclusions
Despite a good overall track record in the field of transplantation, disparities in transplantation rates between EU countries suggest that there remains ample room for improvement. The Action Plan launched by the EU in 2009 increased organ donation and transplantation and was in place until 2015, but further action is now needed to boost activity. Given the substantial differences between countries in transplantation practices (for example, in the overall transplantation rate, ratio of deceased compared with living donation, application of expanded donation and transplantation of specific organs), an in-depth analysis of discrepancies in transplantation rates is required to inform future improvements across the EU. Optimization and coordination of the donation process is indispensable for a successful transplantation programme. Education of patients, professionals and the general population as well as the provision of appropriate legal and financial frameworks is also necessary. This Roadmap, formulated from a thematic network of European organizations, gives a number of recommendations 3 that provide a framework for further action with which to better cope with the growing transplant waiting lists, reduce the number of patients dying on waiting lists, improve equality in access to transplantation, and improve the outcomes of transplanted organs, inside, as well as outside, the EU.
In this Roadmap, we assume that the primary element needed to increase the number of patients with a functioning graft is increased organ donation, which requires investment in processes to coordinate the donation process, approaches to encouraging living donation and consideration of expanded donation criteria. However, donation cannot be enhanced without a parallel investment in infrastructure, the implementation of approaches to overcoming financial barriers, and educational efforts. The remaining factors, such as the need for benchmarking, registration, research and efforts to abolish inequities, might not directly affect the total number of transplants, but their consideration remains essential for ethical reasons and because they support the other strategies. The Joint Statement on which this Roadmap is based 3 outlines a number of key areas along which policy makers could streamline such a plan (Supplementary Box 6 ). The development of such a plan should aim to stimulate increases in transplantation rates similar to those achieved following implementation of the original EU Action Plan on Organ Donation and Transplantation (2009–2015), and should involve yearly assessments and adjustments per country or group of countries, with successful countries serving as examples for the others.
Vanholder, R. et al. Reducing the costs of chronic kidney disease while delivering quality health care: a call to action. Nat. Rev. Nephrol. 13 , 393–409 (2017).
Article PubMed Google Scholar
Vanholder, R. et al. How to increase kidney transplant activity throughout Europe — an advocacy review by the European Kidney Health Alliance. Nephrol. Dial. Transplant. 34 , 1254–1261 (2019).
European Kidney Health Alliance. Joint Statement. Thematic Network on Improving Organ Donation and Transplantation in the EU 2019 http://ekha.eu/wp-content/uploads/FINAL_Joint-Statement-of-the-Thematic-Network-on-Organ-Donation-and-Transplantation.pdf (2019).
World Health Organization. Noncommunicable diseases. WHO http://www.euro.who.int/en/health-topics/noncommunicable-diseases/noncommunicable-diseases (2017).
NCD Countdown Collaborators. NCD Countdown 2030: worldwide trends in non-communicable disease mortality and progress towards Sustainable Development Goal target 3.4. Lancet 392 , 1072–1088 (2018).
Article Google Scholar
Delmonico, F. L., Dominguez-Gil, B., Matesanz, R. & Noel, L. A call for government accountability to achieve national self-sufficiency in organ donation and transplantation. Lancet 378 , 1414–1418 (2011).
WHO, Transplantation Society, Organization Nacional de Transplantes. Third WHO Global Consultation on Organ Donation and Transplantation: striving to achieve self-sufficiency, March 23-25, 2010, Madrid, Spain. Transplantation 91 (Suppl. 11), S27–S28 (2011).
Google Scholar
Dominguez-Gil, B. International figures on donation and transplantation 2019. Newsletter Transplant. European Parliament https://www.europarl.europa.eu/EPRS/Newsletter_Transplant_2019.pdf (2020).
Haase, B. et al. Ethical, legal, and societal issues and recommendations for controlled and uncontrolled DCD. Transpl. Int. 29 , 771–779 (2016).
Lomero, M. et al. Donation after circulatory death today: an updated overview of the European landscape. Transpl. Int. 33 , 76–88 (2020).
Bouwman, R. et al. Study on the uptake and impact of the EU Action Plan on Organ Donation and Transplantation (2009-2015) in the EU Member States. European Commission https://ec.europa.eu/health/sites/health/files/blood_tissues_organs/docs/2017_euactionplan_2009-2015_impact_exe_en.pdf (2017).
Zoccali, C., Kramer, A. & Jager, K. The databases: renal replacement therapy since 1989 — the European Renal Association and European Dialysis and Transplant Association (ERA-EDTA). Clin. J. Am. Soc. Nephrol. 4 (Suppl. 1), 18–22 (2009).
No Authors Listed. Organ Transplant Scandal Shocks Germany. Spiegel http://www.spiegel.de/international/germany/organ-transplant-scandal-shocks-germany-a-848016.html (2012).
Foreman, K. J. et al. Forecasting life expectancy, years of life lost, and all-cause and cause-specific mortality for 250 causes of death: reference and alternative scenarios for 2016-40 for 195 countries and territories. Lancet. 392 , 2052–2090 (2018).
Article PubMed PubMed Central Google Scholar
Tonelli, M. et al. Systematic review: kidney transplantation compared with dialysis in clinically relevant outcomes. Am. J. Transplant. 11 , 2093–2109 (2011).
Article CAS PubMed Google Scholar
Haller, M. C., Kainz, A., Baer, H. & Oberbauer, R. Dialysis vintage and outcomes after kidney transplantation: a retrospective cohort study. Clin. J. Am. Soc. Nephrol. 12 , 122–130 (2017).
Wong, G. et al. Comparative survival and economic benefits of deceased donor kidney transplantation and dialysis in people with varying ages and co-morbidities. PLoS ONE 7 , e29591 (2012).
Article CAS PubMed PubMed Central Google Scholar
European Renal Association – European Dialysis and Transplant Association. ERA-EDTA Registry: ERA-EDTA Registry Annual Report 2017. ERA-EDTA https://era-edta-reg.org/files/annualreports/AnnRep2017.pdf (2017).
Cassuto, J. R. et al. Wait list death and survival benefit of kidney transplantation among nonrenal transplant recipients. Am. J. Transplant. 10 , 2502–2511 (2010).
Haller, M., Gutjahr, G., Kramar, R., Harnoncourt, F. & Oberbauer, R. Cost-effectiveness analysis of renal replacement therapy in Austria. Nephrol. Dial. Transplant. 26 , 2988–2995 (2011).
Mohnen, S. M. et al. Healthcare costs of patients on different renal replacement modalities - Analysis of Dutch health insurance claims data. PLoS ONE 14 , e0220800 (2019).
Bhutiani, N. et al. A cost analysis of early biliary strictures following orthotopic liver transplantation in the United States. Clin. Transplant. 32 , e13396 (2018).
Dageforde, L. A., Feurer, I. D., Pinson, C. W. & Moore, D. E. Is liver transplantation using organs donated after cardiac death cost-effective or does it decrease waitlist death by increasing recipient death? HPB 15 , 182–189 (2013).
Williams, R. et al. Disease burden and costs from excess alcohol consumption, obesity, and viral hepatitis: fourth report of the Lancet Standing Commission on Liver Disease in the UK. Lancet 391 , 1097–1107 (2018).
Long, E. F., Swain, G. W. & Mangi, A. A. Comparative survival and cost-effectiveness of advanced therapies for end-stage heart failure. Circ. Heart Fail. 7 , 470–478 (2014).
Ye, X. T., Parker, A., Brink, J., Weintraub, R. G. & Konstantinov, I. E. Cost-effectiveness of the National Pediatric Heart Transplantation Program in Australia. J. Thorac. Cardiovasc. Surg. 157 , 1158–1166 (2018).
OECD & European Union. Health at a Glance: Europe 2016 – State of Health in the EU Cycle. OECD iLibrary https://doi.org/10.1787/9789264265592-en (2016).
Danuser, B. et al. Employment 12 months after kidney transplantation: An in-depth bio-psycho-social analysis of the Swiss Transplant Cohort. PLoS ONE 12 , e0175161 (2017).
Article PubMed PubMed Central CAS Google Scholar
Dukic, M. Z. & Zibar, L. Employment in patients with renal replacement therapy. SEEMED J. 3 , 11–20 (2019).
Julian Mauro, J. C., Molinuevo Tobalina, J. A. & Sanchez Gonzalez, J. C. Employment in the patient with chronic kidney disease related to renal replacement therapy. Nefrologia. 32 , 439–445 (2012).
PubMed Google Scholar
Liem, Y. S., Bosch, J. L. & Hunink, M. G. Preference-based quality of life of patients on renal replacement therapy: a systematic review and meta-analysis. Value Health 11 , 733–741 (2008).
Manificat, S. et al. Quality of life of children and adolescents after kidney or liver transplantation: child, parents and caregiver’s point of view. Pediatr. Transplant. 7 , 228–235 (2003).
Commission of the European Communities. Action plan on Organ Donation and Transplantation (2009-2015): Strengthened Cooperation between Member. States. European Commission https://ec.europa.eu/health/ph_threats/human_substance/oc_organs/docs/organs_action_en.pdf (2008).
Wu, D. A. et al. Barriers to living donor kidney transplantation in the United Kingdom: a national observational study. Nephrol. Dial. Transplant. 32 , 890–900 (2017).
Council of Europe. Legal Framework. https://www.edqm.eu/en/legal-framework (2021).
No Authors Listed. The Madrid resolution on organ donation and transplantation: national responsibility in meeting the needs of patients, guided by the WHO principles. Transplantation 91 (Suppl. 11), S29–S31 (2011).
Hanson, C. S. et al. Nephrologists’ perspectives on recipient eligibility and access to living kidney donor transplant. Transplantation 100 , 943–953 (2016).
de Jong, R. W. et al. Non-medical barriers reported by nephrologists when providing renal replacement therapy or comprehensive conservative management to end-stage kidney disease patients: a systematic review. Nephrol. Dial. Transplant. https://doi.org/10.1093/ndt/gfz271 (2020).
Matesanz, R., Dominguez-Gil, B., Coll, E., de la Rosa, G. & Marazuela, R. Spanish experience as a leading country: what kind of measures were taken? Transplant. Int. 24 , 333–343 (2011).
Matesanz, R., Marazuela, R., Coll, E., Mahillo, B. & Dominguez-Gil, B. About the opt-out system, live transplantation, and information to the public on organ donation in Spain… Y ole! Am. J. Transpl. 17 , 1695–1696 (2017).
Dominguez-Gil, B. End-of-life practices in patients with devastating brain injury in Spain: implications for organ donation. Med. Intensiva 41 , 162–173 (2017).
Zivcic-Cosic, S. et al. Development of the Croatian model of organ donation and transplantation. Croat. Med. J. 54 , 65–70 (2013).
European Kidney Health Alliance. European Kidney Forum 2019 “Organ Donation and Transplantation in Europe – Are We Meeting the Needs of Patients?”. EKHA http://ekha.eu/blog/european-kidney-forum-2019-organ-donation-and-transplantation-in-europe-are-we-meeting-the-needs-of-patients/ (2019).
Sautenet, B. et al. Developing consensus-based priority outcome domains for trials in kidney transplantation: a multinational Delphi survey with patients, caregivers, and health professionals. Transplantation 101 , 1875–1886 (2017).
Dominguez-Gil, B., Murphy, P. & Procaccio, F. Ten changes that could improve organ donation in the intensive care unit. Intensive Care Med. 42 , 264–267 (2016).
Martin-Delgado, M. C. et al. Summary of Spanish recommendations on intensive care to facilitate organ donation. Am. J. Transplant. 19 , 1782–1791 (2019).
Shrestha, S. et al. Logistical factors influencing cold ischemia times in deceased donor kidney transplants. Transplantation 100 , 422–428 (2016).
Miller, C. & Breakwell, R. What factors influence a family’s decision to agree to organ donation? A critical literature review. London J. Prim. Care 10 , 103–107 (2018).
Dominguez-Gil, B. et al. The critical pathway for deceased donation: reportable uniformity in the approach to deceased donation. Transplant. Int. 24 , 373–378 (2011).
Traynor, C. et al. Twenty-year survivors of kidney transplantation. Am. J. Transplant. 12 , 3289–3295 (2012).
Reichman, T. W. et al. Living donor versus deceased donor liver transplantation: a surgeon-matched comparison of recipient morbidity and outcomes. Transpl. Int. 26 , 780–787 (2013).
Mandelbrot, D. A. & Pavlakis, M. Living donor practices in the United States. Adv. Chron. Kidney Dis. 19 , 212–219 (2012).
Holscher, C. M. et al. Self-reported incident hypertension and long-term kidney function in living kidney donors compared with healthy nondonors. Clin. J. Am. Soc. Nephrol. 14 , 1493–1499 (2019).
Kestenbaum, B. R. & Seliger, S. L. Commentary on risks of living kidney donation: current state of knowledge on core outcomes important to donors. Clin. J. Am. Soc. Nephrol. 14 , 609–610 (2019).
Lennerling, A. et al. Living organ donation practices in Europe — results from an online survey. Transpl. Int. 26 , 145–153 (2013).
Lentine, K. L., Lam, N. N. & Segev, D. L. Risks of living kidney donation: current state of knowledge on outcomes important to donors. Clin. J. Am. Soc. Nephrol. 14 , 597–608 (2019).
Ferrari, P., Weimar, W., Johnson, R. J., Lim, W. H. & Tinckam, K. J. Kidney paired donation: principles, protocols and programs. Nephrol. Dial. Transplant. 30 , 1276–1285 (2015).
Biro, P. et al. Building kidney exchange programmes in europe-an overview of exchange practice and activities. Transplantation 103 , 1514–1522 (2019).
Valentin, M. O. et al. International cooperation for kidney exchange success. Transplantation 103 , e180–e181 (2019).
Bohmig, G. A. et al. Czech-Austrian kidney paired donation: first European cross-border living donor kidney exchange. Transplant. Int. 30 , 638–639 (2017).
Working Group on Living Donation. Toolbox Living Kidney Donation. European Commission https://ec.europa.eu/health/sites/health/files/blood_tissues_organs/docs/eutoolbox_living_kidney_donation_en.pdf (2016).
Truog, R. D. The ethics of organ donation by living donors. N. Engl. J. Med. 353 , 444–446 (2005).
Port, F. K. et al. Donor characteristics associated with reduced graft survival: an approach to expanding the pool of kidney donors. Transplantation 74 , 1281–1286 (2002).
Watson, C. J., Johnson, R. J., Birch, R., Collett, D. & Bradley, J. A. A simplified donor risk index for predicting outcome after deceased donor kidney transplantation. Transplantation 93 , 314–318 (2012).
Collett, D., Friend, P. J. & Watson, C. J. Factors associated with short- and long-term liver graft survival in the United Kingdom: development of a UK donor liver index. Transplantation 101 , 786–792 (2017).
Dahmen, M. et al. Validation of the Kidney Donor Profile Index (KDPI) to assess a deceased donor’s kidneys’ outcome in a European cohort. Sci. Rep. 9 , 11234 (2019).
Cohen, J. B. et al. Survival benefit of transplantation with a deceased diabetic donot kidney compared with remaining on the waitlist. Clin. J. Am. Soc. Nephrol. 12 , 974–982 (2017).
Ibrahim, M. et al. Utilization and outcomes of single and dual kidney transplants from older deceased donors in the United Kingdom. Clin. J. Am. Soc. Nephrol. 15 , 1320–1329 (2020).
Schaapherder, A. et al. Equivalent long-term transplantation outcomes for kidneys donated after brain death and cardiac death: conclusions from a nationwide evaluation. EClinicalMedicine 4 , 25–31 (2018).
Summers, D. M. et al. Analysis of factors that affect outcome after transplantation of kidneys donated after cardiac death in the UK: a cohort study. Lancet 376 , 1303–1311 (2010).
Smith, M., Dominguez-Gil, B., Greer, D. M., Manara, A. R. & Souter, M. J. Organ donation after circulatory death: current status and future potential. Intensive Care Med. 45 , 310–321 (2019).
Minambres, E., Rubio, J. J., Coll, E. & Dominguez-Gil, B. Donation after circulatory death and its expansion in Spain. Curr. Opin. Organ. Transplant. 23 , 120–129 (2018).
Trapero-Marugan, M., Little, E. C. & Berenguer, M. Stretching the boundaries for liver transplant in the 21st century. Lancet Gastroenterol. Hepatol. 3 , 803–811 (2018).
No Authors Listed. NEW release: 7th edition Guide to the quality and safety of Organs for transplantation. Council of Europe https://www.edqm.eu/en/news/new-release-7th-edition-guide-quality-and-safety-organs-transplantation (2018).
Kumar, R. N. & Stosor, V. Organ transplantation in persons with HIV. AIDS 34 , 1107–1116 (2020).
Potluri, V. S. et al. National trends in utilization and 1-year outcomes with transplantation of HCV-viremic kidneys. J. Am. Soc. Nephrol. 30 , 1939–1951 (2019).
Givertz, M. M., Woolley, A. E. & Baden, L. R. Expanding the donor pool with use of hepatitis C infected hearts. Circ. Heart Fail. 11 , e005656 (2018).
Ysebaert, D. et al. Organ procurement after euthanasia: Belgian experience. Transplant. Proc. 41 , 585–586 (2009).
Wilkinson, D. & Savulescu, J. Should we allow organ donation euthanasia? Alternatives for maximizing the number and quality of organs for transplantation. Bioethics 26 , 32–48 (2012).
Bouwman, R., Wiegers, T., van Schoten, S., Coppen, R. & Friele, R. Study on the uptake and impact of the EU Action Plan on Organ Donation and Transplantation (2009-2015) in the EU Member States. European Commission https://ec.europa.eu/health/sites/health/files/blood_tissues_organs/docs/2017_euactionplan_2009-2015_impact_exe_en.pdf (2017).
Dominguez-Gil, B. et al. Current situation of donation after circulatory death in European countries. Transplant. Int. 24 , 676–686 (2011).
Mohan, S. et al. Factors leading to the discard of deceased donor kidneys in the United States. Kidney Int. 94 , 187–198 (2018).
Stallone, G. & Grandaliano, G. To discard or not to discard: transplantation and the art of scoring. Clin. Kidney J. 12 , 564–568 (2019).
Manara, A., Procaccio, F. & Dominguez-Gil, B. Expanding the pool of deceased organ donors: the ICU and beyond. Intensive Care Med. 45 , 357–360 (2019).
Scandroglio, B. et al. Analysis of the attitudes and motivations of the Spanish population towards organ donation after death. Transpl. Int. 24 , 158–166 (2011).
Byrne, M. et al. School education to increase organ donation and awareness of issues in transplantation in the UK. Pediatr. Transplant. 23 , e13492 (2019).
Febrero, B. et al. Knowledge of the brain death concept among older people. Transplant. Proc. 52 , 506–508 (2020).
No Authors Listed. Gift of Life. European Kidney Health Alliance http://ekha.eu/gift-of-life/ (2018).
Zhang, X. et al. Racial/ethnic disparities in waitlisting for deceased donor kidney transplantation 1 year after implementation of the new national kidney allocation system. Am. J. Transplant. 18 , 1936–1946 (2018).
Garg, A. X. Helping more patients receive a living donor kidney transplant. Clin. J. Am. Soc. Nephrol. 13 , 1918–1923 (2018).
Hoogeveen, E. K. et al. Effect of obesity on the outcome of kidney transplantation: a 20-year follow-up. Transplantation 91 , 869–874 (2011).
Oste, M. C. et al. Mediterranean style diet is associated with low risk of new-onset diabetes after renal transplantation. BMJ Open Diabetes Res. Care 5 , e000283 (2017).
Van Biesen, W., van der Veer, S. N., Murphey, M., Loblova, O. & Davies, S. Patients’ perceptions of information and education for renal replacement therapy: an independent survey by the European Kidney Patients’ Federation on information and support on renal replacement therapy. PLoS ONE 9 , e103914 (2014).
Norris, K. & Nissenson, A. R. Race, gender, and socioeconomic disparities in CKD in the United States. J. Am. Soc. Nephrol. 19 , 1261–1270 (2008).
Poulakou, G., Len, O. & Akova, M. Immigrants as donors and transplant recipients: specific considerations. Intensive Care Med. 45 , 401–403 (2019).
Ikram, U. Z., Kunst, A. E., Lamkaddem, M. & Stronks, K. The disease burden across different ethnic groups in Amsterdam, the Netherlands, 2011–2030. Eur. J. Publ. Health 24 , 600–605 (2013).
Zhang, Y., Gerdtham, U. G., Rydell, H. & Jarl, J. Socioeconomic inequalities in the kidney transplantation process: a registry-based study in Sweden. Transplant. Direct 4 , e346 (2018).
Department of Health. Organs for Transplants A report from the Organ Donation Taskforce. NHS https://nhsbtdbe.blob.core.windows.net/umbraco-assets-corp/4245/organsfortransplantstheorgandonortaskforce1streport.pdf .
Tiessen, J. et al. Improving Organ Donation and Transplantation in the European Union. Assessing the Impacts of European Action. Rand Europe https://www.rand.org/content/dam/rand/pubs/technical_reports/2008/RAND_TR602.pdf (2008).
Bratton, C., Chavin, K. & Baliga, P. Racial disparities in organ donation and why. Curr. Opin. Organ. Transpl. 16 , 243–249 (2011).
Valentin, M. O. et al. Implementation of a national priority allocation system for hypersensitized patients in spain, based on virtual crossmatch: initial results. Transplant. Proc. 48 , 2871–2875 (2016).
Puoti, F. et al. Organ transplantation and gender differences: a paradigmatic example of intertwining between biological and sociocultural determinants. Biol. Sex. Differ. 7 , 35 (2016).
Antlanger, M. et al. Sex differences in kidney replacement therapy initiation and maintenance. Clin. J. Am. Soc. Nephrol. 14 , 1616–1625 (2019).
Carrero, J. J., Hecking, M., Chesnaye, N. C. & Jager, K. J. Sex and gender disparities in the epidemiology and outcomes of chronic kidney disease. Nat. Rev. Nephrol. 14 , 151–164 (2018).
Melk, A. et al. Equally interchangeable? How sex and gender affect transplant. Transplantation 103 , 1094–1110 (2019).
Shepherd, L., O’Carroll, R. E. & Ferguson, E. An international comparison of deceased and living organ donation/transplant rates in opt-in and opt-out systems: a panel study. BMC Med. 12 , 131 (2014).
Abadie, A. & Gay, S. The impact of presumed consent legislation on cadaveric organ donation: a cross-country study. J. Health Econ. 25 , 599–620 (2006).
Arshad, A., Anderson, B. & Sharif, A. Comparison of organ donation and transplantation rates between opt-out and opt-in systems. Kidney Int. 95 , 1453–1460 (2019).
Matesanz, R. & Dominguez-Gil, B. Opt-out legislations: the mysterious viability of the false. Kidney Int. 95 , 1301–1303 (2019).
Howard, K. et al. Preferences for policy options for deceased organ donation for transplantation: a discrete choice experiment. Transplantation 100 , 1136–1148 (2016).
Gander, J. C. et al. Association between dialysis facility ownership and access to kidney transplantation. JAMA 322 , 957–973 (2019).
Boulware, L. E., Wang, V. & Powe, N. R. Improving access to kidney transplantation: business as usual or new ways of doing business? JAMA 322 , 931–933 (2019).
Heemann, U., Abramowicz, D., Spasovski, G., Vanholder, R. & European Renal Best Practice Work Group on Kidney Transplantation. Endorsement of the kidney disease improving global outcomes (KDIGO) guidelines on kidney transplantation: a European Renal Best Practice (ERBP) position statement. Nephrol. Dial. Transplant. 26 , 2099–2106 (2011).
Pippias, M. et al. The European Renal Association — European Dialysis and Transplant Association Registry Annual Report 2014: a summary. Clin. Kidney J. 10 , 154–169 (2017).
PubMed PubMed Central Google Scholar
Khush, K. K. et al. The International Thoracic Organ Transplant Registry of the International Society for Heart and Lung Transplantation: thirty-fifth adult heart transplantation report-2018; focus theme: multiorgan transplantation. J. Heart Lung Transplant. 37 , 1155–1168 (2018).
Coemans, M. et al. Analyses of the short- and long-term graft survival after kidney transplantation in Europe between 1986 and 2015. Kidney Int. 94 , 964–973 (2018).
Schroppel, B. & Legendre, C. Delayed kidney graft function: from mechanism to translation. Kidney Int. 86 , 251–258 (2014).
Perico, N., Cattaneo, D., Sayegh, M. H. & Remuzzi, G. Delayed graft function in kidney transplantation. Lancet 364 , 1814–1827 (2004).
Debout, A. et al. Each additional hour of cold ischemia time significantly increases the risk of graft failure and mortality following renal transplantation. Kidney Int. 87 , 343–349 (2015).
Breyer, M. D. & Susztak, K. The next generation of therapeutics for chronic kidney disease. Nat. Rev. Drug Discov. 15 , 568–588 (2016).
Gill, J. S., Rose, C., Pereira, B. J. & Tonelli, M. The importance of transitions between dialysis and transplantation in the care of end-stage renal disease patients. Kidney Int. 71 , 442–447 (2007).
Prendergast, M. B. & Gaston, R. S. Optimizing medication adherence: an ongoing opportunity to improve outcomes after kidney transplantation. Clin. J. Am. Soc. 5 , 1305–1311 (2010).
Dobbels, F., Van Damme-Lombaert, R., Vanhaecke, J. & De Geest, S. Growing pains: non-adherence with the immunosuppressive regimen in adolescent transplant recipients. Pediatr. Transplant. 9 , 381–390 (2005).
Russell, C. L. et al. Improving medication adherence and outcomes in adult kidney transplant patients using a personal systems approach: SystemCHANGE results of the MAGIC randomized clinical trial. Am. J. Transplant. 20 , 125–136 (2020).
Kuypers, D. R. Immunosuppressive drug monitoring — what to use in clinical practice today to improve renal graft outcome. Transpl. Int. 18 , 140–150 (2005).
Wieland, E. et al. Biomarkers as a tool for management of immunosuppression in transplant patients. Ther. Drug Monit. 32 , 560–572 (2010).
Bell, L. E. et al. Adolescent transition to adult care in solid organ transplantation: a consensus conference report. Am. J. Transplant. 8 , 2230–2242 (2008).
Meier-Kriesche, H. U., Schold, J. D., Gaston, R. S., Wadstrom, J. & Kaplan, B. Kidneys from deceased donors: maximizing the value of a scarce resource. Am. J. Transplant. 5 , 1725–1730 (2005).
Huang, E. & Jordan, S. C. Clinical and public policy implications of pre-formed DSA and transplant outcomes. Clin. J. Am. Soc. Nephrol. 14 , 972–974 (2019).
de la Rosa, G. et al. Continuously evaluating performance in deceased donation: the Spanish quality assurance program. Am. J. Transplant. 12 , 2507–2513 (2012).
Weiss, J. et al. Evolution of deceased organ donation activity versus efficiency over a 15-year period: an international comparison. Transplantation 102 , 1768–1778 (2018).
Matesanz, R. et al. Benchmarking in the process of donation after brain death: a methodology to identify best performer hospitals. Am. J. Transplant. 12 , 2498–2506 (2012).
No Authors Listed. Eurotransplant region. Eurotransplant https://www.eurotransplant.org/about-eurotransplant/region/ (2021).
Schneider, S., Schreiner, P., Weiss, J. & Immer, F. F. Assessing the potential of international organ exchange–the Swiss experience. Eur. J. Cardiothorac. Surg. 40 , 1368–1373 (2011).
Organizacion Nacional De Trasplantes. Publicaciones ONT http://www.ont.es/publicaciones/Paginas/Publicaciones.aspx (2021).
European Kidney Health Alliance. Thematic Network on Improving Organ Donation and Transplantation in the EU 2019. EKHA http://ekha.eu/wp-content/uploads/FINAL_14.01.2020_Joint-Statement-of-the-Thematic-Network-on-Organ-Donation-and-Transplantation.pdf (2020).
Download references
Acknowledgements
Each year the European Union commissions a number of Joint Statements regarding health issues, which bring together several stakeholder groups to make recommendations to the European Commission for the coming years. The coordination of the joint statement informing the present Roadmap was allocated to the European Kidney Health Alliance (EKHA). The EKHA represents a common effort by all European key stakeholders in kidney care (patients, nurses, physicians, foundations) to propose solutions for the challenges of kidney disease in Europe through the development of effective prevention and more efficient care pathways. In addition to the EKHA, the organizations involved in this publication and the European Commission Joint Statement are either pan-European Organizations with a focus on transplantation or transplantable organs or the National Transplant Organizations of Croatia and Spain. Specifically, these organizations are the European Society of Organ Transplantation (ESOT); the European Renal Association–European Dialysis and Transplant Association (ERA–EDTA); the ERA-EDTA Registry; United European Gastroenterology (UEG); the European Association for the Study of the Liver (EASL) and the National Competent Authorities for Organ Donation and Transplantation of Croatia and Spain. The Joint Statement was endorsed by 54 Organizations and Institutions and by 19 Members of the European Parliament. The authors are indebted to Marine Faure and Sophie Bruno (Senior Consultants, Interel European Affairs) and Nazli Gül (Consultant, Interel European Affairs) for their assistance in the preparation of the Joint Statement that is the basis for this publication.
Author information
Authors and affiliations.
Department of Internal Medicine and Paediatrics, Ghent University Hospital, Ghent, Belgium
Raymond Vanholder
European Kidney Health Alliance (EKHA), Brussels, Belgium
Organización Nacional de Trasplantes (ONT), Madrid, Spain
Beatriz Domínguez-Gil, Beatriz Mahillo & Maria O. Valentin
Ministry of Health, Zagreb, Croatia
Mirela Busic
Clínica Universitária de Gastrenterologia, Faculdade de Medicina, Universidade de Lisboa, Lisboa, Portugal
Helena Cortez-Pinto
United European Gastroenterology (UEG), Vienna, Austria
European Association for the Study of the Liver (EASL), Geneva, Switzerland
College of Medicine and Public Health, Flinders University, Adelaide, Australia
Jonathan C. Craig
ERA-EDTA Registry, Department of Medical Informatics, Amsterdam Public Health Research Institute, Amsterdam UMC, University of Amsterdam, Amsterdam, The Netherlands
Kitty J. Jager & Vianda S. Stel
Associazione Ipertensione Nefrologia e Trapianto Renale (IPNET), Reggio di Calabria, Italy
Carmine Zoccali
European Renal Association – European Dialysis and Transplant Association (ERA-EDTA), London, UK
Edinburgh Transplant Centre, Royal Infirmary of Edinburgh & University of Edinburgh, Edinburgh, UK
Gabriel C. Oniscu
European Society of Organ Transplantation (ESOT), Amsterdam, the Netherlands
You can also search for this author in PubMed Google Scholar
Contributions
R.V. contributed to conceptualizing and designing the Roadmap, data analyses, the literature search and writing of the manuscript. B.D.-G. contributed to designing the Roadmap, performing the literature search, data collection and writing. G.C.O. contributed to designing the Roadmap, performing the literature search, writing and editing the manuscript before submission. M.B., H.C.-P. and J.C.C. contributed to writing of the manuscript. K.J.J. contributed to writing and data collection. B.M. contributed to data collection. V.S.S. and M.O.V. contributed to the literature search, writing and data collection.
Corresponding author
Correspondence to Raymond Vanholder .
Ethics declarations
Competing interests.
R.V. reports unrestricted grants to the European Kidney Health Alliance from Baxter Health Care, Astellas, Amgen, BBraun, CSL Behring, Hansa BioPharma and Viforpharma, for the organization of the annual EKHA Kidney Forum at the European Parliament. H.C.-P. reports personal fees from Intercept, Gilead, Promethera and Genfit, outside of the submitted work. K.J.J. reports grants from ERA-EDTA during the conduct of the study, and personal fees from Fresenius Medical Care, outside of the submitted work. The other authors declare no conflicts of interest.
Additional information
Peer review information.
Nature Reviews Nephrology thanks L. Hilbrands, who co-reviewed with M. Baas, A. Rahmel, and the other, anonymous, reviewer(s) for their contribution to the peer review of this work.
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Related links
European Kidney Health Alliance: http://ekha.eu/
FOEDUS-EOEO: https://www.foedus-eoeo.eu/#/public
Supplementary information
Supplementary information.
(EKHA). A non-governmental advocacy organization promoting the cause of kidney patients at the level of the European Union and the European Union member states.
A situation in which a kidney transplant candidate receives a donor kidney before starting on dialysis.
Programmes that enable sharing of organs between donor–recipient pairs who cannot exchange a donor organ directly with each other.
A category of patients on the transplant waitlist who are temporarily ineligible for transplantation because of medical, social or personal reasons.
Rights and permissions
Reprints and permissions
About this article
Cite this article.
Vanholder, R., Domínguez-Gil, B., Busic, M. et al. Organ donation and transplantation: a multi-stakeholder call to action. Nat Rev Nephrol 17 , 554–568 (2021). https://doi.org/10.1038/s41581-021-00425-3
Download citation
Accepted : 25 March 2021
Published : 05 May 2021
Issue Date : August 2021
DOI : https://doi.org/10.1038/s41581-021-00425-3
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
This article is cited by
Research progress and prospects of benefit-risk assessment methods for umbilical cord mesenchymal stem cell transplantation in the clinical treatment of spinal cord injury.
Stem Cell Research & Therapy (2024)
Organ trafficking — a continuing challenge
- Thomas F. Mueller
- Sanjay Nagral
Nature Reviews Nephrology (2024)
Heart transplantation: advances in expanding the donor pool and xenotransplantation
- Stephanie Jou
- Sean R. Mendez
- Claudia Gidea
Nature Reviews Cardiology (2024)
Development and outcomes of surgical and urological kidney transplantation programs in Germany: a total population analysis from 2006 to 2021
- Philipp Reimold
- Luka Flegar
World Journal of Urology (2024)
Automating iPSC generation to enable autologous photoreceptor cell replacement therapy
- Laura R. Bohrer
- Nicholas E. Stone
- Budd A. Tucker
Journal of Translational Medicine (2023)
Quick links
- Explore articles by subject
- Guide to authors
- Editorial policies
Sign up for the Nature Briefing newsletter — what matters in science, free to your inbox daily.
Review of Ethical Challenges of Organ Transplantation: Current Debates and International Perspectives
Hansen, Solveig Lena, and Silke Schicktanz (eds). 2021. Ethical Challenges of Organ Transplantation: Current Debates and International Perspectives . Bielefeld: Transcript Verlag. ISBN 978-3-8376-4643-6
- Book Review
- Published: 13 February 2024
Cite this article

- Nitzan Rimon-Zarfaty ORCID: orcid.org/0000-0003-2883-9986 1
142 Accesses
Explore all metrics
This is a preview of subscription content, log in via an institution to check access.
Access this article
Subscribe and save.
- Get 10 units per month
- Download Article/Chapter or eBook
- 1 Unit = 1 Article or 1 Chapter
- Cancel anytime
Price includes VAT (Russian Federation)
Instant access to the full article PDF.
Rent this article via DeepDyve
Institutional subscriptions
Haimes, E. 2002. What can the social sciences contribute to the study of ethics? Theoretical, empirical and substantive considerations. Bioethics 16(2): 89–113.
Article PubMed Google Scholar
Hurst, D.J., J. Potter, and L.A. Padilla. 2022. Organ transplant and Covid‐19 vaccination: Considering the ethics of denying transplant to unvaccinated patients. Clinical Transplantation 36(5): e14589.
Article CAS PubMed Google Scholar
Loupy, A., O. Aubert, P.P Reese, O. Bastien, F. Bayer, and C. Jacquelinet. 2020. Organ procurement and transplantation during the COVID-19 pandemic. The Lancet 395(10237): e95–e96.
Article CAS Google Scholar
Moorlock, G., and H. Draper. 2018. Empathy, social media, and directed altruistic living organ donation. Bioethics 32(5): 289–297.
Article PubMed PubMed Central Google Scholar
Download references
No funding was received for this work.
Author information
Authors and affiliations.
Department of Human Resource Management Studies, Sapir Academic College, 7915600, D.N. Hof Ashkelon, Israel
Nitzan Rimon-Zarfaty
You can also search for this author in PubMed Google Scholar
Corresponding author
Correspondence to Nitzan Rimon-Zarfaty .
Ethics declarations
Conflicts of interest/competing interests.
Nitzan Rimon-Zarfaty was affiliated during 2016–2019 at the Department of Medical Ethics and History of Medicine, the University Medical Center Göttingen, and has scientifically collaborated with Silke Schicktanz on a topic in reproductive medicine and ethics.
Additional information
Publisher's note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Reprints and permissions
About this article
Rimon-Zarfaty, N. Review of Ethical Challenges of Organ Transplantation: Current Debates and International Perspectives . Bioethical Inquiry (2024). https://doi.org/10.1007/s11673-023-10330-y
Download citation
Received : 02 August 2022
Accepted : 05 December 2023
Published : 13 February 2024
DOI : https://doi.org/10.1007/s11673-023-10330-y
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Find a journal
- Publish with us
- Track your research
- Search by keyword
- Search by citation
Page 1 of 2
13 C glucose labelling studies using 2D NMR are a useful tool for determining ex vivo whole organ metabolism during hypothermic machine perfusion of kidneys
The aim of this study is to determine the feasibility of using nuclear magnetic resonance (NMR) tracer studies ( 13 C-enriched glucose) to detect ex vivo de novo metabolism in the perfusion fluid and cortical tissu...
- View Full Text
Matched-pair analysis: identification of factors with independent influence on the development of PTLD after kidney or liver transplantation
Post-transplant lymphoproliferative disorder (PTLD) adversely affects patients’ long-term outcome.
From motivation to acceptability: a survey of public attitudes towards organ donation in Denmark
Over the past three decades, public attitudes to organ donation have been a subject of numerous studies focusing on donor motivation. Here, we present a fresh approach. We suggest focusing on public acceptabil...
Protocol for a prospective randomized controlled trial of recipient remote ischaemic preconditioning in orthotopic liver transplantation (RIPCOLT trial)
Ischaemic reperfusion (IR) injury is a major cause of graft loss, morbidity and mortality following orthotopic liver transplantation (OLT). Demand for liver transplantation has resulted in increasing use of ma...
Some considerations on the current debate about typing resolution in solid organ transplantation
The shortage of suitable organs and achieved tolerance are uncontested main concerns in transplantation. Long waiting lists for deceased donors and limited numbers of living donors are the current scenarios. K...
The role of CYP3A5 polymorphism and dose adjustments following conversion of twice-daily to once-daily tacrolimus in renal transplant recipients
Tacrolimus is available as twice-daily Prograf® (Tac-BID) and the once-daily formulation, Advagraf® (Tac-OD). Although therapeutically equivalent, some transplant recipients require dose adjustments to achieve...
Immunomodulating effects of the anti-viral agent Silibinin in liver transplant patients with HCV recurrence
Silibinin has been shown to have anti-HCV activity and immune-modulating properties by regulating dendritic cell (DC) function. DCs are antigen-presenting cells that, together with regulatory T cells (Treg), p...
Practical considerations for the use of mTOR inhibitors
Immunosuppressive therapy after kidney transplantation is based on calcineurin inhibitors (CNI). In most cases CNI therapy is combined with mycophenolate and steroids. In spite of good short-term results this ...
This article is part of a Supplement: Volume 4 Supplement 1
Reviewing 15 years of experience with sirolimus
Here, we review 15 years of clinical use of sirolimus in our transplant center, in context with the developing immunosuppressive strategies use worldwide. The majority of studies were conducted in de novo kidn...
Proceedings of the 13th international transplantation symposia: mTOR-inhibition: what have we learned and how so we best apply the learning
A moral dilemma argument against clinical trials of incentives for kidney donation.
Commercial transplant tourism results in significant harm to both kidney donors and recipients. However, proponents of incentives for kidney donation assert that proper oversight of the process prevents these ...
Contraindications to kidney transplantation: uneven grounds?
Determining eligibility for a kidney transplant is an important decision. Practice guidelines define contraindications to transplantation; however many are not evidence based. Canadian guidelines recommend tha...
Skin cancer in solid organ transplant recipients: are mTOR inhibitors a game changer?
While immunosuppressive agents are necessary to prevent the rejection of transplanted organs, and are a great medical success story for protecting against early allograft loss, graft and patient survival over ...
Vitamin D and cinacalcet administration pre-transplantation predict hypercalcaemic hyperparathyroidism post-transplantation: a case-control study of 355 deceased-donor renal transplant recipients over 3 years
The effects of pre-transplantation medication for secondary hyperparathyroidism on post-transplantation parathyroid hormone (PTH) and calcium levels have not yet been conclusively determined. Therefore, this s...
Effect of left atrial and ventricular abnormalities on renal transplant recipient outcome—a single-center study
Premature cardiovascular (CV) death is the commonest cause of death in renal transplant recipients. Abnormalities of left ventricular (LV) structure (collectively termed uremic cardiomyopathy) and left atrial ...
Multipotent adult progenitor cells decrease cold ischemic injury in ex vivo perfused human lungs: an initial pilot and feasibility study
Primary graft dysfunction (PGD) is a significant cause of early morbidity and mortality following lung transplantation. Improved organ preservation techniques will decrease ischemia-reperfusion injury (IRI) co...
Factors influencing survival after kidney transplant failure
The failure of a kidney transplant is now a common reason for initiation of dialysis therapy. Kidney transplant recipients commencing dialysis have greater morbidity and mortality than transplant-naïve, incide...
Cascade plasmapheresis (CP) as a preconditioning regime in ABO-incompatible live related donor liver transplants (ABOi-LDLT)
ABO-incompatible live donor liver transplant (ABOi-LDLT) is being widely done to bridge the gap of demand and supply of organs. Different desensitization regimes are being used to reduce titer of blood group a...
The feasibility and applications of non-invasive cardiac output monitoring, thromboelastography and transit-time flow measurement in living-related renal transplantation surgery: results of a prospective pilot observational study
Delayed graft function (DGF) remains a significant and detrimental postoperative phenomenon following living-related renal allograft transplantation, with a published incidence of up to 15%. Early therapeutic ...
Active video gaming in patients with renal transplant: a pilot study
Patients with renal transplant are at higher risk of mortality from cardiovascular disease (CVD) compared with the general population. Physical activity has been shown to reduce the risk of CVD mortality in th...
A randomized controlled trial of daclizumab versus anti-thymocyte globulin induction for heart transplantation
The purpose of this study was to test the efficacy and safety of daclizumab (DZM) versus anti-thymocyte globulin (ATG) as a component of induction therapy in heart transplant recipients.
Development of a preclinical model of donation after circulatory determination of death for translational application
Extracorporeal membranous oxygenation is proposed for abdominal organ procurement from donation after circulatory determination of death (DCD). In France, the national Agency of Biomedicine supervises the proc...

An in-progress, open-label, multi-centre study (SAILOR) evaluating whether a steroid-free immunosuppressive protocol, based on ATG induction and a low tacrolimus dose, reduces the incidence of new onset diabetes after transplantation
Corticosteroids and calcineurin inhibitors (CNIs) are included in renal transplantation immunosuppressive protocols around the world. Well-known side effects are associated with the use of these drugs, includi...
Safety and efficacy of outpatient bronchoscopy in lung transplant recipients - a single centre analysis of 3,197 procedures
Bronchoscopy represents an important diagnostic and therapeutic tool in the management of lung transplant (LTx) recipients. Outpatient bronchoscopy reduces health costs and may improve quality of life amongst ...
Systematic review of melanoma incidence and prognosis in solid organ transplant recipients
Cutaneous melanoma carries the potential for substantial morbidity and mortality in the solid organ transplant population. We systematically reviewed the literature published from January 1995 to January 2012 ...
Influence on ICU course, outcome and costs for lung transplantation after implementation of the new Swiss transplantation law
The Swiss organ allocation system for donor lungs was implemented on 1 July 2007. The effects of this implementation on patient selection, intensive care unit course, outcomes and intensive care costs are unkn...
Organ and tissue donation in clinical settings: a systematic review of the impact of interventions aimed at health professionals
In countries where presumed consent for organ donation does not apply, health professionals (HP) are key players for identifying donors and obtaining their consent. This systematic review was designed to verif...
A prospective cohort conversion study of twice-daily to once-daily extended-release tacrolimus: role of ethnicity
Tacrolimus is a widely used calcineurin inhibitor in kidney transplantation. It is available as twice-daily Prograf® (Tac-BID) and once-daily Advagraf® (Tac-OD). Although therapeutically equivalent, some patie...
Center volume, competition, and outcome in German liver transplant centers
Volume and outcome relation in german liver transplant centers: what lessons can be learned.
The volume and outcome relationship for transplant procedures has become one of the major topics during discussions about consequences following the organ transplantation scandal of wait-list manipulations in ...
Reviewer acknowledgement 2013
The Editors of Transplantation Research would like to thank all our reviewers who have contributed to the journal in Volume 2 (2013).
Long-term mycophenolate monotherapy in human leukocyte antigen (HLA)-identical living-donor kidney transplantation
We analyzed all PRA-negative patients who received a first kidney transplant from an HLA-identical living donor. The patients received no antibody induction. An intraoperative bolus of 500 mg of methylpredniso...
Eligibility for the kidney transplant wait list: a model for conceptualizing patient risk
Determining eligibility for a kidney transplant is one of the most important decisions facing nephrologists. It is assumed that the harm of kidney transplantation is minimal and most will benefit. The purpose ...
Timing of rabbit antithymocyte globulin induction therapy in kidney transplantation: an observational cohort study
Literature on the timing of rabbit antithymocyte globulin (rATG) induction and its effects on kidney transplant outcomes is limited. The manufacturer recommends that the first dose be given intra-operatively, ...
Challenges in machine perfusion preservation for liver grafts from donation after circulatory death
Donation after circulatory death (DCD) is a promising solution to the critical shortage of donor graft tissue. Maintaining organ viability after donation until transplantation is essential for optimal graft fu...
JAK3 inhibition: what potential for the future?
JAK3 inhibition with the CP-690,550 compound has an immunosuppressive potency in murine models, nonhuman primates and humans. This drug blocks STAT5 activation in most T-cell subpopulations but less effectivel...
This article is part of a Supplement: Volume 2 Supplement 1
Alemtuzumab induction therapy in solid organ transplantation
Alemtuzumab (Campath) is a monoclonal antibody that has a profound lymphocyte-depleting effect, targeting the CD52 antigen that is present on all lymphocytes. Alemtuzumab has been used for the treatment of chr...
Optimising the use of mTOR inhibitors in renal transplantation
Renal transplantation is the treatment of choice for end-stage renal failure. Although advances in immunosuppression have led to improvements in short-term outcomes, graft survival beyond 5 to 10 years has not...
Conversion to mTOR-inhibitor-based immunosuppression: which patients and when?
Mammalian target of rapamycin (mTOR) inhibitors are currently considered an alternative immunosuppressive treatment that can prevent the nephrotoxicity, viral infections and malignancies that are associated wi...
The influence of mTOR inhibitors on immunity and the relationship to post-transplant malignancy
The known role of mammalian target of rapamycin (mTOR) in the immune response has been rapidly evolving, from what was once thought to be a simple immunosuppressive antiproliferative effect on T cells to a ver...
What are the key challenges we face in kidney transplantation today?
Transplantation is more predictable than it was 20 to 30 years ago and innovation over the last 20 years has been rapid, delivering substantial short-term and medium-term improvements. The challenges ahead are...
A new risk score model to predict the presence of significant coronary artery disease in renal transplant candidates
Renal transplant candidates are at high risk of coronary artery disease (CAD). We sought to develop a new risk score model to determine the pre-test probability of the occurrence of significant CAD in renal tr...
Standardization of whole blood immune phenotype monitoring for clinical trials: panels and methods from the ONE study
Immune monitoring by flow cytometry is a fast and highly informative way of studying the effects of novel therapeutics aimed at reducing transplant rejection or treating autoimmune diseases. The ONE Study cons...
IL-13 signaling via IL-13Rα 2 triggers TGF-β 1 -dependent allograft fibrosis
Allograft fibrosis still remains a critical problem in transplantation, including heart transplantation. The IL-13/TGF-β 1 interaction has previously been identified as a key pathway orchestrating fibrosis in diff...
Long-term follow-up of kidney transplant recipients: comparison of hospitalization rates to the general population
Kidney transplant recipients are recognized as a vulnerable population that is at increased risk of adverse health outcomes. However, there have been few studies that have compared hospital-related morbidity o...
Efficacy and safety of concentration-controlled everolimus with reduced-dose cyclosporine in Japanese de novo renal transplant patients: 12-month results
No study to date has evaluated the efficacy and safety of everolimus with reduced-exposure cyclosporine in Japanese de-novo renal transplant (RTx) patients.
Comparative analysis of in situ versus ex situ perfusion on flow and microcirculation in kidney procurement: research on a porcine model
The first crucial step in transplantation appears to be the effective rinsing of the graft during organ procurement. Even though there is strong suspicion that ex situ perfusion results in better rinsing of the g...
Extended pancreas donor program – the EXPAND study rationale and study protocol
Simultaneous pancreas kidney transplantation (SPK), pancreas transplantation alone (PTA) or pancreas transplantation after kidney (PAK) are the only curative treatment options for patients with type 1 (juvenil...
Induction with interleukin-2 antagonist for transplantation of kidneys from older deceased donors: an observational study
The most important limiting factor in kidney transplantation is the scarcity of donor organs. Consequently, there is an increased use worldwide of kidneys from older deceased donors. High donor age is a known ...
Exploiting paracrine mechanisms of tissue regeneration to repair damaged organs
Stem cells have been studied for many years for their potential to repair damaged organs in the human body. Although many different mechanisms have been suggested as to how stem cells may initiate and facilita...
Transplantation Research
ISSN: 2047-1440
- General enquiries: [email protected]
Information
- Author Services
Initiatives
You are accessing a machine-readable page. In order to be human-readable, please install an RSS reader.
All articles published by MDPI are made immediately available worldwide under an open access license. No special permission is required to reuse all or part of the article published by MDPI, including figures and tables. For articles published under an open access Creative Common CC BY license, any part of the article may be reused without permission provided that the original article is clearly cited. For more information, please refer to https://www.mdpi.com/openaccess .
Feature papers represent the most advanced research with significant potential for high impact in the field. A Feature Paper should be a substantial original Article that involves several techniques or approaches, provides an outlook for future research directions and describes possible research applications.
Feature papers are submitted upon individual invitation or recommendation by the scientific editors and must receive positive feedback from the reviewers.
Editor’s Choice articles are based on recommendations by the scientific editors of MDPI journals from around the world. Editors select a small number of articles recently published in the journal that they believe will be particularly interesting to readers, or important in the respective research area. The aim is to provide a snapshot of some of the most exciting work published in the various research areas of the journal.
Original Submission Date Received: .
- Active Journals
- Find a Journal
- Journal Proposal
- Proceedings Series
- For Authors
- For Reviewers
- For Editors
- For Librarians
- For Publishers
- For Societies
- For Conference Organizers
- Open Access Policy
- Institutional Open Access Program
- Special Issues Guidelines
- Editorial Process
- Research and Publication Ethics
- Article Processing Charges
- Testimonials
- Preprints.org
- SciProfiles
- Encyclopedia

Article Menu

- Subscribe SciFeed
- Recommended Articles
- Google Scholar
- on Google Scholar
- Table of Contents
Find support for a specific problem in the support section of our website.
Please let us know what you think of our products and services.
Visit our dedicated information section to learn more about MDPI.
JSmol Viewer
Pushing the survival bar higher: two decades of innovation in lung transplantation.

1. Introduction
2. patient selection and indications, 3. transplant indication for ards.
- Patients should be younger than 65 years, since the results of ECMO as a bridge to transplantation (BTT) have been worse in older patients. However, not only chronological age but also patient frailty should be considered.
- Patients should preferably only have single-organ dysfunction. However, patients requiring temporary hemodialysis have been successfully transplanted too. Concomitant liver dysfunction or left heart failure should be considered a contraindication to lung transplantation. The development of right heart failure due to secondary pulmonary hypertension should not be considered a contraindication to transplantation. In this case, veno-venous (v-v) ECMO should be upgraded to veno-arterial (v-a) or veno-arterial-venous (v-a-v) ECMO.
- Enough time should be allowed for lung recovery, usually 4–6 weeks after the initial event. Evaluation for lung transplantation may be considered earlier than 4 weeks, in case of potentially lethal pulmonary complications that cannot be managed medically or through the use of ECMO.
- There should be radiological evidence of irreversible lung disease, such as extensive honeycombing, cystic changes, reticular opacities, and traction bronchiectasis, >80% lung involvement, and a right atrium to left atrium ratio > 1; these are associated with an extended period of static respiratory mechanics or ECMO parameters [ 19 ]. The presence of secondary pulmonary arterial hypertension should be also considered a sign of irreversibility.
- Patients should be awake and able to discuss transplantation. The advantages of “awake” ECMO as a bridge to lung transplantation are well known. However, in some patients, who are otherwise good candidates for transplantation, spontaneous breathing is not possible. In this case, a patient’s next-of-kin may consent to transplantation.
- Patients should be able to participate in physical rehabilitation while on the transplantation waiting list.
- Patients should fulfil the remaining typical criteria for transplantation; these include, for example, an adequate body mass index and an absence of other notable conditions, such as severe coronary artery disease or a history of active smoking.
- Patients should have a negative SARS-CoV-2 virology status.
- Transplantation for ARDS should be performed only in high-volume centers that have substantial experience with ECMO as a bridge to transplantation.
- The transplant center should have access to a broad donor pool and low waiting list mortality. The clinical condition of patients with irreversible lung failure after ARDS may rapidly worsen, thus precluding transplantation. Continuous patient re-evaluation is therefore needed.
- These criteria and the indication for transplantation should be evaluated, discussed and approved by the multidisciplinary transplant conference. A multidisciplinary approach is of paramount importance in successfully transplanting patients after irreversible lung damage due to ARDS ( Figure 2 ).
4. Donor Optimization and EVLP
5. ecls or the holy grail in lung transplantation, 6. antibody-mediated rejection in lung transplantation, 7. conclusions and future directions, author contributions, institutional review board statement, informed consent statement, data availability statement, conflicts of interest, list of abbreviations.
| ARDS | acute respiratory distress syndrome |
| BOS | bronchiolitis obliterans syndrome |
| BTT | bridge to transplantation |
| CABG | coronary artery bypass grafting |
| CBP | cardiopulmonary bypass |
| CLAD | chronic lung allograft dysfunction |
| CO | cardiac output |
| DCD | donation after circulatory death |
| eDSA | early donor-specific anti-HLA antibodies |
| ECD | extended-criteria donor |
| ECLS | extracorporeal life support |
| ECMO | extracorporeal membrane oxygenation |
| ET | Eurotransplant |
| EVLP | ex vivo lung perfusion |
| ISHLT | International Society of Heart and Lung Transplantation |
| LAS | lung allocation score |
| MFI | mean fluorescence intensity |
| PGD | primary graft dysfunction |
| RBCs | red blood cells |
| RAS | restrictive allograft syndrome |
- Chambers, D.S.; Cherikh, W.S.; Harhay, M.O.; Hayes, D., Jr.; Hsich, E.; Khush, K.K.; Meiser, B.; Potena, L.; Rossano, J.W.; Toll, A.E.; et al. The international thoracic organ transplant registry of the International Society for Heart and Lung Transplantation: Thirty-sixth adult lung and heart-lung transplantation report–2019; focus theme: Donor and recipient size match. J. Heart Lung Transplant. 2019 , 38 , 1042–1055. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Goldfarb, S.B.; Hayes, D., Jr.; Levvey, B.J.; Cherikh, W.S.; Chambers, D.C.; Khush, K.K.; Kucheryavaya, A.Y.; Meiser, B.; Rossano, J.W.; Stehlik, J.; et al. The Registry of the International Society for Heart and Lung Transplantation: Twenty-First Pediatric Lung and Heart-Lung Transplantation Report–2018; Focus Theme: Multiorgan Transplantation. J. Heart Lung Transplant. 2018 , 37 , 1196–1206. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Hayes, D.; Cherikh, W.; Chambers, D.; Harhay, M.O.; Khush, K.K.; Lehman, R.R.; Meiser, B.; Rossano, J.W.; Hsich, E.; Potena, L.; et al. The International Thoracic Organ Transplant Registry of the International Society for Heart and Lung Transplantation: Twenty-second pediatric lung and heart-lung transplantation report-2019; Focus theme: Donor and recipient size match. J. Heart Lung Transplant. 2019 , 38 , 1015–1027. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Verleden, S.E.; Todd, J.L.; Sato, M.; Palmer, S.M.; Martinu, T.; Pavlisko, E.N.; Vos, R.; Neyrinck, A.; Van Raemdonck, D.; Saito, T.; et al. Impact of CLAD phenotype on survival after lung re-transplantation: A multicenter study. Am. J. Transplant. 2015 , 15 , 2223–2230. [ Google Scholar ] [ CrossRef ]
- DerHovanessian, A.; Wallace, W.D.; Lynch, J.P., III; Belperio, J.A.; Weigt, S.S. Chronic lung allograft dysfunction: Evolving concepts and therapies. Semin. Respir. Crit. Care Med. 2018 , 39 , 155–171. [ Google Scholar ] [ CrossRef ]
- Kulkarni, H.S.; Cherikh, W.S.; Chambers, D.C.; Garcia, V.C.; Hachem, R.R.; Kreisel, D.; Puri, V.; Kozower, B.D.; Byers, D.E.; Witt, C.A.; et al. Bronchiolitis obliterans syndrome-free survival after lung transplantation: An International Society for Heart and Lung Transplantation Thoracic Transplant Registry analysis. J. Heart Lung Transplant. 2019 , 38 , 5–16. [ Google Scholar ] [ CrossRef ]
- van der Mark, S.C.; Hoek, R.A.S.; Hellemons, M.E. Developments in lung transplantation over the past decade. Eur. Respir. Rev. 2020 , 29 , 190132. [ Google Scholar ] [ CrossRef ]
- Weill, D.; Benden, C.; Corris, P.A.; Dark, J.H.; Davis, R.D.; Keshavjee, S.; Lederer, D.J.; Mulligan, M.J.; Patterson, G.A.; Singer, L.G.; et al. A consensus document for the selection of lung transplant candidates: 2014—An update from the Pulmonary Transplantation Council of the International Society for Heart and Lung Transplantation. J. Heart Lung Transplant. 2015 , 34 , 1–15. [ Google Scholar ] [ CrossRef ]
- Gottlieb, J.; Greer, M.; Sommerwerck, U.; Deuse, T.; Witt, C.; Schramm, R.; Hagl, C.; Strueber, M.; Smits, J.M. Introduction of the lung allocation score in Germany. Am. J. Transplant. 2014 , 14 , 1318–1327. [ Google Scholar ] [ CrossRef ]
- Tsuang, W.M.; Snyder, L.D.; Budev, M.M. Perspectives on donor lung allocation from both sides of the Atlantic: The United States. Clin. Transplant. 2020 , 34 , e13873. [ Google Scholar ] [ CrossRef ]
- Holm, A.M.; Immer, F.; Benden, C. Lung allocation for transplant: The European perspective. Clin. Transplant. 2020 , 34 , e13883. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Parker, W.F.; Dussault, N.E.; Jablonski, R.; Garrity, E.R.; Churpek, M.M. Assessing the accuracy of the lung allocation score. J. Heart Lung Transplant. 2022 , 41 , 217–225. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Brahmbhatt, J.M.; Hee Wai, T.; Goss, C.H.; Lease, E.D.; Merlo, C.A.; Kapnadak, S.G.; Ramos, K.J. The lung allocation score and other available models lack predictive accuracy for post-lung transplant survival. J. Heart Lung Transplant. 2022 , 41 , 1063–1074. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Kolaitis, N.A.; Chen, H.; Calabrese, D.R.; Kumar, K.; Obata, J.; Bach, C.; Golden, J.A.; Simon, M.A.; Kukreja, J.; Hays, S.R.; et al. The Lung Allocation Score Remains Inequitable for Patients with Pulmonary Arterial Hypertension, Even after the 2015 Revision. Am. J. Respir. Crit. Care Med. 2023 , 207 , 300–311. [ Google Scholar ] [ CrossRef ]
- Valapour, M.; Lehr, C.J.; Wey, A.; Skeans, M.A.; Miller, J.; Lease, E.D. Expected effect of the lung Composite Allocation Score system on US lung transplantation. Am. J. Transplant. 2022 , 22 , 2971–2980, Erratum in: Am. J. Transplant. 2024 , 24 , 1520. [ Google Scholar ] [ CrossRef ]
- Ringshausen, F.C.; Sauer-Heilborn, A.; Büttner, T.; Dittrich, A.M.; Schwerk, N.; Ius, F.; Nährlich, L.; Welte, T.; Greer, M. Lung transplantation for end-stage cystic fibrosis before and after the availability of elexacaftor-tezacaftor-ivacaftor, Germany, 2012–2021. Eur. Respir. J. 2023 , 61 , 2201402. [ Google Scholar ] [ CrossRef ]
- Hoeper, M.M.; Badesch, D.B.; Ghofrani, H.A.; Gibbs, J.S.R.; Gomberg-Maitland, M.; McLaughlin, V.V.; Preston, I.R.; Souza, R.; Waxman, A.B.; STELLAR Trial Investigators; et al. Phase 3 Trial of Sotatercept for Treatment of Pulmonary Arterial Hypertension. N. Engl. J. Med. 2023 , 388 , 1478–1490. [ Google Scholar ] [ CrossRef ]
- Iablonskii, P.; Carlens, J.; Mueller, C.; Aburahma, K.; Niehaus, A.; Boethig, D.; Franz, M.; Floethmann, K.; Sommer, W.; Optenhoefel, J.; et al. Indications and outcome after lung transplantation in children under 12 years of age: A 16-year single center experience. J. Heart Lung Transplant. 2022 , 41 , 226–236. [ Google Scholar ] [ CrossRef ]
- Alessandri, F.; Di Nardo, M.; Ramanathan, K.; Brodie, D.; MacLaren, G. Extracorporeal membrane oxygenation for COVID-19-related acute respiratory distress syndrome: A narrative review. J. Intensive Care 2023 , 11 , 5. [ Google Scholar ] [ CrossRef ]
- Avella, D.; Neumann, H.; Bharat, A. Lung Transplantation for Coronavirus Disease-2019 Patients and Coronavirus Disease-2019 in Lung Transplant Recipients. Clin. Chest Med. 2023 , 44 , 191–199. [ Google Scholar ] [ CrossRef ]
- Lepper, P.M.; Barrett, N.A.; Swol, J.; Lorusso, R.; Di Nardo, M.; Belliato, M.; Belohlavek, J.; Broman, L.M. Perception of prolonged extracorporeal membrane oxygenation in Europe: An EuroELSO survey. Perfusion 2020 , 35 , 81–85. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Bojic, A.; Schellongowski, P.; Robak, O.; Hermann, A.; Buchtele, N.; Nagler, B.; Lamm, W.; Staudinger, T. Long-term Respiratory Extracorporeal Membrane Oxygenation and Prognosis: A Retrospective Analysis. ASAIO J. 2021 , 67 , 345–352. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Chang, Y.; Lee, S.O.; Shim, T.S.; Choi, S.H.; Kim, H.R.; Kim, Y.H.; Kim, D.K.; Do, K.-H.; Choi, I.-C.; Hong, S.-B.; et al. Lung Transplantation as a Therapeutic Option in Acute Respiratory Distress Syndrome. Transplantation 2018 , 102 , 829–837. [ Google Scholar ] [ CrossRef ]
- Harano, T.; Ryan, J.P.; Chan, E.G.; Noda, K.; Morrell, M.R.; Luketich, J.D.; Sanchez, P.G. Lung transplantation for the treatment of irreversible acute respiratory distress syndrome. Clin. Transplant. 2021 , 35 , e14182. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Gottlieb, J.; Lepper, P.M.; Berastegui, C.; Montull, B.; Wald, A.; Parmar, J.; Magnusson, J.M.; Schönrath, F.; Laisaar, T.; Michel, S.; et al. Lung transplantation for acute respiratory distress syndrome: A retrospective European cohort study. Eur. Respir. J. 2022 , 59 , 2102078. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Frick, A.E.; Gan, C.T.; Vos, R.; Schwarz, S.; Kraft, F.; Kifjak, D.; Neyrinck, A.P.; Van Raemdonck, D.E.; Klepetko, W.; Jaksch, P.; et al. Lung transplantation for acute respiratory distress syndrome: A multicenter experience. Am. J. Transplant. 2022 , 22 , 144–153. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Cypel, M.; Keshavjee, S. When to consider lung transplantation for COVID-19. Lancet Respir. Med. 2020 , 8 , 944–946. [ Google Scholar ] [ CrossRef ]
- Bharat, A.; Machuca, T.N.; Querrey, M.; Kurihara, C.; Garza-Castillon, R., Jr.; Kim, S.; Lung, K.; Yeldandi, A.; Bharat, A. Early outcomes after lung transplantation for severe COVID-19: A series of the first consecutive cases from four countries. Lancet Respir. Med. 2021 , 9 , 487–497. [ Google Scholar ] [ CrossRef ]
- Roach, A.; Chikwe, J.; Catarino, P.; Rampolla, R.; Noble, P.W.; Megna, D.; Chen, Q.; Emerson, D.; Egorova, N.; Keshavjee, S.; et al. Lung Transplantation for COVID-19-Related Respiratory Failure in the United States. N. Engl. J. Med. 2022 , 386 , 1187–1188. [ Google Scholar ] [ CrossRef ]
- Lang, C.; Ritschl, V.; Augustin, F.; Lang, G.; Moser, B.; Taghavi, S.; Murakoezy, G.; Lambers, C.; Flick, H.; Koestenberger, M.; et al. Clinical relevance of lung transplantation for COVID-19 ARDS: A nationwide study. Eur. Respir. J. 2022 , 60 , 2102404. [ Google Scholar ] [ CrossRef ]
- Razia, D.; Olson, M.T.; Grief, K.; Walia, R.; Bremner, R.M.; Smith, M.A.; Tokman, S. Hospitalized patients with irreversible lung injury from COVID-19 have higher morbidity but similar 1-year survival after lung transplant compared to hospitalized patients transplanted for restrictive lung disease. J. Heart Lung Transplant. 2023 , 42 , 255–263. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Freischlag, K.; Lynch, T.J.; Ievlev, V.; Gries, C.; Keech, J.C.; Arshava, E.V.; Pena, T.; Klesney-Tait, J.A.; Parekh, K.R. A Matched Survival Analysis of Lung Transplant Recipients with Coronavirus Disease 2019-Related Respiratory Failure. Ann. Thorac. Surg. 2023 , 116 , 819–828. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Bermudez, C.; Bermudez, F.; Courtwright, A.; Richards, T.; Diamond, J.; Cevasco, M.; Blumberg, E.; Christie, J.; Usman, A.; Crespo, M.M. Lung transplantation for COVID-2019 respiratory failure in the United States: Outcomes 1-year posttransplant and the impact of preoperative extracorporeal membrane oxygenation support. J. Thorac. Cardiovasc. Surg. 2024 , 167 , 384–395. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Copeland, H.; Hayanga, J.A.; Neyrinck, A.; MacDonald, P.; Dellgren, G.; Bertolotti, A.; Khuu, T.; Burrows, F.; Copeland, J.G.; Gooch, D.; et al. Donor heart and lung procurement: A consensus statement. J. Heart Lung Transplant. 2020 , 39 , 501–517, Erratum in: J. Heart Lung Transplant. 2020 , 39 , 734. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Kirk, R.; Dipchand, A.I.; Davies, R.R.; Miera, O.; Chapman, G.; Conway, J.; Denfield, S.; Gossett, J.G.; Johnson, J.; McCulloch, M.; et al. ISHLT consensus statement on donor organ acceptability and management in pediatric heart transplantation. J. Heart Lung Transplant. 2020 , 39 , 331–341. [ Google Scholar ] [ CrossRef ]
- Yu, W.S.; Son, J. Donor Selection, Management, and Procurement for Lung Transplantation. J. Chest Surg. 2022 , 55 , 277–282. [ Google Scholar ] [ CrossRef ]
- Zhou, A.L.; Larson, E.L.; Ruck, J.M.; Ha, J.S.; Casillan, A.J.; Bush, E.L. Current status and future potential of ex vivo lung perfusion in clinical lung transplantation. Artif. Organs. 2023 , 47 , 1700–1709. [ Google Scholar ] [ CrossRef ]
- Yu, J.; Zhang, N.; Zhang, Z.; Li, Y.; Gao, J.; Chen, C.; Wen, Z. Diagnostic and Therapeutic Implications of Ex Vivo Lung Perfusion in Lung Transplantation: Potential Benefits and Inherent Limitations. Transplantation 2023 , 107 , 105–116. [ Google Scholar ] [ CrossRef ]
- Ahmad, K.; Pluhacek, J.L.; Brown, A.W. Ex Vivo Lung Perfusion: A Review of Current and Future Application in Lung Transplantation. Pulm. Ther. 2022 , 8 , 149–165. [ Google Scholar ] [ CrossRef ]
- Miller, C.L.; O, J.M.; Allan, J.S.; Madsen, J.C. Novel approaches for long-term lung transplant survival. Front. Immunol. 2022 , 13 , 931251. [ Google Scholar ] [ CrossRef ]
- Watanabe, T.; Cypel, M.; Keshavjee, S. Ex vivo lung perfusion. J. Thorac. Dis. 2021 , 13 , 6602–6617. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Iske, J.; Hinze, C.A.; Salman, J.; Haverich, A.; Tullius, S.G.; Ius, F. The potential of ex vivo lung perfusion on improving organ quality and ameliorating ischemia reperfusion injury. Am. J. Transplant. 2021 , 21 , 3831–3839. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Moreno Garijo, J.; Roscoe, A. Ex-vivo lung perfusion. Curr. Opin. Anaesthesiol. 2020 , 33 , 50–54. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Whitson, B.A.; Prekker, M.E.; Herrington, C.S.; Whelan, T.P.; Radosevich, D.M.; Hertz, M.I.; Dahlberg, P.S. Primary graft dysfunction and long-term pulmonary function after lung transplantation. J. Heart Lung Transplant. 2007 , 26 , 1004–1011. [ Google Scholar ] [ CrossRef ]
- Warnecke, G.; Moradiellos, J.; Tudorache, I.; Kühn, C.; Avsar, M.; Wiegmann, B.; Sommer, W.; Ius, F.; Kunze, C.; Gottlieb, J.; et al. Normothermic perfusion of donor lungs for preservation and assessment with the Organ Care System Lung before bilateral transplantation: A pilot study of 12 patients. Lancet 2012 , 380 , 1851–1858. [ Google Scholar ] [ CrossRef ]
- Tikkanen, J.M.; Cypel, M.; Machuca, T.N.; Azad, S.; Binnie, M.; Chow, C.-W.; Chaparro, C.; Hutcheon, M.; Yasufuku, K.; de Perrot, M.; et al. Functional outcomes and quality of life after normothermic ex vivo lung perfusion lung transplantation. J. Heart Lung Transplant. 2015 , 34 , 547–556. [ Google Scholar ] [ CrossRef ]
- Slama, A.; Schillab, L.; Barta, M.; Benedek, A.; Mitterbauer, A.; Hoetzenecker, K.; Taghavi, S.; Lang, G.; Matilla, J.; Ankersmit, H.; et al. Standard donor lung procurement with normothermic ex vivo lung perfusion: A prospective randomized clinical trial. J. Heart Lung Transplant. 2017 , 36 , 744–753. [ Google Scholar ] [ CrossRef ]
- Warnecke, G.; Van Raemdonck, D.; Smith, M.A.; Massard, G.; Kukreja, J.; Rea, F.; Loor, G.; De Robertis, F.; Nagendran, J.; Dhital, K.K.; et al. Normothermic ex-vivo preservation with the portable Organ Care System Lung device for bilateral lung transplantation (INSPIRE): A randomised, open-label, non-inferiority, phase 3 study. Lancet Respir. Med. 2018 , 6 , 357–367. [ Google Scholar ] [ CrossRef ]
- Cypel, M.; Yeung, J.C.; Liu, M.; Anraku, M.; Chen, F.; Karolak, W.; Sato, M.; Laratta, J.; Azad, S.; Madonik, M.; et al. Normothermic ex vivo lung perfusion in clinical lung transplantation. N. Engl. J. Med. 2011 , 364 , 1431–1440. [ Google Scholar ] [ CrossRef ]
- Fisher, A.; Andreasson, A.; Chrysos, A.; Lally, J.; Mamasoula, C.; Exley, C.; Wilkinson, J.; Qian, J.; Watson, G.; Lewington, O.; et al. An observational study of Donor Ex Vivo Lung Perfusion in UK lung transplantation: DEVELOP-UK. Health Technol. Assess. 2016 , 20 , 1–276. [ Google Scholar ] [ CrossRef ]
- Loor, G.; Warnecke, G.; Villavicencio, M.A.; Smith, M.A.; Kukreja, J.; Ardehali, A.; Hartwig, M.; Daneshmand, M.A.; Hertz, M.I.; Huddleston, S.; et al. Portable normothermic ex-vivo lung perfusion, ventilation, and functional assessment with the Organ Care System on donor lung use for transplantation from extended-criteria donors (EXPAND): A single-arm, pivotal trial. Lancet Respir. Med. 2019 , 7 , 975–984. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Abdoul, N.; Legeai, C.; Cantrelle, C.; Mercier, O.; Olland, A.; Mordant, P.; Thomas, P.A.; Jougon, J.; Tissot, A.; Maury, J.-M.; et al. Impact of ex vivo lung perfusion on brain-dead donor lung utilization: The French experience. Am. J. Transplant. 2022 , 22 , 1409–1417. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Noda, K.; Chan, E.G.; Furukawa, M.; Ryan, J.P.; Clifford, S.; Luketich, J.D.; Sanchez, P.G.; UPMC EVLP Group. Single-center experience of ex vivo lung perfusion and subsequent lung transplantation. Clin. Transplant. 2023 , 37 , e14901. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Chen, Q.; Malas, J.; Krishnan, A.; Thomas, J.; Megna, D.; Egorova, N.; Chikwe, J.; Bowdish, M.E.; Catarino, P. Limited cumulative experience with ex vivo lung perfusion is associated with inferior outcomes after lung transplantation. J. Thorac. Cardiovasc. Surg. 2024 , 167 , 371–379. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Halpern, S.E.; Kesseli, S.J.; Au, S.; Krischak, M.K.; Olaso, D.G.; Smith, H.; Tipton, G.; Jamieson, I.R.; Barbas, A.S.; Haney, J.C.; et al. Lung transplantation after ex vivo lung perfusion versus static cold storage: An institutional cost analysis. Am. J. Transplant. 2022 , 22 , 552–564. [ Google Scholar ] [ CrossRef ]
- Peel, J.K.; Keshavjee, S.; Naimark, D.; Liu, M.; Del Sorbo, L.; Cypel, M.; Barrett, K.; Pullenayegum, E.M.; Sander, B. Determining the impact of ex-vivo lung perfusion on hospital costs for lung transplantation: A retrospective cohort study. J. Heart Lung Transplant. 2023 , 42 , 356–367. [ Google Scholar ] [ CrossRef ]
- Ali, A.; Wang, A.; Ribeiro, R.V.P.; Beroncal, E.L.; Baciu, C.; Galasso, M.; Gomes, B.; Mariscal, A.; Hough, O.; Brambate, E.; et al. Static lung storage at 10 °C maintains mitochondrial health and preserves donor organ function. Sci. Transl. Med. 2021 , 13 , eabf7601. [ Google Scholar ] [ CrossRef ]
- Ali, A.; Hoetzenecker, K.; de la Cruz, J.L.C.-C.; Schwarz, S.; Gil Barturen, M.; Tomlinson, G.; Yeung, J.; Donahoe, L.; Yasufuku, K.; Pierre, A.; et al. Extension of Cold Static Donor Lung Preservation at 10 °C. NEJM Evid. 2023 , 2 , EVIDoa2300008. [ Google Scholar ] [ CrossRef ]
- Provoost, A.-L.; Novysedlak, R.; Van Raemdonck, D.; Van Slambrouck, J.; Prisciandaro, E.; Vandervelde, C.M.; Barbarossa, A.; Jin, X.; Denaux, K.; De Leyn, P.; et al. Lung transplantation following controlled hypothermic storage with a portable lung preservation device: First multicenter European experience. Front. Cardiovasc. Med. 2024 , 11 , 1370543. [ Google Scholar ] [ CrossRef ]
- Ius, F.; Tudorache, I.; Warnecke, G. Extracorporeal support, during and after lung transplantation: The history of an idea. J. Thorac. Dis. 2018 , 10 , 5131–5148. [ Google Scholar ] [ CrossRef ]
- Rajagopal, K.; Hoeper, M.M. State of the Art: Bridging to lung transplantation using artificial organ support technologies. J. Heart Lung Transplant. 2016 , 35 , 1385–1398. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Reeb, J.; Olland, A.; Renaud, S.; Lejay, A.; Santelmo, N.; Massard, G.; Falcoz, P.E. Vascular access for extracorporeal life support: Tips and tricks. J. Thorac. Dis. 2016 , 8 (Suppl 4), S353–S363. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Fernandez, R.; DeCamp, M.; Bharat, A. A novel strategy for cardiopulmonary support during lung transplantation. J. Thorac. Dis. 2018 , 10 , E142–E144. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Diaz-Guzman, E.; Sharma, N.S.; Wille, K.; Hoopes, C.W. Use of a novel pulmonary artery cannula to provide extracorporeal membrane oxygenation as a bridge to lung transplantation. J. Heart Lung Transplant. 2016 , 35 , 1051–1053. [ Google Scholar ] [ CrossRef ]
- Bermudez, C.A.; Zaldonis, D.; Fan, M.H.; Pilewski, J.M.; Crespo, M.M. Prolonged Use of the Hemolung Respiratory Assist System as a Bridge to Redo Lung Transplantation. Ann. Thorac. Surg. 2015 , 100 , 2330–2333. [ Google Scholar ] [ CrossRef ]
- Fischer, S.; Simon, A.R.; Welte, T.; Hoeper, M.M.; Meyer, A.; Tessmann, R.; Gohrbandt, B.; Gottlieb, J.; Haverich, A.; Strueber, M. Bridge to lung transplantation with the novel pumpless interventional lung assist device NovaLung. J. Thorac. Cardiovasc. Surg. 2006 , 131 , 719–723. [ Google Scholar ] [ CrossRef ]
- Strueber, M.; Hoeper, M.M.; Fischer, S.; Cypel, M.; Warnecke, G.; Gottlieb, J.; Pierre, A.; Welte, T.; Haverich, A.; Simon, A.R.; et al. Bridge to thoracic organ transplantation in patients with pulmonary artery hypertension using a pumpless lung assist device. Am. J. Transplant. 2009 , 9 , 853–857. [ Google Scholar ] [ CrossRef ]
- Todd, E.M.; Roy, S.B.; Hashimi, A.S.; Serrone, R.; Panchanathan, R.; Kang, P.; Varsch, K.E.; Steinbock, B.E.; Huang, J.; Omar, A.; et al. Extracorporeal membrane oxygenation as a bridge to lung transplantation: A single-center experience in the present era. J. Thorac. Cardiovasc. Surg. 2017 , 154 , 1798–1809. [ Google Scholar ] [ CrossRef ]
- Biscotti, M.; Gannon, W.D.; Agerstrand, C.; Abrams, D.; Sonett, J.; Brodie, D.; Bacchetta, M. Awake Extracorporeal Membrane Oxygenation as Bridge to Lung Transplantation: A 9-Year Experience. Ann. Thorac. Surg. 2017 , 104 , 412–419. [ Google Scholar ] [ CrossRef ]
- Ius, F.; Natanov, R.; Salman, J.; Kuehn, C.; Sommer, W.; Avsar, M.; Siemeni, T.; Bobylev, D.; Poyanmehr, R.; Boethig, D.; et al. Extracorporeal membrane oxygenation as bridge to lung transplantation may not impact overall mortality risk after transplantation: Results from a 7-year single-centre experience. Eur. J. Cardiothorac. Surg. 2018 , 54 , 334–340. [ Google Scholar ] [ CrossRef ]
- Hoetzenecker, K.; Donahoe, L.; Yeung, J.C.; Azad, S.; Fan, E.; Ferguson, N.D.; Del Sorbo, L.; de Perrot, M.; Pierre, A.; Yasufuku, K.; et al. Extracorporeal life support as a bridge to lung transplantation-experience of a high-volume transplant center. J. Thorac. Cardiovasc. Surg. 2018 , 155 , 1316–1328. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Hakim, A.H.; Ahmad, U.; McCurry, K.R.; Johnston, D.R.; Pettersson, G.B.; Budev, M.; Murthy, S.; Blackstone, E.H.; Tong, M.Z. Contemporary Outcomes of Extracorporeal Membrane Oxygenation Used as Bridge to Lung Transplantation. Ann. Thorac. Surg. 2018 , 106 , 192–198. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Fuehner, T.; Kuehn, C.; Hadem, J.; Wiesner, O.; Gottlieb, J.; Tudorache, I.; Olsson, K.M.; Greer, M.; Sommer, W.; Welte, T.; et al. Extracorporeal membrane oxygenation in awake patients as bridge to lung transplantation. Am. J. Respir. Crit. Care Med. 2012 , 185 , 763–768. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Bermudez, C.A.; Rocha, R.V.; Zaldonis, D.; Bhama, J.K.; Crespo, M.M.; Shigemura, N.; Pilewski, J.M.; Sappington, P.L.; Boujoukos, A.J.; Toyoda, Y. Extracorporeal membrane oxygenation as a bridge to lung transplant: Midterm outcomes. Ann. Thorac. Surg. 2011 , 92 , 1226–1231. [ Google Scholar ] [ CrossRef ]
- Lang, G.; Taghavi, S.; Aigner, C.; Renyi-Vamos, F.; Jaksch, P.; Augustin, V.; Nagayama, K.; Ghanim, B.; Klepetko, W. Primary lung transplantation after bridge with extracorporeal membrane oxygenation: A plea for a shift in our paradigms for indications. Transplantation 2012 , 93 , 729–736. [ Google Scholar ] [ CrossRef ]
- Bittner, H.B.; Lehmann, S.; Rastan, A.; Garbade, J.; Binner, C.; Mohr, F.W.; Barten, M.J. Outcome of extracorporeal membrane oxygenation as bridge to lung transplantation and graft recovery. Ann. Thorac. Surg. 2012 , 94 , 942–949. [ Google Scholar ] [ CrossRef ]
- Javidfar, J.; Brodie, D.; Iribarne, A.; Jurado, J.; Lavelle, M.; Brenner, K.; Arcasoy, S.; Sonett, J.; Bacchetta, M. Extracorporeal membrane oxygenation as a bridge to lung transplantation and recovery. J. Thorac. Cardiovasc. Surg. 2012 , 144 , 716–721. [ Google Scholar ] [ CrossRef ]
- Schmidt, F.; Sasse, M.; Boehne, M.; Mueller, C.; Bertram, H.; Kuehn, C.; Warnecke, G.; Ono, M.; Seidemann, K.; Jack, T.; et al. Concept of “awake venovenous extracorporeal membrane oxygenation” in pediatric patients awaiting lung transplantation. Pediatr. Transplant. 2013 , 17 , 224–230. [ Google Scholar ] [ CrossRef ]
- Toyoda, Y.; Bhama, J.K.; Shigemura, N.; Zaldonis, D.; Pilewski, J.; Crespo, M.; Bermudez, C. Efficacy of extracorporeal membrane oxygenation as a bridge to lung transplantation. J. Thorac. Cardiovasc. Surg. 2013 , 145 , 1065–1070. [ Google Scholar ] [ CrossRef ]
- Lafarge, M.; Mordant, P.; Thabut, G.; Brouchet, L.; Falcoz, P.-E.; Haloun, A.; Le Pimpec-Barthes, F.; Maury, J.-M.; Reynaud-Gaubert, M.; Saint-Raymond, C.; et al. Experience of extracorporeal membrane oxygenation as a bridge to lung transplantation in France. J. Heart Lung Transplant. 2013 , 32 , 905–913. [ Google Scholar ] [ CrossRef ]
- Lang, G.; Kim, D.; Aigner, C.; Matila, J.; Taghavi, S.; Jaksch, P.; Murakoezi, G.; Klepetko, W. Awake extracorporeal membrane oxygenation bridging for pulmonary retransplantation provides comparable results to elective retransplantation. J. Heart Lung Transplant. 2014 , 14 , 1224–1228. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Dellgren, G.; Riise, G.C.; Swärd, K.; Gilljam, M.; Rexius, H.; Liden, H.; Silverborn, M. Extracorporeal membrane oxygenation as a bridge to lung transplantation: A long-term study. Eur. J. Cardiothorac. Surg. 2015 , 47 , 95–100. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Hayanga, A.J.; Aboagye, J.; Esper, S.; Shigemura, N.; Bermudez, C.A.; Cunha, J.D.; Bhama, J. Extracorporeal membrane oxygenation as a bridge to lung transplantation in the United States: An evolving strategy in the management of rapidly advancing pulmonary disease. J. Thorac. Cardiovasc. Surg. 2015 , 149 , 291–296. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Hayes, D., Jr.; Tobias, J.D.; Tumin, D. Center Volume and Extracorporeal Membrane Oxygenation Support at Lung Transplantation in the Lung Allocation Score Era. Am. J. Respir. Crit. Care Med. 2016 , 194 , 317–326. [ Google Scholar ] [ CrossRef ]
- Schechter, M.A.; Ganapathi, A.M.; Englum, B.R.; Speicher, P.J.; Daneshmand, M.A.; Davis, R.D.; Hartwig, M.G. Spontaneously Breathing Extracorporeal Membrane Oxygenation Support Provides the Optimal Bridge to Lung Transplantation. Transplantation 2016 , 100 , 2699–2704. [ Google Scholar ] [ CrossRef ]
- Yeo, H.J.; Lee, S.; Yoon, S.H.; Lee, S.E.; Cho, W.H.; Jeon, D.; Kim, Y.S.; Kim, D. Extracorporeal Life Support as a Bridge to Lung Transplantation in Patients with Acute Respiratory Failure. Transplant. Proc. 2017 , 49 , 1430–1435. [ Google Scholar ] [ CrossRef ]
- Tsiouris, A.; Budev, M.M.; Yun, J.J. Extracorporeal Membrane Oxygenation as a Bridge to Lung Transplantation in the United States: A Multicenter Survey. ASAIO 2018 , 64 , 689–693. [ Google Scholar ] [ CrossRef ]
- Tudorache, I.; Sommer, W.; Kühn, C.; Wiesner, O.; Hadem, J.; Fühner, T.; Ius, F.; Avsar, M.; Schwerk, N.; Böthig, D.; et al. Lung Transplantation for Severe Pulmonary Hypertension–Awake Extracorporeal Membrane Oxygenation for Postoperative Left Ventricular Remodeling. Transplantation 2015 , 99 , 451–458. [ Google Scholar ] [ CrossRef ]
- Salman, J.; Ius, F.; Sommer, W.; Siemeni, T.; Kuehn, C.; Avsar, M.; Boethig, D.; Molitoris, U.; Bara, C.; Gottlieb, J.; et al. Mid-term results of bilateral lung transplant with postoperatively extended intraoperative extracorporeal membrane oxygenation for severe pulmonary hypertension. Eur. J. Cardiothorac. Surg. 2017 , 52 , 163–170. [ Google Scholar ] [ CrossRef ]
- Turner, D.A.; Cheifetz, I.M.; Rehder, K.J.; Williford, W.L.; Bonadonna, D.; Banuelos, S.J.; Peterson-Carmichael, S.; Lin, S.S.; Davis, R.D.; Zaas, D. Active rehabilitation and physical therapy during extracorporeal membrane oxygenation while awaiting lung transplantation: A practical approach. Crit. Care Med. 2011 , 39 , 2593–2598. [ Google Scholar ] [ CrossRef ]
- Rahimi, R.A.; Skrzat, J.; Reddy, D.R.S.; Zanni, J.M.; Fan, E.; Stephens, R.S.; Needham, D.M. Physical Rehabilitation of Patients in the Intensive Care Unit Requiring Extracorporeal Membrane Oxygenation: A Small Case Series. Phys. Ther. 2013 , 93 , 248–255. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Hayes, K.; Hodgson, C.L.; Pellegrino, V.A.; Snell, G.; Tarrant, B.; Fuller, L.M.; Holland, A.E. Physical Function in Subjects Requiring Extracorporeal Membrane Oxygenation Before or After Lung Transplantation. Respir. Care 2018 , 63 , 194–202. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Kolaitis, N.A.; Soong, A.; Shrestha, P.; Zhuo, H.; Neuhaus, J.; Katz, P.P.; Greenland, J.R.; Golden, J.; Leard, L.E.; Shah, R.J.; et al. Improvement in patient-reported outcomes after lung transplantation is not impacted by the use of extracorporeal membrane oxygenation as a bridge to transplantation. J. Thorac. Cardiovasc. Surg. 2018 , 156 , 440–448. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Capoccia, M.; Brewer, J.M.; Rackauskas, M.; Becker, T.K.; Maybauer, D.M.; Stukov, Y.; Lorusso, R.; Maybauer, M.O. Outcome of Veno-Pulmonary Extracorporeal Life Support in Lung Transplantation Using ProtekDuo Cannula: A Systematic Review and Description of Configurations. J. Clin. Med. 2024 , 13 , 4111. [ Google Scholar ] [ CrossRef ]
- Saeed, O.; Stein, L.H.; Cavarocchi, N.; Tatooles, A.J.; Mustafa, A.; Jorde, U.P.; Alvarez, C.; Gluck, J.; Saunders, P.; Abrol, S.; et al. Outcomes by cannulation methods for venovenous extracorporeal membrane oxygenation during COVID-19: A multicenter retrospective study. Artif. Organs. 2022 , 46 , 1659–1668. [ Google Scholar ] [ CrossRef ]
- Bermudez, C.A.; Shiose, A.; Esper, S.A.; Shigemura, N.; D’cunha, J.; Bhama, J.K.; Richards, T.J.; Arlia, P.; Crespo, M.M.; Pilewski, J.M. Outcomes of Intraoperative Venoarterial Extracorporeal Membrane Oxygenation Versus Cardiopulmonary Bypass During Lung Transplantation. Ann. Thorac. Surg. 2014 , 98 , 1936–1943. [ Google Scholar ] [ CrossRef ]
- Biscotti, M.; Yang, J.; Sonett, J.; Bacchetta, M. Comparison of extracorporeal membrane versus cardiopulmonary bypass for lung transplantation. J. Thorac. Cardiovasc. Surg. 2014 , 148 , 2410–2416. [ Google Scholar ] [ CrossRef ]
- Machuca, T.N.; Collaud, S.; Mercier, O.; Cheung, M.; Cunningham, V.; Kim, S.J.; Azad, S.; Singer, L.; Yasufuku, K.; de Perrot, M.; et al. Outcomes of intraoperative extracorporeal membrane oxygenation versus cardiopulmonary bypass for lung transplantation. J. Thorac. Cardiovasc. Surg. 2015 , 149 , 1152–1157. [ Google Scholar ] [ CrossRef ]
- Winter, H.; Müller, H.-H.; Meiser, B.; Neurohr, C.; Behr, J.; Guenther, S.; Hagl, C.; Hoechter, D.J.; von Dossow, V.; Schramm, R. The Munich Lung Transplant Group: Intraoperative Extracorporeal Circulation in Lung Transplantation. Thorac. Cardiovasc. Surg. 2015 , 63 , 706–714. [ Google Scholar ] [ CrossRef ]
- Pettenuzzo, T.; Faggi, G.; Di Gregorio, G.; Schiavon, M.; Marulli, G.; Gregori, D.; Rea, F.; Ori, C.; Feltracco, P. Blood Products Transfusion and Mid-Term Outcomes of Lung Transplanted Patients Under Extracorporeal Membrane Oxygenation Support. Prog. Transplant. 2018 , 28 , 314–321. [ Google Scholar ] [ CrossRef ]
- Hoetzenecker, K.; Schwarz, S.; Muckenhuber, M.; Benazzo, A.; Frommlet, F.; Schweiger, T.; Bata, O.; Jaksch, P.; Ahmadi, N.; Muraközy, G.; et al. Intraoperative extracorporeal membrane oxygenation and the possibility of postoperative prolongation improve survival in bilateral lung transplantation. J. Thorac. Cardiovasc. Surg. 2018 , 155 , 2193–2206. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Yu, W.S.; Paik, H.C.; Haam, S.J.; Lee, C.Y.; Nam, K.S.; Jung, H.S.; Do, Y.W.; Shu, J.W.; Lee, J.G. Transition to routine use of venoarterial extracorporeal oxygenation during lung transplantation could improve early outcomes. J. Thorac. Dis. 2016 , 8 , 1712–1720. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Cosgun, T.; Tomaszek, S.; Opitz, I.; Wilhelm, M.; Schuurmans, M.M.; Weder, W.; Inci, I. Single-center experience with intraoperative extracorporeal membrane oxygenation use in lung transplantation. Int. J. Artif. Organs , 2017; epub ahead of print . [ Google Scholar ] [ CrossRef ]
- Magouliotis, D.E.; Tasiopoulou, V.S.; Svokos, A.A.; Svokos, A.A.; Zacharoulis, D. Extracorporeal membrane oxygenation versus cardiopulmonary bypass during lung transplantation: A meta-analysis. Gen. Thorac. Cardiovasc. Surg. 2018 , 66 , 38–47. [ Google Scholar ] [ CrossRef ]
- Hoechter, D.J.; Shen, Y.-M.; Kammerer, T.; Günther, S.; Weig, T.; Schramm, R.; Hagl, C.; Born, F.; Meiser, B.; Preissler, G.; et al. Extracorporeal Circulation During Lung Transplantation Procedures: A meta-Analysis. ASAIO J. 2017 , 63 , 551–561. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Ius, F.; Sommer, W.; Tudorache, I.; Avsar, M.; Siemeni, T.; Salman, J.; Molitoris, U.; Gras, C.; Juettner, B.; Puntigam, J.; et al. Five-year experience with intraoperative extracorporeal membrane oxygenation in lung transplantation: Indications and midterm results. J. Heart Lung Transplant. 2016 , 35 , 39–58. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Ius, F.; Aburahma, K.; Boethig, D.; Salman, J.; Sommer, W.; Draeger, H.; Poyanmehr, R.; Avsar, M.; Siemeni, T.; Bobylev, D.; et al. Long-term outcomes after intraoperative extracorporeal membrane oxygenation during lung transplantation. J. Heart Lung Transplant. 2020 , 39 , 915–925. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Franz, M.; Siemeni, T.; Aburahma, K.; Yablonski, P.; Poyanmehr, R.; Avsar, M.; Bobylev, D.; Sommer, W.; Boethig, D.; Greer, M.; et al. Lung transplant and severe coronary artery disease: Results from a single-centre experience. Eur. J. Cardiothorac. Surg. 2022 , 62 , ezac348. [ Google Scholar ] [ CrossRef ]
- Hartwig, M.G.; Walczak, R.; Lin, S.S.; Davis, R.D. Improved Survival but Marginal Allograft Function in Patients Treated with Extracorporeal Membrane Oxygenation after Lung Transplantation. Ann. Thorac. Surg. 2012 , 93 , 366–371. [ Google Scholar ] [ CrossRef ]
- Vlasselaers, D.; Verleden, G.M.; Meyns, B.; Van Raemdonck, D.; Demedts, M.; Lerut, A.; Lauwers, P. Femoral Venoarterial Extracorporeal Membrane Oxygenation for Severe Reimplantation Response After Lung Transplantation. Chest 2000 , 118 , 559–561. [ Google Scholar ] [ CrossRef ]
- Dahlberg, P.S.; Prekker, M.E.; Herrington, C.S.; Hertz, M.I.; Park, S.J. Medium-Term Results of Extracorporeal Membrane Oxygenation for Severe Acute Lung Injury After Lung Transplantation. J. Heart Lung Transplant. 2004 , 23 , 979–984. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Oto, T.; Rosenfeldt, F.; Rowland, M.; Pick, A.; Rabinov, M.; Preovolos, A.; Snell, G.; Williams, T.; Esmore, D. Extracorporeal Membrane Oxygenation After Lung Transplantation: Evolving Technique Improves Outcomes. Ann. Thorac. Surg. 2004 , 78 , 1230–1235. [ Google Scholar ] [ CrossRef ]
- Mason, D.P.; Boffa, D.J.; Murthy, S.C.; Gildea, T.R.; Budev, M.M.; Mehta, A.C.; McNeill, A.M.; Smedira, N.G.; Feng, J.; Rice, T.W.; et al. Extended use of extracorporeal membrane oxygenation after lung transplantation. J. Thorac. Cardiovasc. Surg. 2006 , 132 , 954–960. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Fischer, S.; Bohn, D.; Rycus, P.; Pierre, A.F.; de Perrot, M.; Waddell, T.K.; Keshavjee, S. Extracorporeal membrane Oxygenation for Primary Graft Dysfunction After Lung Transplantation: Analysis of the Extracorporeal Life Support Organization (ELSO) Registry. J. Heart Lung Transplant. 2007 , 26 , 472–477. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Bermudez, C.A.; Adusumilli, P.S.; McCurry, K.R.; Zaldonis, D.; Crespo, M.M.; Pilewski, J.M.; Toyoda, Y. Extracorporeal Membrane Oxygenation for Primary Graft Dysfunction After Lung Transplantation: Long-Term Survival. Ann. Thorac. Surg. 2009 , 87 , 854–860. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Marasco, S.F.; Vale, M.; Preovolos, A.; Pellegrino, V.; Lee, G.; Snell, G.; Williams, T. Institution of extracorporeal membrane oxygenation late after lung transplantation—A futile exercise? Clin. Transplant. 2012 , 26 , E71–E77. [ Google Scholar ] [ CrossRef ]
- Mulvihill, M.S.; Yerokun, B.A.; Davis, R.P.; Renney, D.N.; Daneshmand, M.A.; Hartwig, M. Extracorporeal membrane oxygenation following lung transplantation: Indications and survival. J. Heart Lung Transplant. 2018 , 37 , 259–267. [ Google Scholar ] [ CrossRef ]
- Moser, B.; Jaksch, P.; Taghavi, S.; Muraközy, G.; Lang, G.; Hager, H.; Krenn, C.; Roth, G.; Faybik, P.; Bacher, A.; et al. Lung transplantation for idiopathic pulmonary arterial hypertension on intraoperative and postoperatively prolonged extracorporeal membrane oxygenation provides optimally controlled reperfusion and excellent outcome. Eur. J. Cardiothorac. Surg. 2018 , 53 , 178–185. [ Google Scholar ] [ CrossRef ]
- Terasaki, P.I. Humoral theory of transplantation. Am. J. Transplant. 2003 , 3 , 665–673. [ Google Scholar ] [ CrossRef ]
- Campbell, P. Clinical relevance of human leukocyte antigen antibodies in liver, heart, lung and intestine transplantation. Curr. Opin. Organ. Transplant. 2013 , 18 , 463–469. [ Google Scholar ] [ CrossRef ]
- Jordan, S.C.; Vo, A.A. Donor-specific antibodies in allograft recipients: Etiology, impact and therapeutic approaches. Curr. Opin. Organ. Transplant. 2014 , 19 , 591–597. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Loupy, A.; Lefaucheur, C. Antibody-mediated rejection of solid-organ allografts. N. Engl. J. Med. 2018 , 379 , 1150–1160. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Nguyen, V.P.; Kobashigawa, J.A. Antibody-medicated rejection after heart transplantation: Diagnosis and clinical implications. Curr. Opin. Organ. Transplant. 2020 , 25 , 248–254. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Stewart, S.; Fishbein, M.C.; Snell, G.I.; Berry, G.J.; Boehler, A.; Burke, M.M.; Glanville, A.; Gould, F.K.; Magro, C.; Marboe, C.C.; et al. Revision of the 1996 working formulation for the standardization of nomenclature in the diagnosis of lung rejection. J. Heart Lung Transplant. 2007 , 26 , 1229–1242. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Roden, A.C.; Aisner, D.L.; Allen, T.C.; Aubry, M.C.; Barrios, R.J.; Beasley, M.B.; Cagle, P.T.; Capelozzi, V.L.; Dacic, S.; Ge, Y.; et al. Diagnosis of Acute Cellular Rejection and Antibody-Mediated Rejection on Lung Transplant Biopsies: A Perspective From Members of the Pulmonary Pathology Society. Arch. Pathol. Lab. Med. 2017 , 141 , 437–444. [ Google Scholar ] [ CrossRef ]
- Levine, D.J.; Glanville, A.R.; Aboyoun, C.; Belperio, J.; Benden, C.; Berry, G.J.; Hachem, R.; Hayes, D.; Neil, D.; Reinsmoen, N.L.; et al. Antibody-mediated rejection of the lung: A consensus report of the International Society for Heart and Lung Transplantation. J. Heart Lung Transplant. 2016 , 35 , 397–406. [ Google Scholar ] [ CrossRef ]
- Tambur, A.R.; Campbell, P.; Chong, A.S.; Feng, S.; Ford, M.L.; Gebel, H.; Gill, R.G.; Kelsoe, G.; Kosmoliaptsis, V.; Mannon, R.B.; et al. Sensitization in Transplantation: Assessment of Risk (STAR) 2017 Working Group Meeting Report. Am. J. Transplant. 2018 , 18 , 1604–1614. [ Google Scholar ] [ CrossRef ]
- Roux, A.; Levine, D.; Zeevi, A.; Hachem, R.; Halloran, K.; Halloran, P.; Gibault, L.; Taupin, J.; Neil, D.; Loupy, A.; et al. Banff lung report: Current knowledge and future research perspectives for diagnosis and treatment of pulmonary antibody-mediated rejection (AMR). Am. J. Transplant. 2019 , 19 , 21–31. [ Google Scholar ] [ CrossRef ]
- Pavlisko, E.N.; Adam, B.A.; Berry, G.J.; Calabrese, F.; Cortes-Santiago, N.; Glass, C.H.; Goddard, M.; Greenland, J.R.; Kreisel, D.; Levine, D.J.; et al. The 2022 Banff Meeting Lung Report. Am. J. Transplant. 2024 , 24 , 542–548. [ Google Scholar ] [ CrossRef ]
- Chong, A.S. B cells as antigen-presenting cells in transplantation rejection and tolerance. Cell Immunol. 2020 , 349 , 104061. [ Google Scholar ] [ CrossRef ]
- Reinsmoen, N.L.; Mirocha, J.; Ensor, C.R.; Marrari, M.; Chaux, G.; Levine, D.J.; Zhang, X.; Zeevi, A. A 3-center study reveals new insights into the impact of non-HLA antibodies on lung transplantation outcome. Transplantation 2017 , 101 , 1215–1221. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Rao, U.; Mohanakumar, T.; Ahn, C.; Gao, A.; Kaza, V. Prevalence of antibodies to lung self-antigens (Kalpha1 tubulin and collagen V) and donor specific antibodies to HLA in lung transplant recipients and implications for lung transplant outcomes: Single center experience. Transpl. Immunol. 2019 , 54 , 65–72. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Xu, Q.; Elrefaei, M.; Taupin, J.-L.; Hitchman, K.M.; Hiho, S.; Gareau, A.J.; Iasella, C.J.; Marrari, M.; Belousova, N.; Bettinotti, M.; et al. Chronic lung allograft dysfunction is associated with an increased number of non-HLA antibodies. J. Heart Lung Transplant. 2024 , 43 , 663–672. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Hachem, R.R. The impact of non-HLA antibodies on outcomes after lung transplantation and implications for therapeutic approaches. Hum. Immunol. 2019 , 80 , 583–587. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Zhang, X.; Reinsmoen, N.L. Impact and production of non-HLA-specific antibodies in solid organ transplantation. Int. J. Immunogenet. 2020 , 47 , 235–242. [ Google Scholar ] [ CrossRef ]
- Kardol-Hoefnagel, T.; Otten, H.G. A comprehensive overview of the clinical relevance and treatment options for antibody-mediated rejection with non-HLA antibodies. Transplantation 2021 , 105 , 1459–1470. [ Google Scholar ] [ CrossRef ]
- Scornik, J.C.; Zander, D.S.; Baz, M.A.; Donnelly, W.H.; Staples, E.D. Susceptibility of lung transplants to preformed donor-specific HLA antibodies as detected by flow cytometry. Transplantation 1999 , 68 , 1542–1546. [ Google Scholar ] [ CrossRef ]
- Hadjiliadis, D.; Chaparro, C.; Reinsmoen, N.L.; Gutierrez, C.; Singer, L.G.; Steele, M.P.; Waddell, T.K.; Davis, R.D.; Hutcheon, M.A.; Palmer, S.M.; et al. Pre-transplant panel reactive antibody in lung transplant recipients is associated with significantly worse post-transplant survival in a multicenter study. J. Heart Lung Transplant. 2005 , 24 , S249–S254. [ Google Scholar ] [ CrossRef ]
- Masson, E.; Chabod, M.S.J.; Thevenin, C.; Gonin, F.; Rebibou, J.M.; Tiberghien, P. Hyperacute rejection after lung transplantation caused by undetected low-titer anti-HLA antibodies. J. Heart Lung Transplant. 2007 , 26 , 642–645. [ Google Scholar ] [ CrossRef ]
- Shah, A.S.; Nwakanma, L.; Simpkins, C.; Williams, J.; Chang, D.C.; Conte, J.V. Pretransplant panel reactive antibodies in human lung transplantation: An analysis of over 10,000 patients. Ann. Thorac. Surg. 2008 , 85 , 1919–1924. [ Google Scholar ] [ CrossRef ]
- Lachmann, N.; Todorova, K.; Schulze, H.; Schönemann, C. Luminex ® and its applications for solid organ transplantation, hematopoietic stem cell transplantation, and transfusion. Transfus. Med. Hemother. 2013 , 40 , 182–189. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Brugière, O.; Roux, A.; Le Pavec, J.; Sroussi, D.; Parquin, F.; Pradère, P.; Dupin, C.; Bunel, V.; Mourin, G.; Jebrak, G.; et al. Role of C1q-binding anti-HLA antibodies as a predictor of lung allograft outcome. Eur. Respir. J. 2018 , 52 , 1701898. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Iasella, C.J.; Ensor, C.R.; Marrari, M.; Mangiola, M.; Xu, Q.; Nolley, E.; Moore, C.A.; Morrell, M.R.; Pilewski, J.M.; Sanchez, P.G.; et al. Donor-specific antibody characteristics, including persistence and complement-binding capacity, increase risk for chronic lung allograft dysfunction. J. Heart Lung Transplant. 2020 , 39 , 1417–1425. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Brugière, O.; Suberbielle, C.; Thabut, G.; Lhuillier, E.; Dauriat, G.; Metivier, A.-C.; Gautreau, C.; Charron, D.; Mal, H.; Parquin, F.; et al. Lung transplantation in patients with pretransplantation donor-specific antibodies detected by Luminex assay. Transplantation 2013 , 95 , 761–765. [ Google Scholar ] [ CrossRef ]
- Girnita, A.L.; McCurry, K.R.; Iacono, A.T.; Duquesnoy, R.; Corcoran, T.E.; Awad, M.; Spichty, K.J.; Yousem, S.A.; Burckart, G.; Dauber, J.H.; et al. HLA-specific antibodies are associated with high-grade and persistent-recurrent lung allograft acute rejection. J. Heart Lung Transplant. 2004 , 23 , 1135–1141. [ Google Scholar ] [ CrossRef ]
- Hachem, R.R.; Yusen, R.D.; Meyers, B.F.; Aloush, A.A.; Mohanakumar, T.; Patterson, G.A.; Trulock, E.P. Anti-HLA antibodies and pre-emptive antibody-directed therapy after lung transplantation. J. Heart Lung Transplant. 2010 , 29 , 973–980. [ Google Scholar ] [ CrossRef ]
- Snyder, L.D.; Wang, Z.; Chen, D.-F.; Reinsmoen, N.L.; Finlen-Copeland, C.A.; Davis, W.A.; Zaas, D.W.; Palmer, S.M. Implications for human leukocyte antigen antibodies after lung transplantation. A 10-year experience in 441 patients. Chest 2013 , 144 , 226–233. [ Google Scholar ] [ CrossRef ]
- Lobo, L.J.; Aris, R.M.; Schmitz, J.; Neuringer, I.P. Donor-specific antibodies are associated with antibody-mediated rejection, acute cellular rejection, bronchiolitis obliterans syndrome, and cystic fibrosis after lung transplantation. J. Heart Lung Transplant. 2013 , 32 , 70–77. [ Google Scholar ] [ CrossRef ]
- Witt, C.A.; Gaut, J.P.; Yusen, R.D.; Byers, D.E.; Iuppa, J.A.; Bain, K.B.; Patterson, G.A.; Mohanakumar, T.; Trulock, E.P.; Hachem, R.R. Acute Antibody-Mediated Rejection After Lung Transplantation: A Retrospective, Single Center, Case Series. J. Heart Lung Transplant. 2013 , 32 , 1034–1040. [ Google Scholar ] [ CrossRef ]
- Smith, J.D.; Ibrahim, M.W.; Newell, H.; Danskine, A.J.; Soresi, S.; Burke, M.M.; Rose, M.L.; Carby, M. Pre-transplant donor HLA-specific antibodies: Characteristics causing detrimental effects on survival after lung transplantation. J. Heart Lung Transplant. 2014 , 33 , 1074–1082. [ Google Scholar ] [ CrossRef ]
- Kim, M.; Townsend, K.R.; Wood, I.G.; Boukedes, S.; Guleria, I.; Gabardi, S.; El-Chemaly, S.; Camp, P.C.; Chandraker, A.K.; Milford, E.L.; et al. Impact of pretransplant anti-HLA antibodies on outcomes in lung transplant candidates. Am. J. Respir. Crit. Care Med. 2014 , 189 , 1234–1239. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Morrell, M.R.; Pilewski, J.M.; Gries, C.J.; Pipeling, M.R.; Crespo, M.M.; Ensor, C.R.; Yousem, S.A.; D’cunha, J.; Shigemura, N.; Bermudez, C.A.; et al. De novo donor-specific HLA antibodies are associated with early and high-grade bronchiolitis obliterans syndrome and death after lung transplantation. J. Heart Lung Transplant. 2014 , 33 , 1288–1294. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Safavi, S.; Robinson, D.R.; Soresi, S.; Carby, M.; Smith, J.D. De novo donor HLA-specific antibodies predict development of bronchiolitis obliterans syndrome after lung transplantation. J. Heart Lung Transplant. 2014 , 33 , 1273–1281. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Bosanquet, J.P.; Witt, C.A.; Bemiss, B.C.; Byers, D.E.; Yusen, R.D.; Patterson, A.G.; Kreisel, D.; Mohanakumar, T.; Trulock, E.P.; Hachem, R.R. The impact of pre-transplant allosensitization on outcomes after lung transplantation. J. Heart Lung Transplant. 2015 , 34 , 1415–1422. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Roux, A.; Le Lan, I.B.; Holifanjaniaina, S.; Thomas, K.A.; Hamid, A.M.; Picard, C.; Grenet, D.; De Miranda, S.; Douvry, B.; Foch Lung Transplantation Group; et al. Antibody-Mediated Rejection in Lung Transplantation: Clinical Outcomes and Donor-Specific Antibody Characteristics. Am. J. Transplant. 2016 , 16 , 1216–1228. [ Google Scholar ] [ CrossRef ]
- Visentin, J.; Chartier, A.; Massara, L.; Linares, G.; Guidicelli, G.; Blanchard, E.; Parrens, M.; Begueret, H.; Dromer, C.; Taupin, J.-L. Lung intragraft donor-specific antibodies as a risk factor for graft loss. J. Heart Lung Transplant. 2016 , 35 , 1418–1426. [ Google Scholar ] [ CrossRef ]
- Ius, F.; Sommer, W.; Tudorache, I.; Kühn, C.; Avsar, M.; Siemeni, T.; Salman, J.; Hallensleben, M.; Kieneke, D.; Greer, M.; et al. Early-donor-specific antibodies in lung transplantation: Risk factors and impact on survival. J. Heart Lung Transplant. 2014 , 33 , 1255–1263. [ Google Scholar ] [ CrossRef ]
- Le Pavec, J.; Suberbielle, C.; Lamrani, L.; Feuillet, S.; Savale, L.; Dorfmüller, P.; Stephan, F.; Mussot, S.; Mercier, O.; Fadel, E. De-novo donor-specific anti-HLA antibodies 30 days after lung transplantation are associated with worse outcomes. J. Heart Lung Transplant. 2016 , 35 , 1067–1077. [ Google Scholar ] [ CrossRef ]
- Tikkanen, J.M.; Singer, L.G.; Kim, S.J.; Li, Y.; Binnie, M.; Chaparro, C.; Chow, C.-W.; Martinu, T.; Azad, S.; Keshavjee, S.; et al. De Novo DQ Donor-Specific Antibodies Are Associated with Chronic Lung Allograft Dysfunction after Lung Transplantation. Am. J. Respir. Crit. Care Med. 2016 , 194 , 596–606. [ Google Scholar ] [ CrossRef ]
- Zazueta, O.E.; Preston, S.E.; Moniodis, A.; Fried, S.; Kim, M.; Townsend, K.; Wood, I.; Boukedes, S.; Guleria, I.; Camp, P.; et al. The presence of pretransplant HLA antibodies does not impact the development of chronic lung allograft dysfunction or CLAD-related death. Transplantation 2017 , 101 , 2207–2212. [ Google Scholar ] [ CrossRef ]
- Verleden, S.E.; Vanaudenaerde, B.M.; Emonds, M.-P.; Van Raemdonck, D.E.; Neyrinck, A.P.; Verleden, G.M.; Vos, R. Donor-specific and –nonspecific HLA antibodies and outcome post lung transplantation. Eur. Respir. J. 2017 , 50 , 1701248. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Schmitzer, M.; Winter, H.; Kneidinger, N.; Meimarakis, G.; Dick, A.; Schramm, R.; Klotz, L.V.; Preissler, G.; Strobl, N.; von Dossow, V.; et al. Persistence of de novo donor-specific HLA-antibodies after lung transplantation: A potential marker of decreased patient survival. HLA 2018 , 92 , 24–32. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Courtwright, A.M.; Cao, S.; Wood, I.; Mallidi, H.R.; Kawasawa, J.; Moniodis, A.; Ng, J.; El-Chemaly, S.; Goldberg, H.J. Clinical outcomes of lung transplantation in the presence of donor-specific antibodies. Ann. Am. Thorac. Soc. 2019 , 16 , 1131–1137. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Keller, M.; Yang, S.; Ponor, L.; Bon, A.; Cochrane, A.; Philogene, M.; Bush, E.; Shah, P.; Matthews, J.; Brown, A.W.; et al. Preemptive treatment of de novo donor-specific antibodies in lung transplant patients reduces subsequent risk of chronic lung allograft dysfunction or death. Am. J. Transplant. 2023 , 23 , 559–564. [ Google Scholar ] [ CrossRef ]
- Hachem, R.R.; Kamoun, M.; Budev, M.M.; Askar, M.; Ahya, V.N.; Lee, J.C.; Levine, D.J.; Pollack, M.S.; Dhillon, G.S.; Weill, D.; et al. Human Leukocyte antigens antibodies after lung transplantation: Primary results of the HALT study. Am. J. Transplant. 2018 , 37 , 1119–1130. [ Google Scholar ] [ CrossRef ]
- Bouquegneau, A.; Loheac, C.; Aubert, O.; Bouatou, Y.; Viglietti, D.; Empana, J.P.; Ulloa, C.; Hassan Murad, M.; Legendre, C.; Glotz, D.; et al. Complement-activating donor-specific anti-HLA antibodies and solid organ transplant survival: A systematic review and meta-analysis. PLoS Med. 2018 , 15 , e1002572. [ Google Scholar ]
- Roux, A.; Thomas, K.A.; Sage, E.; Suberbielle-Boissel, C.; Beaumont-Azuar, L.; Parquin, F.; Le Guen, M.; Harre, N.; Hamid, A.M.; Reed, E.F. Donor-specific HLA antibody-mediated complement activation is a significant indicator of antibody-mediated rejection and poor long-term graft outcome during lung transplantation: A single center cohort study. Transpl. Int. 2018 , 31 , 761–772. [ Google Scholar ] [ CrossRef ]
- Miyamoto, E.; Motoyama, H.; Sato, M.; Aoyama, A.; Menju, T.; Shikuma, K.; Sowa, T.; Yoshizawa, A.; Saito, M.; Takahagi, A.; et al. Association of local intrapulmonary production of antibodies specific to donor major histocompatibility complex class I with the progression of chronic rejection of lung allografts. Transplantation 2017 , 101 , e156–e165. [ Google Scholar ] [ CrossRef ]
- Sacreas, A.; Taupin, J.L.; Emonds, M.P.; Daniëls, L.; Van Raemdonck, D.E.; Vos, R.; Verleden, G.M.; Vanaudenaerde, B.M.; Roux, A.; Verleden, S.E. Intragraft donor-specific anti-HLA antibodies in phenotypes of chronic lung allograft dysfunction. Eur. Respir. J. 2019 , 54 , 1900847. [ Google Scholar ] [ CrossRef ]
- Berry, G.; Burke, M.; Andersen, C.; Angelini, A.; Bruneval, P.; Calabrese, F.; Fishbein, M.C.; Goddard, M.; Leone, O.; Maleszewski, J.; et al. Pathology of pulmonary antibody-mediated rejection: 2012 update from the Pathology Council of the ISHLT. J. Heart Lung Transplant. 2013 , 32 , 14–21. [ Google Scholar ] [ CrossRef ]
- Kataria, A.; Kumar, D.; Gupta, G. Donor-derived Cell-free DNA in Solid Organ Transplant Diagnostics: Indications, Limitations, and Future Directions. Transplantation 2021 , 105 , 1203–1211. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Keller, M.; Agbor-Enoh, S. Cell-free DNA in lung transplantation: Research tool or clinical workhorse? Curr. Opin. Organ. Transplant. 2022 , 27 , 177–183. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Kauke, T.; Kneidinger, N.; Martin, B.; Dick, A.; Schneider, C.; Schramm, R.; Meimarakis, G.; Preissler, G.; Eickelberg, O.; Von Dossow, V.; et al. Bronchiolitis obliterans syndrome due to donor-specific HLA antibodies. Tissue Antigens 2015 , 86 , 178–185. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Westall, G.P.; Snell, G.I. Antibody-mediated rejection in lung transplantation: Fable, spin, or fact? Transplantation 2014 , 98 , 927–930. [ Google Scholar ] [ CrossRef ]
- Chong, A.S. Mechanisms of organ transplant injury mediated by B cells and antibodies: Implications for antibody-mediated rejection. Am. J. Transplant. 2020 , 20 , 23–32. [ Google Scholar ] [ CrossRef ]
- Hulbert, A.L.; Pavlisko, E.N.; Palmer, S.M. Current challenges and opportunities in the management of antibody-mediated rejection in lung transplantation. Curr. Opin. Organ. Transplant. 2018 , 23 , 308–315. [ Google Scholar ] [ CrossRef ]
- Habal, M.V.; Farr, M.; Restaino, S.; Chong, A. Desensitization in the era of precision medicine: Moving from the bench to bedside. Transplantation 2019 , 103 , 1574–1581. [ Google Scholar ] [ CrossRef ]
- Wan, S.S.; Ying, T.D.; Wyburn, K.; Roberts, D.M.; Wyld, M.; Chadban, S.J. The treatment of antibody-mediated rejection in kidney transplantation: An updated systematic review and meta-analysis. Transplantation 2018 , 102 , 557–568. [ Google Scholar ] [ CrossRef ]
- Jordan, S.C.; Ammerman, N.; Choi, J.; Kumar, S.; Huang, E.; Toyoda, M.; Kim, I.; Wu, G.; Vo, A. Interleukin-6: An important mediator of allograft injury. Transplantation 2020 , 104 , 2497–2506. [ Google Scholar ] [ CrossRef ]
- Suchanek, O.; Clatworthy, M.R. Novel strategies to target the humoral alloimmune response. HLA 2020 , 96 , 667–680. [ Google Scholar ] [ CrossRef ]
- Schinstock, C.A.; Mannon, R.B.; Budde, K.; Chong, A.S.; Haas, M.; Knechtle, S.; Lefaucheur, C.; Montgomery, R.A.; Nickerson, P.; Tullius, S.G.; et al. Recommended treatment for antibody-mediated rejection after kidney transplantation: The 2019 expert consensus from the Transplantation Society Working Group. Transplantation 2020 , 104 , 911–922. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Nickerson, P.W. What have we learned about how to prevent and treat antibody-mediated rejection in kidney transplantation? Am. J. Transplant. 2020 , 20 , 12–22. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Mayer, K.A.; Doberer, K.; Eskandary, F.; Halloran, P.F.; Böhmig, G.A. New concepts in chronic antibody-mediated rejection: Prevention and treatment. Curr. Opin. Organ. Transplant. 2021 , 26 , 97–105. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Vo, A.A.; Choi, J.; Kim, I.; Louie, S.; Cisneros, K.; Kahwaji, J.; Toyoda, M.; Ge, S.; Haas, M.; Puliyanda, D.; et al. A phase I/II trial of the interleukin-6 receptor specific humanized monoclonal (Tocilizumab) + intravenous immunoglobulin in difficult to desensitize patients. Transplantation 2015 , 99 , 2356–2363. [ Google Scholar ] [ CrossRef ]
- Choi, J.; Aubert, O.; Vo, A.; Loupy, A.; Haas, M.; Puliyanda, D.; Kim, I.; Louie, S.; Kang, A.; Peng, A.; et al. Assessment of Tocilizumab (anti-interleukin-6 receptor monoclonal) as a potential treatment for chronic antibody-mediated rejection and transplant glomerulopathy in HLA-sensitized renal allograft recipients. Am. J. Transplant. 2017 , 17 , 2381–2389. [ Google Scholar ] [ CrossRef ]
- Pottebaum, A.A.; Venkatachalam, K.; Liu, C.; Brennan, D.C.; Murad, H.; Malone, A.F.; Alhamad, T. Efficacy and safety of Tocilizumab in the treatment of acute active antibody-mediated rejection in kidney transplant recipients. Transplant. Direct 2020 , 6 , e543. [ Google Scholar ] [ CrossRef ]
- Lavacca, A.; Presta, R.; Gai, C.; Mella, A.; Gallo, E.; Camussi, G.; Abbasciano, I.; Barreca, A.; Caorsi, C.; Fop, F.; et al. Early effects of first-line treatment with anti-interleukin-6 receptor antibody tocilizumab for chronic active antibody-mediated rejection in kidney transplantation. Clin. Transplant. 2020 , 34 , e13908. [ Google Scholar ] [ CrossRef ]
- Shin, B.H.; Everly, M.J.; Zhang, H.; Choi, J.; Vo, A.; Zhang, X.; Huang, E.; Jordan, S.C.; Toyoda, M. Impact of Tocilizumab (anti-IL-6R) treatment on immunoglobulins and anti-HLA antibodies in kidney transplant patients with chronic antibody-mediated rejection. Transplantation 2020 , 104 , 856–863. [ Google Scholar ] [ CrossRef ]
- Sethi, S.; Peng, A.; Najjar, R.; Vo, A.; Jordan, S.C.; Huang, E. Infectious Complications in Tocilizumab-Treated Kidney Transplant Recipients. Transplantation 2021 , 105 , 1818–1824. [ Google Scholar ] [ CrossRef ]
- Ius, F.; Sommer, W.; Tudorache, I.; Kühn, C.; Avsar, M.; Siemeni, T.; Salman, J.; Hallensleben, M.; Kieneke, D.; Greer, M.; et al. Preemptive treatment with therapeutic plasma exchange and rituximab for early donor-specific antibodies after lung transplantation. J. Heart Lung Transplant. 2015 , 34 , 50–58. [ Google Scholar ] [ CrossRef ]
- Stuckey, L.J.; Kamoun, M.; Chan, K.M. Lung transplantation across donor-specific anti-human leukocyte antigen antibodies: Utility of bortezomib therapy in early graft dysfunction. Ann. Pharmacother. 2012 , 46 , e2. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Ensor, C.R.; Yousem, S.A.; Marrari, M.; Morrell, M.R.; Mangiola, M.; Pilewski, J.M.; D’cunha, J.; Wisniewski, S.R.; Venkataramanan, R.; Zeevi, A.; et al. Proteasome inhibitor carfilzomib-based therapy for antibody-mediated rejection of the pulmonary allograft: Use and short-term findings. Am. J. Transplant. 2017 , 17 , 1380–1388. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Pham, C.; Pierce, B.J.; Nguyen, D.T.; Graviss, E.A.; Huang, H.J. Assessment of Carfilzomib Treatment Response in Lung Transplant Recipients with Antibody-mediated Rejection. Transplant. Direct 2021 , 7 , e68. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Muller, Y.D.; Aubert, J.D.; Vionnet, J.; Rotman, S.; Sadallah, S.; Aubert, V.; Pascual, M. Acute antibody-mediated rejection 1 week after lung transplantation successfully treated with Eculizumab, Intravenous Immunoglobulins, and Rituximab. Transplantation 2018 , 102 , e301–e303. [ Google Scholar ] [ CrossRef ]
- Dawson, K.L.; Parulekar, A.; Seethamraju, H. Treatment of hyperacute antibody-mediated lung allograft rejection with eculizumab. J. Heart Lung Transplant. 2012 , 31 , 1325–1326. [ Google Scholar ] [ CrossRef ]
- Schinstock, C.A.; Bentall, A.J.; Smith, B.H.; Cornell, L.D.; Everly, M.; Gandhi, M.J.; Stegall, M.D. Long-term outcomes of eculizumab-treated positive crossmatch recipients: Allograft survival, histologic findings, and natural history of the donor-specific antibodies. Am. J. Transplant. 2019 , 19 , 1671–1683. [ Google Scholar ] [ CrossRef ]
- Baskaran, G.; Tiriveedhi, V.; Ramachandran, S.; Aloush, A.; Grossman, B.; Hachem, R.; Mohanakumar, T. Efficacy of extracorporeal photopheresis in clearance of antibodies to donor-specific and lung-specific antigens in lung transplant recipients. J. Heart Lung Transplant. 2014 , 33 , 950–956. [ Google Scholar ] [ CrossRef ]
- Benazzo, A.; Worel, N.; Schwarz, S.; Just, U.; Nechay, A.; Lambers, C.; Böhmig, G.; Fischer, G.; Koren, D.; Muraközy, G.; et al. Outcome of extracorporeal photopheresis as an add-on therapy for antibody-mediated rejection in lung transplant recipients. Transfus. Med. Hemother. 2020 , 47 , 205–213. [ Google Scholar ] [ CrossRef ]
- Jackups, R., Jr.; Canter, C.; Sweet, S.C.; Mohanakumar, T.; Morris, G.P. Measurement of donor-specific HLA antibodies following Plasma Exchange Therapy Predicts Clinical Outcome in Pediatric Heart and Lung Transplant Recipients with Antibody-mediated Rejection. J. Clin. Apher. 2013 , 28 , 301–308. [ Google Scholar ] [ CrossRef ]
- Timofeeva, O.A.; Choe, J.; Alsammak, M.; Yoon, E.J.; Geier, S.S.; Mathew, L.; McCollick, A.; Carney, K.; Au, J.; Diamond, A.; et al. Guiding therapeutic plasma exchange for antibody-mediated rejection treatment in lung Transplant recipients—A retrospective study. Transpl. Int. 2021 , 34 , 700–708. [ Google Scholar ] [ CrossRef ]
- Roux, A.; Bunel, V.; Belousova, N.; Messika, J.; Tanaka, S.; Salpin, M.; Roussel, A.; Beaumont-Azuar, L.; Picard, C.; Brugiere, O.; et al. First use of imlifidase desensitization in a highly sensitized lung transplant candidate: A case report. Am. J. Transplant. 2023 , 23 , 294–297. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Vo, A.A.; Jordan, S.C. Benefits, efficacy, cost-effectiveness and infectious complications in transplant patients desensitized with intravenous immunoglobulin and anti-CD20 therapy. Clin. Exp. Immunol. 2014 , 178 (Suppl. S1), 48–51. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Shevach, E.M. Mechanisms of foxp3+ T regulatory cell-mediated suppression. Immunity 2009 , 30 , 636–645. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Tedla, F.M.; Roche-Recinos, A.; Brar, A. Intravenous immunoglobulin in kidney transplantation. Curr. Opin. Organ. Transplant. 2015 , 20 , 630–637. [ Google Scholar ] [ CrossRef ]
- Panda, S.; Ding, J.L. Natural antibodies bridge innate and adaptive immunity. J. Immunol. 2015 , 149 , 13–20. [ Google Scholar ] [ CrossRef ]
- Nguyen, T.T.T.; Baumgarth, N. Natural IgM and the Development of B cell-mediated autoimmune diseases. Crit. Rev. Immunol. 2016 , 36 , 163–177. [ Google Scholar ] [ CrossRef ]
- Lobo, P.I. Role of Natural Autoantibodies and Natural IgM Anti-Leucocyte Autoantibodies in Health and Disease. Front. Immunol. 2016 , 7 , 198. [ Google Scholar ] [ CrossRef ]
- Perez, E.E.; Orange, J.S.; Bonilla, F.; Chinen, J.; Chinn, I.K.; Dorsey, M.; El-Gamal, Y.; Harville, T.O.; Hossny, E.; Mazer, B.; et al. Update on the use of immunoglobulin in human disease: A review of evidence. J. Allergy Clin. Immunol. 2017 , 139 , S1–S46. [ Google Scholar ] [ CrossRef ]
- Liu, J.; Wang, Y.; Xiong, E.; Hong, R.; Lu, Q.; Ohno, H.; Wang, J.Y. Role of the IgM Fc receptor in immunity and tolerance. Front. Immunol. 2019 , 10 , 529. [ Google Scholar ] [ CrossRef ]
- Matsuda, Y.; Hiramitsu, T.; Li, X.K.; Watanabe, T. Characteristics of Immunoglobulin M Type Antibodies of Different Origins from the Immunologic and Clinical Viewpoints and Their Application in Controlling Antibody-Mediated Allograft Rejection. Pathogens 2020 , 10 , 4. [ Google Scholar ] [ CrossRef ]
- Maddur, M.S.; Lacroix-Desmazes, S.; Dimitrov, J.D.; Kazatchkine, M.D.; Bayry, J.; Kaveri, S.V. Natural antibodies: From first-line defence against pathogens to perpetual immune homeostasis. Clin. Rev. Allergy Immunol. 2020 , 58 , 213–228. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Ius, F.; Sommer, W.; Verboom, M.; Erdfelder, C.; Tudorache, I.; Kühn, C.; Avsar, M.; Siemeni, T.; Salman, J.; Greer, M.; et al. IgM-Enriched Human Intravenous Immunoglobulin-Based Treatment of Patients with Early Donor Specific Anti-HLA Antibodies After Lung Transplantation. Transplantation 2016 , 100 , 2682–2692. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Ius, F.; Verboom, M.; Sommer, W.; Poyanmehr, R.; Knoefel, A.K.; Salman, J.; Kuehn, C.; Avsar, M.; Siemeni, T.; Erdfelder, C.; et al. Preemptive treatment of early donor-specific antibodies with IgA- and IgM-enriched intravenous human immunoglobulins in lung transplantation. Am. J. Transplant. 2018 , 18 , 2295–2304. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Ius, F.; Müller, C.; Sommer, W.; Verboom, M.; Hallensleben, M.; Salman, J.; Siemeni, T.; Kühn, C.; Avsar, M.; Bobylev, D.; et al. Six-year experience with treatment of early donor-specific anti-HLA antibodies in pediatric lung transplantation using a human immunoglobulin-based protocol. Pediatr. Pulmonol. 2020 , 55 , 754–764. [ Google Scholar ] [ CrossRef ]
- Appel, J.Z., III; Hartwig, M.G.; Davis, R.D.; Reinsmoen, N.L. Utility of peritransplant and rescue intravenous immunoglobulin and extracorporeal immunoadsorption in lung transplant recipients sensitized to HLA antigens. Hum. Immunol. 2005 , 66 , 378–386. [ Google Scholar ] [ CrossRef ]
- Snyder, L.D.; Gray, A.L.; Reynolds, J.M.; Arepally, G.M.; Bedoya, A.; Hartwig, M.G.; Davis, R.D.; Lopes, K.E.; Wegner, W.E.; Chen, D.F.; et al. Antibody desensitization therapy in highly sensitized lung transplant candidates. Am. J. Transplant. 2014 , 14 , 849–856. [ Google Scholar ] [ CrossRef ]
- Tinckam, K.J.; Keshavjee, S.; Chaparro, C.; Barth, D.; Azad, S.; Binnie, M.; Chow, C.W.; de Perrot, M.; Pierre, A.F.; Waddell, T.K.; et al. Survival in sensitized lung transplant recipients with perioperative desensitization. Am. J. Transplant. 2015 , 15 , 417–426. [ Google Scholar ] [ CrossRef ]
- Aversa, M.; Martinu, T.; Patriquin, C.; Cypel, M.; Barth, D.; Ghany, R.; Ma, J.; Keshavjee, S.; Singer, L.G.; Tinckam, K. Long-term outcomes of sensitized lung transplant recipients after peri-operative desensitization. Am. J. Transplant. 2021 , 21 , 3444–3448. [ Google Scholar ] [ CrossRef ]
- Parquin, F.; Zuber, B.; Vallée, A.; Taupin, J.-L.; Cuquemelle, E.; Malard, S.; Neuville, M.; Devaquet, J.; Le Guen, M.; Fessler, J.; et al. A virtual crossmatch-based strategy for perioperative desensitisation in lung transplant recipients with pre-formed donor-specific antibodies: 3-year outcome. Eur. Respir. J. 2021 , 58 , 2004090. [ Google Scholar ] [ CrossRef ]
- Heise, E.L.; Chichelnitskiy, E.; Greer, M.; Franz, M.; Aburahma, K.; Iablonskii, P.; de Manna, N.D.; Christoph, S.; Verboom, M.; Hallensleben, M.; et al. Lung transplantation despite preformed donor-specific antihuman leukocyte antigen antibodies: A 9-year single-center experience. Am. J. Transplant. 2023 , 23 , 1740–1756. [ Google Scholar ] [ CrossRef ]
- Butler, C.L.; Valenzuela, N.M.; Thomas, K.A.; Reed, E.F. Not all antibodies are created equal: Factors that influence antibody mediated rejection. J. Immunol. Res. 2017 , 2017 , 7903471. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Daoud, A.H.S.; Betensley, A.D. Diagnosis and treatment of antibody mediated rejection in lung transplantation: A retrospective case series. Transpl. Immunol. 2013 , 28 , 1–3. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Otani, S.; Davis, A.K.; Cantwell, L.; Ivulich, S.; Pham, A.; Paraskeva, M.A.; Snell, G.I.; Westall, G.P. Evolving experience of treating antibody-mediated rejection following lung transplantation. Transpl. Immunol. 2014 , 31 , 75–80. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Islam, A.K.; Sinha, N.; DeVos, J.M.; Kaleekal, T.S.; Jyothula, S.S.; Teeter, L.D.; Nguyen, D.T.M.; Eagar, T.N.; Moore, L.W.; Puppala, M.; et al. Early clearance vs persistence of de novo donor-specific antibodies following lung transplantation. Clin. Transplant. 2017 , 31 , e13028. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Vacha, M.; Chery, G.; Hulbert, A.; Byrns, J.; Benedetti, C.; Finlen Copeland, C.A.; Gray, A.; Onwuemene, O.; Palmer, S.M.; Snyder, L.D. Antibody depletion strategy for the treatment of suspected antibody-mediated rejection in lung transplant recipients: Does it work? Clin Transplant. 2017 , 31 , e12886. [ Google Scholar ] [ CrossRef ]
- Khush, K.K.; Cherikh, W.S.; Chambers, D.C.; Harhay, M.O.; Hayes, D.; Hsich, E.; Meiser, B.; Potena, L.; Robinson, A.; International Society for Heart and Lung Transplant; et al. The international thoracic organ transplant registry of the international society for heart and lung transplantation: Thirty-sixth adult heart transplantation report–2019; focus theme: Donor and recipient size match. J. Heart Lung Transplant. 2019 , 38 , 1056–1066. [ Google Scholar ] [ CrossRef ]
- Noda, K.; Furukawa, M.; Chan, E.G.; Sanchez, P.G. Expanding Donor Options for Lung Transplant: Extended Criteria, Donation After Circulatory Death, ABO Incompatibility, and Evolution of Ex Vivo Lung Perfusion. Transplantation 2023 , 107 , 1440–1451. [ Google Scholar ] [ CrossRef ]
- Levvey, B.J.; Snell, G.I. How do we expand the lung donor pool? Curr. Opin. Pulm. Med. 2024 , 30 , 398–404. [ Google Scholar ] [ CrossRef ]
- Strüber, M.; Warnecke, G.; Hafer, C.; Goudeva, L.; Fegbeutel, C.; Fischer, S.; Gottlieb, J.; Avsar, M.; Simon, A.R.; Haverich, A. Intentional ABO-incompatible lung transplantation. Am. J. Transplant. 2008 , 8 , 2476–2478. [ Google Scholar ] [ CrossRef ]
- Chen-Yoshikawa, T.F. ABO blood type incompatible lung transplantation. J. Thorac. Dis. 2023 , 15 , 3437–3442. [ Google Scholar ] [ CrossRef ]
- Wood, K.J.; Bushell, A.; Hester, J. Regulatory immune cells in transplantation. Nat. Rev. Immunol. 2012 , 12 , 417–430. [ Google Scholar ] [ CrossRef ]
Click here to enlarge figure
| Parameter | Lund | OCS | Toronto |
|---|---|---|---|
| Perfusion | |||
| Perfusate | Cellular | Cellular | Acellular |
| Solution | STEEN | OCS | STEEN |
| Cellular component | RBCs | RBCs | none |
| Target flow | 100% cardiac output | 2–2.5 L/min | 40% cardiac output |
| Flow type | Continuous | Pulsatile | Continuous |
| PA pressure | <20 mmHg | <20 mmHg | <15 mmHg |
| Left atrium | Open | Open | Closed |
| Ventilation | |||
| Start temperature | 32 °C | 34 °C | 32 °C |
| Tidal volume | 5–7 mL/kg | 6 mL/kg | 7 mL/kg |
| Respiratory rate | 20/min | 10/min | 7/min |
| FiO (%) | 0.5 | 0.12 | 0.21 |
| Transportability | Static | Portable | Static |
| The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
Share and Cite
Aburahma, K.; de Manna, N.D.; Kuehn, C.; Salman, J.; Greer, M.; Ius, F. Pushing the Survival Bar Higher: Two Decades of Innovation in Lung Transplantation. J. Clin. Med. 2024 , 13 , 5516. https://doi.org/10.3390/jcm13185516
Aburahma K, de Manna ND, Kuehn C, Salman J, Greer M, Ius F. Pushing the Survival Bar Higher: Two Decades of Innovation in Lung Transplantation. Journal of Clinical Medicine . 2024; 13(18):5516. https://doi.org/10.3390/jcm13185516
Aburahma, Khalil, Nunzio Davide de Manna, Christian Kuehn, Jawad Salman, Mark Greer, and Fabio Ius. 2024. "Pushing the Survival Bar Higher: Two Decades of Innovation in Lung Transplantation" Journal of Clinical Medicine 13, no. 18: 5516. https://doi.org/10.3390/jcm13185516
Article Metrics
Article access statistics, further information, mdpi initiatives, follow mdpi.

Subscribe to receive issue release notifications and newsletters from MDPI journals
- Research article
- Open access
- Published: 27 May 2020
Knowledge, attitude and willingness to donate organ among medical students of Jimma University, Jimma Ethiopia: cross-sectional study
- Fantu Kerga Dibaba ORCID: orcid.org/0000-0003-4331-3907 1 ,
- Kabaye Kumela Goro 1 ,
- Amare Desalegn Wolide 2 ,
- Fanta Gashe Fufa 1 ,
- Aster Wakjira Garedow 1 ,
- Birtukan Edilu Tufa 3 &
- Eshetu Mulisa Bobasa 1
BMC Public Health volume 20 , Article number: 799 ( 2020 ) Cite this article
7991 Accesses
19 Citations
7 Altmetric
Metrics details
The lack of organ donors has become a limiting factor for the development of organ transplantation programs. Many countries are currently facing a severe shortage of organs for transplantation. Medical students, as future doctors can engage in the role of promoting organ donation by creating awareness and motivating the community to donate their organs besides their voluntary organ donation. The aim of this study is to assess the knowledge, attitude and willingness of undergraduate medical students’ towards organ donation at Jimma University.
A cross-sectional study was conducted among 320 medical students from year I to internship using questionnaire in order to assess their knowledge, attitude and willingness regarding organ donation. Data collected was entered using epidata and analyzed using Statistical Package for Social Sciences (SPSS) software version 20.
Mean (±SD = standard deviation) age of participants was 23.48 ± 17.025 years. 57.8% of the study subjects were male. There was a statistically significant interaction effect between gender and year of study on the combined knowledge questions (dependent variables) F(25,062) = 1.755, P = 0.014, Wilk’s Λ = .033. Variables which were related to a positive attitude towards organ donation were: being of the male sex (Odds Ratio = 1.156); having awareness about organ donation (Odds Ratio = 2.602); not having a belief on the importance of burying intact body (Odds Ratio = 5.434); willingness to donate blood (Odds Ratio = 4.813); and willingness to donate organ (Odds Ratio = 19.424).
High level of knowledge but low level of positive attitude and willingness was noticed among the study participants toward organ donation.
Peer Review reports
The need for organ donation has increased globally in the past years due to an increase in organ failure [ 1 ]. Every day in the United States of America (USA), 21 people die waiting for an organ and more than 120,048 men, women, and children await life-saving organ transplants [ 2 ]. Accor-ding to a survey In India every year about 5 lakh (500,000) people die because of non-availability of organs and 1.5 lakh(150,000) people await a kidney transplant but only 5000 get among them [ 3 ]. Recently published report has found that approximately 3 million people in sub-Saharan Africa diagnosed with end-stage kidney disease (ESKD) die each year due to renal failure [ 4 ]. In Kenya, the kidney transplant queue at Kenyatta National Hospital in Nairobi stretches all the way to 2018, despite the hospital performing the procedure on a weekly basis [ 5 ]. In Ethiopia, between 130 and 150 corneas are collected yearly. However, there are more than 300,000 blind people waiting for corneal transplantation [ 6 ].
There are no sufficient facilities which provide maintenance and transplantation therapy for failed organs in Ethiopia. Currently there are only cornea and living related kidney transplant programs established in the nation’s capital Addis Ababa [ 6 ]. Facilities which provide maintenance dialysis has been in existence in the country starting from 2001. Hemodialysis has become on hand in private institutions, mostly in Addis Ababa the capital city of the country, and more recently in a few other urban and semi-urban regions. Currently, there are 30 hemodialysis centers with a total of 186 hemodialysis chairs and approximately 800 patients on hemodialysis. Among patients on maintenance dialysis, only about one-third receives treatment 3× per year because the cost of hemodialysis is unaffordable for the majority of patients [ 7 ].
Organ transplantation is one of the great advances in modern medicine and is the best option for failed organ. Transplantation is defined as the transfer of human cells, tissues or organs from a donor to recipient with an aim of restoring normal physiology in the body [ 8 ]. In Ethiopia, up to 2018, 1336 corneal and 90 living donor kidney transplants have been performed. Currently the kidney transplant program accepts candidates only at the age of 14 and above [ 7 , 9 ].
Some studies found out that the issue of organ donation is multifactorial. In developed countries relational ties, religious beliefs, cultural influences, family influences, body integrity, and previous interactions with the health-care system were reported as the potential factors for organ donation [ 10 ]. However, there are limited studies regarding organ donation and the factors that influence it in developing countries for instance, in Kenya there are peoples who believe a person’s body should be intact when buried this belief and other sociocultural and legal factors hinder the harvest of organ from patients who have been medically declared to be in a “state of dying” [ 5 ].
Among 100,000 of people died each year are believed to be potential donors; however, only less than 200 actually become donors [ 11 ]. This indicates that a lot should be done on awareness creation towards organ donation. As a new approach in solving the organ shortage, it has been suggested that awareness about organ donation to be made a part of school education [ 12 ]. In Ethiopia we suggest to use religious leaders besides to incorporating the issue in school education, because Ethiopia is religious country. Our country has close ties with all three major Abrahamic religions, and it was the first in the region to officially adopt Christianity in the fourth century. Christians account for 63% of the country’s population, with 43.5% belonging to the Ethiopian Orthodox Church, 18.5% Protestant and 0.7% Catholic. Ethiopia has the first Hijra in Islamic history and the oldest Muslim settlement on the continent. Muslims account for 34% of the population, traditional 2.7% and other 0.6% [ 13 ].
In Ethiopia there are no data on public perception of organ donation and transplantation Therefore, the present study was designed to assess the knowledge, attitude and willingness of organ donation among medical students. Medical students, as future doctors can take up the role of promoting organ donation by educating and motivating the public to initiate them donate their organs besides their voluntary organ donation. Therefore, assessing medical student’s knowledge, attitude and willingness to donate organ is very important to decrease the shortage of organ in the future.
Study setting and subjects
A cross sectional study was carried out for 3 months from May to July 2019among under graduate medical students in Jimma University after obtaining Institutional Ethical Clearance from institutional review board (IRB) of Jimma University. The University is located in Jimma town which is 352 km from Addis Ababa, the capital city of Ethiopia. Jimma University is one of the most distinguished centers of excellence in medical education in the country.
Sample size
All medical students (from first to internship) registered in the year 2018/2019 were the source population. Based on their training background, medical students in Jimma University were divided into two groups: PRE-CLINICAL and CLINICAL. PRECLINICAL is subdivided in to two groups: Year I (PC-I) and Year II (PC-II) and CLINICAL in to three subgroups Year III(C-I), Year IV(C-II) and internship. The sample size was calculated by using simple proportion formula assuming a prevalence of 50% for knowledge, attitudes and willingness of organ donation, a 95% confidence interval and a sample error of 5%. This was adjusted for 10% non-response rate; bringing the total sample size to 320.There were about 1200 students studying in Jimma University medical school.
The questionnaire was distributed to undergraduate medical students during lecture hours in the classroom and in ward during attachment. They were instructed not to discuss the questions among themselves. The importance of the study was explained and confidentiality regarding the participant response for the questions was ensured.
A 20-item self-administered questionnaire was developed. The first part of the questionnaire gathered the demographic details from the students, which included age, gender, year of study and religion. The second, third and fourth sections assessed the levels of knowledge (Q1–7), attitude (Q8–16) and willingness (Q17–20) to donate organ, respectively.
The students were grouped as those who do have adequate and inadequate knowledge based on their score.
Adequate knowledge is when 4–6 questions were answered correctly and inadequate when less than 4 questions answered correctly out of 6 knowledge questions.
Attitude was assessed by using 9 attitude statements and respondents were categorized as those who do have positive attitude and negative if they agree to 6–9 and less than 6 attitude statements respectively.
Statistical analysis
Data was entered to EPI data and exported to SPSS version 20 for analysis. Descriptive statistics like percentage and mean and standard deviation were used to present socio-demography, knowledge, attitude and willingness response of the participants. Multivariate analysis was used in order to relate those factors that gave a significant result: One way Multivariate analysis of variance (MANOVA) was used to see a significant relationship between one independent variable and dependent variables and two ways MANOVA was considered to know if there was an interaction between two independent variables on the dependent variables. One way Analysis of Variance (ANOVA) was used for comparing means of variables to know among which groups were the differences. Finally, Odds ratio analysis was used to find out variables which were related to a positive attitude towards organ donation.
Out of 320 participants 57.8% were male. Mean (±SD = standard deviation) age of participants was 23.48 ± 17.025 years. Majority of the participants were orthodox (49%.7) and the least percentage being others constituting wakeefeta, apostolic, humanity, atheist and Seventh Day Adventist (SDA) (2.8%) (Table 1 ).
96.9% of the students had awareness about organ donation. Only 25% had knowledge that there was no age limit for organ donation (Table 2 ).
There was a statistically significant difference in level of knowledge between study groups as demonstrated by one-way ANOVA(F (4,315) =7.6, p = 0.001). Based on the post hoc test the significant difference was between PC-I and C-II( p = 0.001), PC-I and intern( p = 0.001), PC-II and C-I( P = 0.022) and PC-II and intern( p = 0.010). The mean for PC-I, PC-II, C-I, C-II and intern is 1.37, 1.27, 1.20, 1.08 and 1.05 respectively. Therefore, PC=I had significantly higher level of knowledge when compared to the rest year of study (Table 3 ).
74.1% of the participants agreed to support family members if they wish to become an organ donor. Majority of the study subjects (91.9%) felt that awareness about organ donation should be made a part of school education (Table 4 ).
According to our finding, males were 1.156 (Odds Ratio = 1.156) times likely to have positive attitude towards to organ donation as compared to female. Students who had an awareness about organ donation were 2.602 (Odds Ratio = 2.602) times likely to have positive attitude towards to organ donation as compared to those who were unaware. The other variables which were related to a positive attitude towards organ donation were: not having a belief on the importance of burying intact body (Odds Ratio = 5.434); knowing definition of brain death (Odds Ratio = 1.257); not having a belief that there is a danger of misuse, abuse or misappropriation of donated organ (Odds Ratio = 2.777); willingness to donate blood (Odds Ratio = 4.813); and willingness to donate organ (Odds Ratio = 19.424).
58.1% of the study participants were willing to donate their organs and allow organ donation after the death of a family member. Majority of the study subjects (88.4%) did not like to take money for organ donation. 90.3% of the study subjects were willing to donate blood and 58.1% were willing to donate their organ (Table 5 ) (Fig. 1 ).
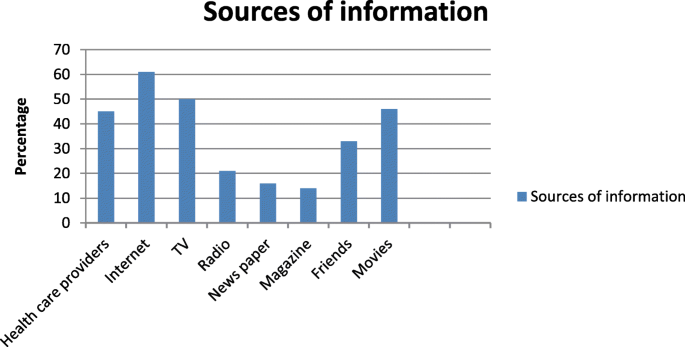
Distribution of study subjects according to the source of information about organ donations. i.e. Note: No of respondents may be greater than sample size as multiple options were allowed. Most common source of information about organ donation was found to be internet (61%) television (50%) followed by, Movies and health care providers 46 and 45% respectively
There were an association between willingness and attitude. Willingness to donate organ was significantly higher among those who do have positive attitude (88.2%) as compared to those with negative attitude (11.8%) (Table 6 ).
There was a statistically significant difference on belief of burying intact body between religions as demonstrated by one-way ANOVA(F (3,316) =4.5, p = .004). Based on the post hoc test the significant difference was between Protestant and Muslim ( p = .007). The mean for protestant is 1.83 and Muslim 1.56.Therefore, Protestant had significantly higher belief on the importance of burying intact body when compared to Muslim (Table 7 ).
There was a statistically significant difference between males and females when knowledge questions considered jointly Wilk’s Λ = .96, F (6,312) = 2.247, P = 0.039, multivariate ƞ 2 = 0.041 and attitude statements consider jointly Wilk’s Λ = .94, F (9,310) = 2.301, P = 0.016, multivariate ƞ 2 = 0.063.
When year of study is considered, there was a statistically significant difference among year of studies when knowledge questions considered jointly Wilk’s Λ = .75, F (25,079) = 3.966, P < 0.001, multivariate ƞ 2 = .071, attitude statements considered jointly Wilk’s Λ = .77, F (37,152) = .766, P < 0.001, multivariate ƞ 2 = .065 and willingness questions considered jointly Wilk’s Λ = .93, F (12,828) = 2.072, P = 0.017, multivariate ƞ 2 = .026.
Two way MANOVA was considered to know if there was an interaction between two independent variables on the dependent variables. There was a statistically significant interaction effect between gender and year of study on the combined knowledge questions (dependent variables) F (25,062) = 1.755, P = 0.014, Wilk’s Λ = .033.
Knowledge of the participant
Organ failure and shortage of donated organs are global problem. Among 100,000 of people died each year are believed to be potential donors; however, only less than 200 actually become donors [ 9 ]. The widespread shortage of donated organs indicates that there is low donor rate worldwide; In Ethiopia there is no data on rate of organ donation. In 2017 Spain had the highest donor rate in the world at 46.9 per million people, followed by Portugal (34.0 per million), Belgium (33.6 per million), Croatia (33.0 per million) and the US (32.0 per million) [ 14 ]. Donated organs are the major pre-requisite for consistency of organ transplantation program; one of the solutions to increase organ supply is to assess public knowledge, attitude and willingness towards organ donation and taking an action based on the data. In our country there is no study done on people’s perception towards organ donation this background pledges us to conduct this study.
In our study 96.9% of the participants heard about organ donation which is similar to study done by Annadurai et al and Jothula et al. [ 15 , 16 ] both reported that 100% of the participants were aware about organ donation.74.1% of the participants were aware about the meaning of organ donation which is relatively higher than the study done by Annadurai et al. [ 15 ]. In the present study, level of knowledge was significantly higher among PC=I (year I) students as compared to the other year of study this finding was similar to study done among undergraduate dental students of Panineeya Institute of Dental Sciences and Hospital, which showed higher average knowledge among first-year students [ 17 ]. In this study, only 82.5%of medical students had adequate knowledge about organ donation which is relatively higher than the study done on final semester medical students by Karini et al. which showed that only 56% of them were having adequate knowledge [ 18 ].
In the present study the main sources of information about organ donation was found to be internet (61%) and television (50%).This was similar to study conducted in USA and Australia [ 19 , 20 ]. However; Similar findings were observed by Sindhu et al. and Jothula KY et al. [ 16 , 21 ]. The third source of information about organ donation in our study are health care providers (45%) which is relatively higher than the study done by Annadurai et al. [ 15 ] which reported 34.1%. this finding showed that health care providers are playing undeniable role in creating awareness towards organ donation in Ethiopia.
206(64.4%) of our study participants had identified all the organs that can be donated. This finding was higher than the study done by Annadurai et al. [ 15 ] and Karini et al. [ 18 ] which reported 16.1 and 26% respectively. In the present study 80(25%) of the students knew that there is no age limit for organ donation which is approximate to Sucharitha et al. and lower than Jothula KY et al. [ 16 , 22 ].
Attitude of medical students regarding organ donation
201(62.8%) of our study subjects have a positive attitude towards organ donation which is lower than the study in Spain and India which found 80 and 71.3% respectively [ 23 , 24 ]. 91.9% of this study subjects, felt that awareness about organ donation should be included in school curriculum which is similar to Adithyan et al. reported that 91.2% of the subjects felt the need for revision of medical curriculum on organ donation [ 25 ] Our study found out that 251(78.4%) of the study subjects would like to motivate others for organ donation which is lower than to the Vinay et al [ 26 ].
77(24.1%) of our study subjects belief that person’s body should be intact when buried A study in USA reported that 8% of participants strongly agree and 11.7% agree to this statement which is almost similar to our finding [ 19 ]. In our study being of the male sex (Odds Ratio = 1.156) was related to a favorable attitude towards to organ donation; in contrast, a study done in Spain reported that being of females sex (Odds Ratio = 1.739) was related to a favorable attitude [ 23 ]. In our study not having a belief on the importance of burying intact body (Odds Ratio = Ratio = 5.434) was one of the variables which affect positive attitude towards to organ donation which was similar to a study in USA [ 19 ]. A study done in Spain reported being a blood donor (OR = 2.824) as a variable related to a positive attitude towards to organ donation similarly in our study we found out willingness to donate blood (Odds Ratio = 4.813) as a variable to a favorable attitude.
Willingness of medical students to donate organ
In this study 186(58.1%) of the study participants were willing to donate their organ which is similar to a study done in USA [ 20 ] and lower than Payghan et al. and Vinay et al revealed that almost 90% of study participants were willing to donate their organs [ 26 , 27 ]. The present study found out that there is a significant association between attitude regarding organ donation and willingness to donate organs which is different from the finding by Ali et al. and by Dasgupta et al. [ 28 , 29 ] which reported that there was a significant association between attitude and knowledge acquired. Though taking money for organ donation is unethical 11.6% of our study participants would like to take money for organ donation which was higher than study by Jothula KY et al. [ 16 ].
Though most of the students had adequate knowledge, still gaps exist in their attitude and willingness. This implies the need for an intensified and sustained education to raise attitude and willingness of the students towards organ donation.
Recommendations
Most of the students (91.9%) felt that awareness about organ donation should be made a part of school education; until it included in school curriculum, we recommend the students to acquire an adequate knowledge by themselves; In our study the most common source of information about organ donation was internet; so, they can browse more to acquire additional knowledge and make informed decision.
Availability of data and materials
The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.
Abbreviations
Analysis of variance
Clinical-II
End-stage kidney disease
Institutional Review Board
Jimma University Medical College
Multivariate analysis of variance
Pre-clinical-I
Pre-clinical-II
Seventh Day Adventist
Statistical Package for Social Sciences
United States of America
Wakefield MA, Loken B, Hornik RC. Use of mass media campaigns to change health behaviour. Lancet. 2010;376(9748):1261–71.
Article Google Scholar
Organ Donation Facts & Info _ Organ Transplants _ Cleveland Clinic www.unos.org , Nov. 1, 2016. Accessed 26 Jan 2020.
National Health Portal. “Organ donation day”. Available at http://www.nhp.gov.in/organdonation-day_pg . Accessed 18 Feb 2018.
Ashuntantang G, Osafo C, Olowu WA, et al. Outcomes in adults and children with end-stage kidney disease requiring dialysis in sub-Saharan Africa: a systematic review. Lancet Glob Health. 2017;5:e408–17.
Organ failure: patients in East Africa wait endlessly for donors. Science & Health https://www.theeastafrican.co.ke . Accessed 26 Aug 2019.
Rao GN, Gopinathan U. Eye banking: an introduction. Community Eye Health. 2009;22(71):46–7.
PubMed PubMed Central Google Scholar
Ahmed, et al. Organ transplantation in Ethiopia. 2019;103(3):449–51.
World Health Organisation (WHO). Global glossary of terms and definitions on donation and transplantation, vol. 14. Geneva; 2009.
13. Eye Bank of Ethiopia celebrates 15 th anniversary June 28, 2018 by New Business Ethiopia. http://newbusinessethiopia.com/health/eye-bank-of-ethiopia-celebrates-15th-anniversary/ .
Irving MJ, Tong A, Jan S, Cass A, Rose J, Chadban S, et al. Factors that influence the decision to be an organ donor: a systematic review of the qualitative literature. Nephrol Dial Transplant. 2012;27:2526–33.
Sahi M. Myths and misconceptions and reality on organ donation. Transplantation Research. https://www.mohanfoundation.org/organ-donation-transplant-resources/Myths-Misconceptions-and-the-Reality-of-Organ-Donation.asp .
Burra P, De Bona M, Canova D, et al. Changing attitude to organ donation and transplantation in university students during the years of medical school in Italy. Transplant Proc. 2005;37:547–50.
Article CAS Google Scholar
Ethiopia PEOPLE 2019, CIA World Fact book Theodora.com https://theodora.com/wfbcurrent/ethiopia/ethiopia_people.html .
Newsletter 2018 (PDF). International registry in organ donation and transplantation. 2018 . Retrieved December 30, 2018 . .
Google Scholar
Annadurai K, Mani K, Ramasamy J. A study on knowledge, attitude and practices about organ donation among college students in Chennai, Tamil Nadu −2012. Prog Health Sci. 2013;3:2 KAP on organ donation.
Jothula KY, Sreeharshika D. Study to assess knowledge, attitude and practice regarding organ donation among interns of a medical college in Telangana, India. Int J Community Med Public Health. 2018;5:1339–45.
Chakradhar K, Doshi D, Srikanth Reddy B, et al. Knowledge, attitude and practice regarding organ donation among Indian dental students. Int J Organ Transplant Med. 2016;7(1):28–35.
CAS PubMed PubMed Central Google Scholar
Karini D, Sunitha S, Devi Madhavi B. Perceptions of medical students in a government medical college towards organ donation. J Evid Based Med Healthc. 2015;2(44):7998–8005.
U.S. Department of Health and Human Services, Health Resources and Services Administration, Healthcare Systems Bureau, 2012 National Survey of Organ Donation Attitudes and Behaviors. Rockville, Maryland: U.S. Department of Health and Human Services; 2013.
Hyde MK, Chambers SK. Information sources, donation knowledge, and attitudes toward transplant recipients in Australia. Prog Transplant. 2014;24:169–77.
Sindhu A, Ramakrishnan TS, Khera A, Singh G. A study to assess the knowledge of medical students regarding organ donation in a selected college of Western Maharashtra. Med J DY Patil Univ. 2017;10:349–53.
Agarwal S. Are medical students having enough knowledge about organ donation. IOSR J Dental Med Sci. 2015;14(7):29–34.
Ríos A, López-Navas A, López-López A, Gómez FJ, Iriarte J, Herruzo R, Blanco G, Llorca FJ, Asunsolo A, Sánchez P, Gutiérrez PR, Fernández A, de Jesús MT, MartínezAlarcón L, Lana A, Fuentes L, Hernández JR, Virseda J, Yelamos J, Bondía JA, Hernández AM, Ayala MA, Ramírez P, Parrilla P. A multicentre and stratified study of the attitude of medical students towards organ donation in Spain. Ethn Health. 2019;24(4):443–61. https://doi.org/10.1080/13557858.2017.1346183 .
Article PubMed Google Scholar
Bathija GV, Ananthesh BG, Bant DD. Study to assess knowledge and attitude towards organ donation among interns and post graduates of a medical college in Karnataka, India. Natl J Community Med. 2017;8(5):236–40.
Adithyan GS, Mariappan M, Nayana KB. A study on knowledge and attitude about organ donation among medical students in Kerala. Indian J Transplant. 2017;11:133–7.
Vinay KV, Beena N, Sachin KS, Praveen S. Changes in knowledge and attitude among medical students towards organ donation and transplantation. Int J Anat Res. 2016;4(3):2873–7.
Payghan BS, Kadam SS, Furmeen S. Organ donation: awareness and perception among medical students. J Pharm Sci Innov. 2014;3(4):379–81.
Ali NF, Qureshi A, Jilani BN, Zehra N. Knowledge and ethical perception regarding organ donation among medical students. BMC Med Ethics. 2013;14:38.
Dasgupta A, Shahbabu B, Sarkar K, Sarkar I, Das S, Das MK. Perception of organ donation among adults: a community based study in an urban. Sch J App Med Sci. 2014;2(6A):2016–2021.
Download references
Acknowledgements
Not applicable.
The study was funded with the support of Jimma University; Faculty of Health Science. The funding body has no role in the design of the study and collection, analysis, and interpretation of data and in writing the manuscript.
Author information
Authors and affiliations.
Faculty of Health Sciences, School of Pharmacy, Jimma University, 378, Jimma, Ethiopia
Fantu Kerga Dibaba, Kabaye Kumela Goro, Fanta Gashe Fufa, Aster Wakjira Garedow & Eshetu Mulisa Bobasa
Facility of Medicine, Jimma University, 378, Jimma, Ethiopia
Amare Desalegn Wolide
Faculty of Health Sciences, School of Midwifery and Nursing, Jimma University, 378, Jimma, Ethiopia
Birtukan Edilu Tufa
You can also search for this author in PubMed Google Scholar
Contributions
FKD, EMB, KKG, ADW, FGF, AWG, BET involved in the data collection. FKD analyze the data and FKD and EMB prepared the manuscript. All authors read and approved the final manuscript.
Corresponding author
Correspondence to Fantu Kerga Dibaba .
Ethics declarations
Ethics approval and consent to participate.
The study protocol was approved by the institutional review board (IRB) of Jimma University, College of Health Sciences and ethical clearance was obtained with the Reference Number IHRPGD/3019/2019. Permission of data collection was granted with formal letter from chief executive director of Jimma University Medical College (JUMC). The purpose and protocol of this study was explained, participants signed informed written consent.
Consent for publication
Competing interests.
The authors declare that they have no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Dibaba, F.K., Goro, K.K., Wolide, A.D. et al. Knowledge, attitude and willingness to donate organ among medical students of Jimma University, Jimma Ethiopia: cross-sectional study. BMC Public Health 20 , 799 (2020). https://doi.org/10.1186/s12889-020-08931-y
Download citation
Received : 19 September 2019
Accepted : 17 May 2020
Published : 27 May 2020
DOI : https://doi.org/10.1186/s12889-020-08931-y
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Organ donation
- Willingness
- Medical students
BMC Public Health
ISSN: 1471-2458
- General enquiries: [email protected]
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
- My Bibliography
- Collections
- Citation manager
Save citation to file
Email citation, add to collections.
- Create a new collection
- Add to an existing collection
Add to My Bibliography
Your saved search, create a file for external citation management software, your rss feed.
- Search in PubMed
- Search in NLM Catalog
- Add to Search
Worldwide barriers to organ donation
Affiliations.
- 1 Neurocritical Care Unit and Stroke Department, Hospital Copa D'Or, Rio de Janeiro, Brazil.
- 2 Cerebrovascular Center of the Neurological Institute, Cleveland Clinic, Cleveland, Ohio.
- PMID: 25402335
- DOI: 10.1001/jamaneurol.2014.3083
Importance: The disparity between patients awaiting organ transplantation and organ availability increases each year. As a consequence, organ trafficking has emerged and developed into a multibillion-dollar-a-year industry.
Objective: To identify and address barriers to organ donation in the United States and globally.
Evidence review: Evidence-based peer-reviewed articles, including prospective and retrospective cohort studies, as well as case series and reports were identified in a PubMed search of organ donation, barriers to organ donation, brain death, donation after cardiac death, and organ trafficking. Additional Internet searches were conducted of national and international transplant and organ donation websites and US Department of Health of Health and Human Services websites. Citation publication dates ranged from August 1, 1968, through June 28, 2014.
Findings: The lack of standardization of brain death and organ donation criteria worldwide contributes to a loss of potential donors. Major barriers to donation include variable clinical and legal definitions of brain death; inconsistent legal upholding of brain death criteria; racial, ethnic, and religious perspectives on organ donation; and physician discomfort and community misunderstanding of the process of donation after cardiac death. Limited international legislation and oversight of organ donation and transplant has contributed to the dilemma of organ trafficking.
Conclusions and relevance: An urgent need exists for a global standard on the definition of brain death and donation after death by cardiac criteria to better regulate organ donation and maximize transplantation rates. Unified standards may have a positive effect on limiting organ trafficking.
PubMed Disclaimer
Similar articles
- National evaluation of healthcare provider attitudes toward organ donation after cardiac death. Mandell MS, Zamudio S, Seem D, McGaw LJ, Wood G, Liehr P, Ethier A, D'Alessandro AM. Mandell MS, et al. Crit Care Med. 2006 Dec;34(12):2952-8. doi: 10.1097/01.CCM.0000247718.27324.65. Crit Care Med. 2006. PMID: 17075366
- The rate of organ and tissue donation after brain death: causes of donation failure in a Romanian university city. Grigoraş I, Blaj M, Florin G, Chelarescu O, Craus C, Neagu R. Grigoraş I, et al. Transplant Proc. 2010 Jan-Feb;42(1):141-3. doi: 10.1016/j.transproceed.2009.11.026. Transplant Proc. 2010. PMID: 20172300
- Improving cadaveric organ donation rates in kidney and liver transplantation in Asia. Vathsala A. Vathsala A. Transplant Proc. 2004 Sep;36(7):1873-5. doi: 10.1016/j.transproceed.2004.08.131. Transplant Proc. 2004. PMID: 15518680
- Islam, brain death, and transplantation: culture, faith, and jurisprudence. Arbour R, AlGhamdi HM, Peters L. Arbour R, et al. AACN Adv Crit Care. 2012 Oct-Dec;23(4):381-94. doi: 10.1097/NCI.0b013e3182683b1e. AACN Adv Crit Care. 2012. PMID: 23095963 Review.
- Eligibility for organ donation: a medico-legal perspective on defining and determining death. Downie J, Kutcher M, Rajotte C, Shea A. Downie J, et al. Can J Anaesth. 2009 Nov;56(11):851-63. doi: 10.1007/s12630-009-9130-x. Epub 2009 Jul 8. Can J Anaesth. 2009. PMID: 19585180 Review.
- Impact of the life-sustaining treatment decision act on organ donation in out-of-hospital cardiac arrests in South Korea: a multi-centre retrospective study. Kim MJ, Lee DE, Kim JK, Yeo IH, Jung H, Kim JH, Jang TC, Lee SH, Park J, Kim D, Ryoo HW. Kim MJ, et al. BMC Med Ethics. 2024 Sep 2;25(1):93. doi: 10.1186/s12910-024-01090-4. BMC Med Ethics. 2024. PMID: 39223644 Free PMC article.
- Attitudes of Polish Medical Students toward Organ Donation in Cases of Brain Death. Mikla M, Rachubińska K, Ríos A, Schneider-Matyka D, Panczyk M, Kotwas A, Karakiewicz B, Grochans E, Cybulska AM. Mikla M, et al. Eur J Investig Health Psychol Educ. 2024 Apr 23;14(5):1114-1127. doi: 10.3390/ejihpe14050073. Eur J Investig Health Psychol Educ. 2024. PMID: 38785571 Free PMC article.
- Medical students' knowledge and attitude toward brain death and the influence of medical education: a cross-sectional study. Liu C, Liu S. Liu C, et al. BMC Med Educ. 2024 Mar 28;24(1):346. doi: 10.1186/s12909-024-05346-w. BMC Med Educ. 2024. PMID: 38549110 Free PMC article.
- Intensive care admission aiming at organ donation. Con. Vergano M, Jung C, Metaxa V. Vergano M, et al. Intensive Care Med. 2024 Mar;50(3):440-442. doi: 10.1007/s00134-024-07326-6. Epub 2024 Jan 25. Intensive Care Med. 2024. PMID: 38270641 No abstract available.
- Organ Donation in the Emergency Department: Awareness and Opportunities. Akeely YY, Al Otaibi MM, Alesa SA, Bokhari NN, Alghamdi TA, Alahmari MS, AlRasheed NK. Akeely YY, et al. Cureus. 2023 Nov 30;15(11):e49746. doi: 10.7759/cureus.49746. eCollection 2023 Nov. Cureus. 2023. PMID: 38161899 Free PMC article.
Publication types
- Search in MeSH
Related information
- Cited in Books
LinkOut - more resources
Full text sources.
- Ovid Technologies, Inc.
- Silverchair Information Systems
Research Materials
- NCI CPTC Antibody Characterization Program
- Citation Manager
NCBI Literature Resources
MeSH PMC Bookshelf Disclaimer
The PubMed wordmark and PubMed logo are registered trademarks of the U.S. Department of Health and Human Services (HHS). Unauthorized use of these marks is strictly prohibited.
- Search Menu
- Sign in through your institution
- Advance Articles
- Editor's Choice
- Cover Archive
- Author videos
- Supplements
- Anniversary Collection
- Cardio-Renal Collection
- Cover Images
- Author Guidelines
- Submission Site
- Open Access Options
- Why publish with NDT?
- About the ERA
- Editorial Board
- Advertising and Corporate Services
- Journals Career Network
- Self-Archiving Policy
- Dispatch Dates
- Terms and Conditions
- Editorial Fellowship
- The ERA Journals
- Journals on Oxford Academic
- Books on Oxford Academic

Article Contents
Introduction, materials and methods, supplementary data.
- < Previous
Factors that influence the decision to be an organ donor: a systematic review of the qualitative literature
- Article contents
- Figures & tables
- Supplementary Data
Michelle J. Irving, Allison Tong, Stephen Jan, Alan Cass, John Rose, Steven Chadban, Richard D. Allen, Jonathan C. Craig, Germaine Wong, Kirsten Howard, Factors that influence the decision to be an organ donor: a systematic review of the qualitative literature, Nephrology Dialysis Transplantation , Volume 27, Issue 6, June 2012, Pages 2526–2533, https://doi.org/10.1093/ndt/gfr683
- Permissions Icon Permissions
Transplantation is the treatment of choice for organ failure, but a worldwide shortage of suitable organs exists. We conducted a systematic review of qualitative studies that explored community attitudes towards living and deceased solid organ donation to inform strategies to improve organ donation rates.
Medline, Embase, PsycINFO and EconLIT were searched. Qualitative studies that explored community attitudes towards living and deceased solid organ donation were included. A thematic synthesis of the results and conclusions reported by primary authors was performed.
Eighteen studies involving 1019 participants were identified. Eight themes emerged. The decision to be an organ donor was influenced by (i) relational ties; (ii) religious beliefs; (iii) cultural influences; (iv) family influences; (v) body integrity; (vi) previous interactions with the health care system—medical mistrust, validity of brain death and fear of early organ retrieval; (vii) the individual’s knowledge about the organ donation process and (viii) major reservations about the process of donation, even in those who support organ donation.
This review of qualitative studies highlights that seemingly intractable factors, such as religion and culture, are often tied in with more complex issues such as a distrust of the medical system, misunderstandings about religious stances and ignorance about the donation process. Intervention that could be considered includes culturally appropriate strategies to engage minority groups, especially through religious or cultural leaders, and more comprehensively available information about the donation process and its positive outcomes.
Transplantation is the treatment of choice for severe organ failure. Despite this, and general recognition of organ donation as a global priority, demand for organs outstrips supply in virtually every country in the world [ 1 ]. Understanding the reasons why people do or do not donate can help inform policies to address this undersupply.
Previous studies have found a number of specific factors that are certainly associated with positive attitudes to organ donation, including education level, socio-economic status and being young [ 2–7 ]. It has also been found that people are more willing to make a living donation to a family member than a donation after death [ 8–11 ], while religious reasons were commonly cited as barriers [ 3 , 5 , 6 , 12 , 13 ].
People beliefs, however, often need to be understood through a broader narrative to uncover the interaction of multiple influences. Qualitative research is able to capture these narratives and their context and therefore helps us better understand the reasons why people hold particular views.
This study aims to synthesize the qualitative research on community attitudes towards living and deceased organ donation and the factors that influence these attitudes.
Study selection
Studies that explored community attitudes towards living and deceased solid organ (heart, lung, liver and kidney) donation using qualitative data through focus groups or interviews were included. Papers were excluded if they focussed on non-solid organ transplantation, were editorials or reviews or discussion papers that did not elicit perspectives from the community.
Literature search
MeSH terms and text words for community (public and population) were combined with terms relating to organ donation. The searches were carried out in Medline, Embase, PsycINFO and EconLIT (See Supplementary Appendix). We also searched reference lists of relevant studies and reviews, dissertation and thesis databases and transplantation journals.
Included studies were examined for study eligibility by both K.H. and M.J.I.
Comprehensiveness of reporting
There is no universally accepted quality appraisal tool for qualitative research, therefore two reviewers (M.J.I. and K.H.) independently assessed each study for comprehensiveness of reporting, based broadly on the COREQ framework [ 14 ], and any disagreement was resolved by discussion. The assessment included details about the research team, the study methods, context of the study, analyses and interpretations ( Table 2 ).
Synthesis of findings
We performed a thematic synthesis of the results and conclusions reported by the primary author. We extracted from each paper all text under the headings ‘results/findings’ and ‘conclusion/discussion’. These were entered verbatim into Hyperresearch 2.8.3 (ResearchWare Inc., Randolph, MA) software. For each paper, two authors (M.J.I. and K.H.) independently coded the text and recorded concepts that focussed on (i) participants’ attitude towards organ donation; (ii) the reasons for participants’ beliefs and (iii) the interpretations given of participant perspectives on organ donation. A grounded theory [ 33 ] approach to analysis was used and further developed through negative case analysis [ 34 ]. To achieve a higher level of analytical abstraction, the concepts were examined for similarities, variations and relationships with one another. This informed the development of an analytical schema of themes.
Literature search and study descriptions
Our search yielded 3498 citations. Of these, 3320 were ineligible after title and abstract review. Of the potentially eligible 178 studies, 18 studies involving 1019 respondents were eligible to be included in the review ( Figure 1 ). Fourteen studies explored factors influencing attitudes towards both deceased and live organ donation. Two studies focussed on attitudes to live organ donation only and two studies focussed on deceased donation. Six studies employed focus groups, eight studies used interviews and four studies used both focus groups and interviews.

Search results.
Studies were conducted in the UK, Canada, USA, South Africa, Malta and Australia. Many of the studies included respondents from specific minority groups and focussed on barriers to donation ( Table 1 ).
Qualitative studies on community attitudes to organ donation
| Authors | Study reference | Country | Population | Minority group, Yes/No | Data collection | Donor type | Research topic | |
| Alkhawari | UK | 141 | Indo-Asians Muslims in the UK | Yes | Interviews and focus groups | Live/deceased | Attitudes to organ donation and transplantation | |
| Alvaro | USA | 52 | Spanish-Hispanics in Arizona | Yes | Focus groups | Live | Barriers and opportunities for living kidney donation | |
| Benghu | Africa | 48 | Zulu traditional healers and religious leaders | No | Interviews | Live/deceased | Cultural norms and social structures and their influence on organ donation | |
| Corlet | Canada | 60 | Donors, non-donors and ambivalent | No | Focus groups | Live/deceased | Attitudes to organ donation and transplantation | |
| Davis | UK | 120 | Black African/Caribbean | Yes | Focus groups | Live/deceased | Awareness and attitudes to organ donation | |
| Davis | UK | 120 | Black African/Caribbean | Yes | Focus groups | Live/deceased | Influence of religion on organ donation and transplantation | |
| Exley | UK | 22 | Sikh community | Yes | Interviews and focus groups | Live/deceased | Attitudes and beliefs on organ donation | |
| Fahrenwald | USA | 21 | American Indian adults in an Indian Reservation in South Dakota | Yes | Semi-structured interviews | Live/deceased | Sociocultural perspective on organ donation | |
| Griffin | USA | 12 | African American dialysis patient’s care givers | Yes | Face to face, interviews with Knowledge | Kidney live | Factors that influence relatives decision about kidney donation | |
| Lauri | Malta | 57 | General community | No | Focus groups | Deceased | Social representations the public has of organ donation | |
| Moloney | Australia | 29 | General community | No | Focus groups | Live/deceased | Contradiction between endorsement and donation | |
| Molzahn | Canada | 14 | Canadian aboriginals | Yes | Interviews | Live/deceased | Values and beliefs on organ donation | |
| Molzahn | Canada | 39 | Chinese Canadians | Yes | Interviews and focus groups | Live/deceased | Beliefs on organ donation | |
| Molzahn | Canada | 40 | Indo-Canadians | Yes | Interviews and focus groups | Live/deceased | Beliefs on organ donation | |
| Morgan | UK | 14 | Caribbean descent in London | Yes | Interviews | Live/deceased | How ethnicity shapes perceptions of identity and belonging that underpin organ donation | |
| Morgan | USA | 156 | General community—family pairs | No | Interviews | Deceased | Reasons for not signing an organ donor card | |
| Randhawa | UK | 64 | Asians in the UK | Yes | In-depth interviews | Live/deceased | Examining the influences to attitudes on organ donation | |
| Wittig | USA | 10 | African American women in Southern USA | Yes | Interviews | Live/deceased | Cultural care beliefs, meanings and practices regarding organ donation |
| Authors | Study reference | Country | Population | Minority group, Yes/No | Data collection | Donor type | Research topic | |
| Alkhawari | UK | 141 | Indo-Asians Muslims in the UK | Yes | Interviews and focus groups | Live/deceased | Attitudes to organ donation and transplantation | |
| Alvaro | USA | 52 | Spanish-Hispanics in Arizona | Yes | Focus groups | Live | Barriers and opportunities for living kidney donation | |
| Benghu | Africa | 48 | Zulu traditional healers and religious leaders | No | Interviews | Live/deceased | Cultural norms and social structures and their influence on organ donation | |
| Corlet | Canada | 60 | Donors, non-donors and ambivalent | No | Focus groups | Live/deceased | Attitudes to organ donation and transplantation | |
| Davis | UK | 120 | Black African/Caribbean | Yes | Focus groups | Live/deceased | Awareness and attitudes to organ donation | |
| Davis | UK | 120 | Black African/Caribbean | Yes | Focus groups | Live/deceased | Influence of religion on organ donation and transplantation | |
| Exley | UK | 22 | Sikh community | Yes | Interviews and focus groups | Live/deceased | Attitudes and beliefs on organ donation | |
| Fahrenwald | USA | 21 | American Indian adults in an Indian Reservation in South Dakota | Yes | Semi-structured interviews | Live/deceased | Sociocultural perspective on organ donation | |
| Griffin | USA | 12 | African American dialysis patient’s care givers | Yes | Face to face, interviews with Knowledge | Kidney live | Factors that influence relatives decision about kidney donation | |
| Lauri | Malta | 57 | General community | No | Focus groups | Deceased | Social representations the public has of organ donation | |
| Moloney | Australia | 29 | General community | No | Focus groups | Live/deceased | Contradiction between endorsement and donation | |
| Molzahn | Canada | 14 | Canadian aboriginals | Yes | Interviews | Live/deceased | Values and beliefs on organ donation | |
| Molzahn | Canada | 39 | Chinese Canadians | Yes | Interviews and focus groups | Live/deceased | Beliefs on organ donation | |
| Molzahn | Canada | 40 | Indo-Canadians | Yes | Interviews and focus groups | Live/deceased | Beliefs on organ donation | |
| Morgan | UK | 14 | Caribbean descent in London | Yes | Interviews | Live/deceased | How ethnicity shapes perceptions of identity and belonging that underpin organ donation | |
| Morgan | USA | 156 | General community—family pairs | No | Interviews | Deceased | Reasons for not signing an organ donor card | |
| Randhawa | UK | 64 | Asians in the UK | Yes | In-depth interviews | Live/deceased | Examining the influences to attitudes on organ donation | |
| Wittig | USA | 10 | African American women in Southern USA | Yes | Interviews | Live/deceased | Cultural care beliefs, meanings and practices regarding organ donation |
Comprehensiveness of reporting of included studies
The comprehensiveness of reporting of the included studies is described in Table 2 . All studies provided respondent quotations, details of sample sizes and a range and depth of insights into attitudes to organ donation. Twelve studies described the setting for data collection.
Comprehensiveness of reporting for included papers
| Study | [ ] | [ ] | [ ] | [ ] | [ ] | [ ] | [ ] | [ ] | [ ] | [ ] | [ ] | [ ] | [ ] | [ ] | [ ] | [ ] | [ ] | [ ] |
| Personal characteristics | ||||||||||||||||||
| Researcher identified | ||||||||||||||||||
| Credentials | ||||||||||||||||||
| Occupation | ||||||||||||||||||
| Sex | ||||||||||||||||||
| Experience and training | ||||||||||||||||||
| Relationship with participants | ||||||||||||||||||
| Participants selection | ||||||||||||||||||
| Sampling | ||||||||||||||||||
| Method of approach | ||||||||||||||||||
| Sample size | ||||||||||||||||||
| No. and reason for non-participation | ||||||||||||||||||
| Setting | ||||||||||||||||||
| Setting of data collection | ||||||||||||||||||
| Presence of non-participants | ||||||||||||||||||
| Description of sample | ||||||||||||||||||
| Data collection | ||||||||||||||||||
| Interview guide | ||||||||||||||||||
| Repeat interviews | ||||||||||||||||||
| Audio/visual recording | ||||||||||||||||||
| Field notes | ||||||||||||||||||
| Duration | ||||||||||||||||||
| Data or theoretical saturation | ||||||||||||||||||
| Transcripts returned to participants | ||||||||||||||||||
| Data analysis | ||||||||||||||||||
| No. data coders | ||||||||||||||||||
| Description of coding tree | ||||||||||||||||||
| Protocol for data preparation and transcription | ||||||||||||||||||
| Use of software | ||||||||||||||||||
| Reporting | ||||||||||||||||||
| Respondent quotations provided | ||||||||||||||||||
| Range and depth of insight into attitudes to organ donation | ||||||||||||||||||
| Range and depth of insight into cultural diversity |
| Study | [ ] | [ ] | [ ] | [ ] | [ ] | [ ] | [ ] | [ ] | [ ] | [ ] | [ ] | [ ] | [ ] | [ ] | [ ] | [ ] | [ ] | [ ] |
| Personal characteristics | ||||||||||||||||||
| Researcher identified | ||||||||||||||||||
| Credentials | ||||||||||||||||||
| Occupation | ||||||||||||||||||
| Sex | ||||||||||||||||||
| Experience and training | ||||||||||||||||||
| Relationship with participants | ||||||||||||||||||
| Participants selection | ||||||||||||||||||
| Sampling | ||||||||||||||||||
| Method of approach | ||||||||||||||||||
| Sample size | ||||||||||||||||||
| No. and reason for non-participation | ||||||||||||||||||
| Setting | ||||||||||||||||||
| Setting of data collection | ||||||||||||||||||
| Presence of non-participants | ||||||||||||||||||
| Description of sample | ||||||||||||||||||
| Data collection | ||||||||||||||||||
| Interview guide | ||||||||||||||||||
| Repeat interviews | ||||||||||||||||||
| Audio/visual recording | ||||||||||||||||||
| Field notes | ||||||||||||||||||
| Duration | ||||||||||||||||||
| Data or theoretical saturation | ||||||||||||||||||
| Transcripts returned to participants | ||||||||||||||||||
| Data analysis | ||||||||||||||||||
| No. data coders | ||||||||||||||||||
| Description of coding tree | ||||||||||||||||||
| Protocol for data preparation and transcription | ||||||||||||||||||
| Use of software | ||||||||||||||||||
| Reporting | ||||||||||||||||||
| Respondent quotations provided | ||||||||||||||||||
| Range and depth of insight into attitudes to organ donation | ||||||||||||||||||
| Range and depth of insight into cultural diversity |
Eight main themes emerged from the synthesis of the studies. These were relational ties, religious beliefs, cultural beliefs, family influence, body integrity, interaction with the health care system, knowledge and information about donation and the significant reservations for the support that many gave for organ donation.
Relational ties
I couldn’t understand anyone who could let their brother or their sister or their mother, father, continue to suffer or even possibly die when it’s within their means to help them. When you love someone that’s what you do. (Respondent) [ 12 ]
Religious beliefs
Our religion says do not waste things; if they [organs] can be utilized and used for the good of other people, then that item should not be thrown away. (Respondent) [ 31 ]
A large number of participants expressed their belief that Islam forbids organ donation, on the basis of statements from the Qur’an and traditional Islamic literature. (Author) [ 15 ]
‘ I don’t want half of my body buried and half to go to heaven. (Male Respondent) [ 19 ] After you die, you may go to another world. If you don’t have an eye, you cannot see. (Respondent) [ 27 ]
Cultural beliefs
Black people in general didn’t like to talk about death and were very private about particular matters. (Author) [ 20 ]
Some cultures believed that the spirit transferred from the donor to the recipient and others discussed the need for ancestral approval before donation, so that the remaining family did not lose ancestral protection in the future. Others highlighted the importance of particular rituals to do with the grieving process and that organ donation was seen to interfere in this process [ 26 ]. Some spoke about the change in traditional cultural beliefs over time and how younger generations were deciding to become donors.
Family influence
I personally have no objection but my father does, so I am not sure … . (Respondent, Female, 20) [ 15 ]
Some felt they had to ask permission from family members. Some also felt that a definite decision, from family members regarding donation, would ensure that loved ones were not burdened later with a difficult choice. Some felt that organ donation would interfere with the grieving process for families.
Body integrity
To be honest with you I do care what happens to my body after I die, I may be dead but it’s still my body and I want it to look right and be treated right. (Respondent, Female) [ 30 ] I'd sign, but my wife and children object. The children don't like to see daddy cut up. (Respondent, Male) [ 18 ]
I would not donate my eyes, ever, because of the ceremony prior to cremation when people come to the funeral to see the body. I don’t want to not have any eyes. (Respondent) [ 31 ]
Interaction with the health care system
How fast is the decision made? Are you really dead? Who makes the decision? (Respondent) [ 18 ] . . . They’ll start gutting you up like a deer. (Respondent) [ 29 ]
Sorry to say, but we all think it’s for the whites and not us because whenever we see pictures on TV about people receiving transplants they are always white. So we think we are not part of a culture who needs donors or organs. (Respondent, Female aged 18–30 years, African) [ 19 ]
Level of knowledge and information on organ donation
A number of people expressed concern about the lack of information available concerning organ donation. Over time, ‘urban myths had been translated into what people perceived to be correct information and had subsequently resulted in fears about donation. (Author) [ 19 ]
One study, though, indicated that participants would still choose not to donate even if they had more information about the process, as their belief system did not support donation [ 18 ].
Participants’ reservations despite positive beliefs
Overwhelmingly … people cited the amazing potential of organ donation to help people who are suffering … However, these same people went on to voice serious misgivings about organ donation, especially about institutions and individuals involved with the process of organ donation. (Author) [ 29 ]

Balance of attitudes to organ donation.
We identified eight major themes regarding community attitudes towards organ donation. Many made decisions regarding organ donation based on personal beliefs (religious, cultural, family, social and body integrity), levels of knowledge about organ donation and previous interaction with the health care system. Many maintained positive attitudes to organ donation despite significant reservations about the organ donation process. Resistance to donation tended to be less in the case of living donation for family.
There are some limitations in this study. Although we set out to synthesize community attitudes to organ donation, 13 of the 18 included papers were specifically designed to elicit barriers to organ donation from ethnic or cultural groups with previously known low donation rates. Consequently, the results of this review are perhaps skewed towards the negative influences on the organ donation process.
Previous research tells us that religious beliefs are often associated with being a non-donor [ 3 , 5 , 6 , 12 , 13 ]. In this study, we find that some religious beliefs could also be positive influences and where negative beliefs were present, these often stemmed from uncertainty or misrepresentation of religious edicts. One solution would be for the transplant community to more actively engage religious leaders, especially when it has been reported that, across the major religions, there are very few cases where organ donation can be seen to be inconsistent with religious edicts [ 35 ]. Religious leaders could be made available in hospitals to assist families in making decisions regarding organ donation and potentially debunk misperceptions. Staff members who have a role in approaching families to request consent for donation could also be more effective through awareness programmes and resources about religious concerns.
Similarly, cultural sensitivity to issues such as apprehensiveness to discuss death among certain groups or individuals and the importance to many of death rituals may improve dialogue regarding organ donation. Studies have shown that engaging some minority groups in the health care system and creating a sense of belonging and ownership can improve compliance with health interventions [ 36 ]. As a consequence, efforts should be made to create positive interactions within the health care system, especially for minority groups, to improve donation rates.
Although many qualitative studies have found that higher socio-economic status and education were associated with a stronger willingness to be an organ donor [ 2 , 3 , 5 ], little can be discerned directly from these studies as to the reasons why. However, issues of alienation, as highlighted in relation to ethnic minorities, and of ignorance are likely to be at play. This suggests that programmes to better engage disadvantaged communities particularly through targeted information campaigns would be worth considering. Some of the strong reservations held, even among those with generally positive views towards donation, such as concerns that agreeing to donation would discourage doctors from caring so much about saving their lives in an emergency or that it would result in the premature removal of their organs or indeed prevent them from having an open coffin at their funerals, are examples of very real barriers that can be readily addressed through information.
The organ donation decision is a complex one, based strongly on personal beliefs. There are some factors, such as religious and cultural beliefs, that are seemingly intractable and are often cited as reasons for a refusal to donate. In this review of qualitative studies, it is shown that these have often been found to be tied in with more complex issues such as a distrust of the medical system, misunderstandings about religious stances and ignorance about the donation process. Interventions to better engage the community, including disadvantaged and minority groups, to foster trust and provide information represent promising opportunities of promoting organ donation in the future.
Supplementary Appendix is available online at http://ndt.oxfordjournals.org .
This work was funded by Australian Research Council Discovery Project Grant (DP0985187).
Conflict of interest statement . None declared.
Google Scholar
Google Preview
- organ donation
- health care systems
- personal integrity
| Month: | Total Views: |
|---|---|
| November 2016 | 1 |
| January 2017 | 59 |
| February 2017 | 210 |
| March 2017 | 177 |
| April 2017 | 106 |
| May 2017 | 72 |
| June 2017 | 68 |
| July 2017 | 33 |
| August 2017 | 43 |
| September 2017 | 105 |
| October 2017 | 107 |
| November 2017 | 254 |
| December 2017 | 842 |
| January 2018 | 826 |
| February 2018 | 1,090 |
| March 2018 | 1,496 |
| April 2018 | 1,401 |
| May 2018 | 1,734 |
| June 2018 | 973 |
| July 2018 | 736 |
| August 2018 | 1,111 |
| September 2018 | 884 |
| October 2018 | 1,030 |
| November 2018 | 1,466 |
| December 2018 | 1,028 |
| January 2019 | 835 |
| February 2019 | 1,005 |
| March 2019 | 1,279 |
| April 2019 | 1,230 |
| May 2019 | 1,396 |
| June 2019 | 1,471 |
| July 2019 | 1,393 |
| August 2019 | 1,490 |
| September 2019 | 1,002 |
| October 2019 | 668 |
| November 2019 | 499 |
| December 2019 | 339 |
| January 2020 | 372 |
| February 2020 | 366 |
| March 2020 | 520 |
| April 2020 | 437 |
| May 2020 | 213 |
| June 2020 | 302 |
| July 2020 | 261 |
| August 2020 | 287 |
| September 2020 | 322 |
| October 2020 | 509 |
| November 2020 | 507 |
| December 2020 | 408 |
| January 2021 | 323 |
| February 2021 | 435 |
| March 2021 | 663 |
| April 2021 | 460 |
| May 2021 | 439 |
| June 2021 | 336 |
| July 2021 | 343 |
| August 2021 | 420 |
| September 2021 | 422 |
| October 2021 | 416 |
| November 2021 | 411 |
| December 2021 | 282 |
| January 2022 | 305 |
| February 2022 | 301 |
| March 2022 | 680 |
| April 2022 | 412 |
| May 2022 | 274 |
| June 2022 | 177 |
| July 2022 | 184 |
| August 2022 | 202 |
| September 2022 | 228 |
| October 2022 | 373 |
| November 2022 | 373 |
| December 2022 | 316 |
| January 2023 | 255 |
| February 2023 | 206 |
| March 2023 | 323 |
| April 2023 | 281 |
| May 2023 | 265 |
| June 2023 | 203 |
| July 2023 | 238 |
| August 2023 | 187 |
| September 2023 | 281 |
| October 2023 | 398 |
| November 2023 | 370 |
| December 2023 | 251 |
| January 2024 | 385 |
| February 2024 | 496 |
| March 2024 | 579 |
| April 2024 | 427 |
| May 2024 | 394 |
| June 2024 | 272 |
| July 2024 | 269 |
| August 2024 | 206 |
| September 2024 | 147 |
Email alerts
Citing articles via.
- ndt Twitter
- ERA Twitter
- ERA Facebook
- ERA Instagram
- ERA LinkedIn
- Recommend to Your Librarian
Affiliations

- Online ISSN 1460-2385
- Print ISSN 0931-0509
- Copyright © 2024 European Renal Association
- About Oxford Academic
- Publish journals with us
- University press partners
- What we publish
- New features
- Open access
- Institutional account management
- Rights and permissions
- Get help with access
- Accessibility
- Advertising
- Media enquiries
- Oxford University Press
- Oxford Languages
- University of Oxford
Oxford University Press is a department of the University of Oxford. It furthers the University's objective of excellence in research, scholarship, and education by publishing worldwide
- Copyright © 2024 Oxford University Press
- Cookie settings
- Cookie policy
- Privacy policy
- Legal notice
This Feature Is Available To Subscribers Only
Sign In or Create an Account
This PDF is available to Subscribers Only
For full access to this pdf, sign in to an existing account, or purchase an annual subscription.
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
The PMC website is updating on October 15, 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Ann Transplant

Knowledge and Ethical Issues in Organ Transplantation and Organ Donation: Perspectives from Iranian Health Personnel
Mahmoud abbasi.
1 Medical Ethics and Law Research Center, Shahid Beheshti University of Medical Sciences, Tehran, Iran
Mehrzad Kiani
2 Department of Medical Ethics, Faculty of Traditional Medicine, Shahid Beheshti University of Medical Sciences, Tehran, Iran
Mehdi Ahmadi
3 Razi Vaccine and Serum Research Institute (RVSRI), Agricultural Research, Education and Extension Organization (AREEO), Karaj, Iran
Bahare Salehi
Organ transplantation is one of the most critical topics in medical ethics that is commonplace in various countries. This study aimed to evaluate the knowledge and the ethical issues surrounding organ transplantation and organ donation among healthcare personnel in Tehran, Iran.
Material/Methods
In a cross-sectional study performed on 450 healthcare personnel, self-administered questionnaires were used to derive data from individuals. Among the 450 health personnel who received the questionnaires, 377 completed their questionnaires (83.77%).
The willingness and unwillingness to donate organs among individuals were 47.48% ( n =179) and 52.51% ( n =198), respectively. Among the individuals who signed the organ donation card, 96.5% ( n =55) were willing to donate their organs and 3.5% ( n =2) were unwilling to donate their organs. Most of the individuals that were willing (48.34%; n =175) and unwilling (51.66%; n =187) to donate their organs claimed religious support for organ donation ( P =0.00). Out of these people, 110 willing people (67.48%) and 53 (32.52%) unwilling people were familiar with the idea of brain death. The individuals who selected cadavers (67.64%; n =255) and brain death (24.4%; n =92) were chosen as the best candidates for organ donation. Most individuals believed that young patients ( n =123; 32.62%) and people who had not already had organ transplants ( n =90; 23.87%) should be the preferred recipients of organs. Most individuals had learned about organ transplantation from television (30.24%; n= 114), newspapers (23.61%; n =89), and the radio (19.89%; n =75).
Conclusions
In conclusion, there is a need for more educational programs for the improvement of knowledge and ethical consideration with regard to organ transplantation and organ donation among healthcare personnel.
The transplantation of human organs in the case of the irreversible failure of an organ has been raised for a long time in scientific and social committees, and this topic has been addressed from scientific, moral, religious, political, and legal perspectives [ 1 – 4 ]. Organ donation options, such as the heart, lungs, kidneys, the liver, and the eyes, from a patient with brain death before cardiac arrest, are particularly important because these organs can save another patient’s life. Organ transplantation is one of the most critical topics explored in medical ethics, which is presently commonplace in many countries. Owing to the prevalence of organ transplants in the world, various issues need careful attention from researchers. Organ transplantation within the study of medical ethics contains hundreds of topics.
Ethics, at its foundation, considers the values, ideas, traditions, and practices of a community or an individual [ 5 ]. Thus, any action in opposition to these concepts is deemed to be unethical [ 6 ]. Recently, transplantation has seen improvements across its various features; it can be performed in most regions of the world, including Asian countries [ 7 – 9 ]. In most western nations, voluntary consent is required for organ transplants [ 10 , 11 ]. The demand for organ transplantation has quickly increased during the past decade in many countries. Owing to the increased incidence of organ failure, growing success and significant improvement have become prevalent in post-transplant results. Nevertheless, the lack of adequate organs for transplantation to meet the existing demand has resulted in substantial organ-shortage crises as a result of an increase in the critical conditions of certain patients on transplant waiting lists, as well as in the number of patients deaths while waiting [ 12 – 14 ].
In Islamic countries, many religious scholars have allowed organ transplantation [ 15 , 16 ]. The ethical verdict on organ transplantation is disputable and varying. Therefore, opinions about organ transplantation depend on personal opinions, as well as religious and geographical reasons, and involve economic, emotional, and socio-cultural factors, which deserve discussion and study [ 17 ]. The Islamic Republic of Iran is one of the countries in which Islam is the dominant religion. In Iran, the organ donation law was first passed in 2000 by the Islamic Consultative Assembly. From 2001 to 2010, reports from Iran showed a notably increasing rate of transplantation from cadaveric organs [ 18 ]. It seems logical that all countries and regions need to promote expansion of the yield of organs for transplantation. Healthcare knowledge has exposed a key reason for the success or the failure of organ transplantation plans [ 19 ]. One way to reach this aim involves focusing on the knowledge of healthcare workers. The lack of knowledge among healthcare workers has been recognized as a barrier and is essential to successful organ donation [ 20 ]. The objective of the present study was to evaluate the knowledge, the willingness, and the ethical considerations of healthcare personnel with regard to organ transplantation and organ donation in Tehran, Iran.
Material and Methods
This was a cross-sectional study in the hospitals of Tehran, Iran. Data were collected from 2016 to 2017. The survey was carried out by a self-administered questionnaire given to healthcare personnel, which included patient care assistants, security, pharmacists, managers, culinary staff, and nutritionists, and excluded doctor and nurses. The questionnaire form was prepared with 4 parts: socio-demography, knowledge, willingness for organ donation, and ethical beliefs about organ transplantation and organ donation. The educational qualifications of individuals in this study were classified arbitrarily as ‘medium’ (Diploma, Associate, and Bachelor degrees) or ‘high’ (Master’s and Ph.D. degrees). The knowledge of respondents was evaluated through scores of correct responses to questions. In addition, we considered extra questions about the willingness to donate as well as ethical issues for individuals. All the questionnaires were in printed format and the survey was self-administered. During distribution to individuals, we directed the participants to only select 1 response to each query. We assigned a code number for each questionnaire to allow computerized data entry. This study was approved by the Research Ethics Committee of Shahid Beheshti University of Medical Sciences, Tehran, Iran.
Statistical analysis
All the data were entered into a dedicated SPSS database (IBM SPSS Statistics for Windows, Version 11.5; IBM, Armonk, New York). The analysis was carried out with the use of the aforementioned software. We used the chi-square test for the analysis of proportions of categorical variables. The independent-samples Student’s t test was used to compare the means for 2 groups of variables. P <0.05 was considered significant. The missing responses to specific questions in the completed questionnaires were coded as missing. Percentages were calculated from the total number of respondents, including those with missing responses.
Socio-demographic characteristics of individuals and healthcare levels
We shared 450 questionnaires among the healthcare personnel. We received 377 completed questionnaires (response rate=83.77%). The socio-demographic characteristics of individuals and healthcare levels are shown in Table 1 . Most of the individuals were female (55.7%; n= 210), single or married (55.04%; n= 120, and 56.6%; n= 90, respectively), and had children (56%; n= 70). Most were less than 35 years (60.21%; n= 227), with 43.17% ( n= 98) males and 56.83% ( n = 129) females. The medium education level had the highest frequency among all participants (66.04%; n =249).
Socio-demographic factors among healthcare personnel.
| Characteristics | Male, n (%) | Female, n (%) | -value |
|---|---|---|---|
| Age | |||
| Less than 35 years old | 98 (43.17) | 129 (56.83) | 0.145 |
| Between 35 and 40 years old | 49 (43.36) | 64 (56.64) | |
| Older than 41 years | 20 (54.05) | 17 (45.95) | |
| Educational level | |||
| Medium | 127 (51) | 122 (49) | 0.14 |
| High | 40 (31.25) | 88 (68.75) | |
| Marital status | |||
| Single | 98 (44.96) | 120 (55.04) | 0.041 |
| Married | 69 (43.4) | 90 (56.6) | |
| Parenthood | |||
| Parent | 55 (44) | 70 (56) | 0.023 |
| Nonparent | 14 (41.18) | 20 (58.82) | |
Willingness and knowledge of healthcare personnel about organ donation
The effect of the characteristics on the willingness towards organ donation among healthcare personnel is shown in Table 2 . The individuals were divided into willing to donate (47.48%; n =179) and unwilling to donate (52.51%; n =198). The category comprising willing to donate organs was higher among females (54.29%; n =114), married people (65.69%; n =134), and individuals with a high level of education (92.38%; n =109). The results showed that the years spent working in healthcare does not significantly affect the willingness to be an organ donor ( P =0.45). Out of all the individuals who signed the organ donation card, 96.5% ( n =55) were willing to donate their organs and 3.5% ( n =2) were unwilling to donate their organs. Most individuals did not know anyone who had donated an organ. Only 40 (76.93%) individuals among the willing-to-donate category and 12 (23.07%) individuals among the unwilling-to-donate category knew someone who had donated an organ. The willingness of individuals to donate blood showed that there was no significant difference between the willingness to donate and the unwillingness to donate ( P =0.24). All the individuals were Muslims and most of the people willing to donate organs (48.34%; n =175) and the people who were unwilling to donate organs (51.66%; n =187) claimed that their religion supports organ donation ( P =0.00). With respect to the concept of brain death, 110 (67.48%) of the participants who were willing to donate and 53 (32.52%) of the participants who were unwilling to donate, were familiar with the concept of brain death. Among the participants, 173 participants (77.23%) who were willing to donate and the 51 participants (22.77%) who were unwilling to donate claimed to know somebody who was waiting for transplantation ( P= 0.01).
Characteristics affecting the willingness to donate organs among healthcare personnel.
| Factors | Willingness to donate | -value | |
|---|---|---|---|
| Yes, n (%) | No, n (%) | ||
| Gender | |||
| Male | 65 (38.92) | 102 (61.08) | 0.00 |
| Female | 114 (54.29) | 96 (45.71) | |
| Marital status | |||
| Single | 45 (26.01) | 128 (73.99) | 0.03 |
| Married | 134 (65.69) | 70 (34.31) | |
| Education Level | |||
| Medium | 70 (27.03) | 189 (72.97) | 0.01 |
| High | 109 (92.38) | 9 (7.62) | |
| Years working in healthcare environment | |||
| <1 | 24 (40) | 36 (60) | 0.45 |
| 1–5 | 25 (29.77) | 59 (70.23) | |
| 6–10 | 46 (41.81) | 64 (58.19) | |
| 11–15 | 46 (65.71) | 24 (34.29) | |
| >15 | 38 (71.7) | 15 (28.3) | |
| Have you received an organ donation card? | |||
| Yes | 55 (96.5) | 2 (3.5) | 0.00 |
| No | 124 (38.75) | 196 (61.25) | |
| Knowing anyone who had donated organ | |||
| Yes | 40 (76.93) | 12 (23.07) | 0.00 |
| No | 139 (42.76) | 186 (57.24) | |
| Willingness to donate blood | |||
| Yes | 156 (64.46) | 86 (35.54) | 0.24 |
| No | 23 (17.03) | 112 (82.97) | |
| Does one’s religion support organ donation? | |||
| Yes | 175 (48.34) | 187 (51.66) | |
| No/unsure | 4 (26.66) | 11 (73.34) | 0.00 |
| Understand the concept of brain death | |||
| Yes | 110 (67.48) | 53 (32.52) | 0.01 |
| No | 69 (32.24) | 145 (67.76) | |
| Knowing somebody waiting for transplantation | |||
| Yes | 173 (77.23) | 51 (22.77) | 0.01 |
| No | 6 (3.92) | 147 (96.08) | |
Ethical considerations of healthcare personnel with respect to organ donation
The individual’s perspective on the ideal candidate for organ donation is shown in Table 3 . One hundred and twenty-six (33.42%) males and 129 (34.21%) females regarded cadavers as the best candidates for organ donation ( P =0.032). In addition, brain death was selected by 37 (9.81%) males and 55 (14.58%) females as an acceptable source of organ donation. Furthermore, 3 individuals agreed on organ reception from an animal ( P =0.03). Two individuals believed that a paralyzed person was a good candidate for organ donation ( P =0.00). The perspective of individual preference for a received organ is shown in Table 4 . Organ transplants for young patients ( n =123; 32.62%) and people who have not already had organ transplants ( n =90; 23.87%) were given the greatest preference for organ reception. Sixty-five (17.24%) males selected anyone who has not already had an organ transplant as the preferred group, while 88 (23.34%) females regarded young patients as their preferred choice for who should receive an organ.
Perspectives of individuals with regard to the characteristics of ideal candidate for organ donation.
| Characteristics | All, n (%) | Male, n (%) | Female, n (%) | -value |
|---|---|---|---|---|
| Healthy person | 25 (6.63) | 5 (1.32) | 20 (5.3) | 0.001 |
| Cadaver (organ donation after death) | 255 (67.64) | 126 (33.42) | 129 (34.21) | 0.032 |
| Paralyzed person | 2 (0.53) | 1 (0.26) | 1 (0.0.26) | 0.00 |
| Brain death | 92 (24.4) | 37 (9.81) | 55 (14.58) | 0.001 |
| Animal | 3 (0.79) | 2 (0.53) | 1 (0.26) | 0.03 |
Perspective of individuals with regard to preference for the recipient of an organ.
| Characteristics | All, n (%) | Male, n (%) | Female, n (%) | -value |
|---|---|---|---|---|
| Priority in organ transplants with those who have not already had organ transplants | 90 (23.87) | 65 (17.24) | 25 (6.63) | 0.003 |
| Priority in organ transplant with young patients | 123 (32.62) | 35 (9.28) | 88 (23.34) | 0.02 |
| Low-income patients | 45 (11.93) | 14 (3.71) | 31 (8.22) | 0.03 |
| Those who have organ damage due to illness | 32 (8.48) | 8 (2.12) | 24 (6.36) | 0.04 |
| Priority when those who are waiting a long time for organ transplants | 87 (23.07) | 39 (10.34) | 48 (12.73) | 0.001 |
Information sources of healthcare personnel on organ transplantation
The healthcare personnel who participated in this study heard about organ transplantation from television (30.24%; n =114), newspapers (23.61%; n =89), the radio (19.89%; n =75), the Internet (10.08%; n =38), doctors (6.63%; n =25), friends/colleagues (1.59%; n =6), and others sources (7.96%; n= 30) ( Figure 1 ).

Information sources of individuals with regard to organ transplantation.
Organ transplantation brings up troublesome ethical issues about an individual’s claims in figuring out what happens to their bodies prior to and after death. In the present study, we found that 47.48% of healthcare personnel were willing to be organ donors. Those belonging to the willing-to-donate category cited the human spirit as the most important reason for donation. We found that women and individuals with higher education were more likely to consent to organ donation than men and individuals with a less education. This result was similar to the findings of Popp et al. [ 21 ] in their assessment of the readiness for living liver donation among the general German population. Alvaro et al. [ 22 ] carried out a study on the predictors of organ donation behavior among Hispanic Americans. The results of this study showed that women were more likely to consent to organ donation than men. Oluyombo et al. [ 23 ] reported that only 29.5% of healthcare workers in south-west Nigeria were willing to donate an organ, even though there was a high level of awareness (93%) and knowledge (82.5%) about organ donation. Unlike our study, Yilmaz [ 24 ] reported that people with higher education tended to have sceptical attitudes towards organ donation. Education level is one of the most important causes that can influence organ donation decisions. In our study, individuals with a higher level of education were more likely to donate and they were less fearful of organ donation. It is clear that people with a higher level of education have a better understanding that organ transplantation can save lives.
In our study, 30.72% of individuals who were willing to donate signed the organ donation card. Schut [ 25 ] reported that only about 7–10% of all the individuals in Germany who are in favor of organ donation carry a donor card. Akqun et al. [ 26 ] performed a study on the knowledge and the personal views of Turkish healthcare professionals, showing that 44.2% of healthcare personnel were willing to donate, but only 17.9% carried donor cards. Agreements to sign organ donation cards suggest body mutilation at the point of death or after, which, in the eyes of many, is taboo and against personal beliefs. Most individuals in our study had not signed donation cards, mostly due to ignorance and inaccurate information. This implies the need to motivate and encourage positive attitudes through appropriate advertising [ 23 ]. In the last year in Iran, 3438 organs were transplanted from dead donors. Recently, around 1.8 million individuals have been issued voluntary organ donation cards in Iran. Every donor can save up to 10 individual lives. Although the willingness to donate the organs of patients with brain death has lately expanded in Iran, more plans should be created to encourage more individuals to become organ donors.
We found that 52.51% of individuals were unwilling to be an organ donor. Previous studies reported some reasons why individuals are unwilling to donate their organs, and indicated that the reasons are complicated [ 27 ]. The results of our study show that certain reasons, traditions, and socio-cultural beliefs make a person unwilling to donate his organs.
Morgan et al. [ 27 ] reported that one of the most important factors affecting organ donation was religion. Sunni and Shi’i are the 2 major branches of Islam, with an overwhelming majority (90%) of Iranians practicing Shi’i Islam, which is the official religion of Iran. Most Islamic religious leaders have acceptant attitudes towards organ donation during life, but certain religious leaders do not believe brain death is an acceptable criterion for donor status, and consider the cessation of all signs of life, including the heartbeat, as a precondition for declaring death [ 28 ]. Religion is an essential part of life for many Asians [ 29 ]. Dehghani et al. [ 30 ] studied the causes of organ donation refusal in southern Iran. They reported a high level of family refusal to allow their relatives to donate organs due to belief that the definition of brain death is obscure and because miracles could still occur and a brain-dead person could recover. For efficient and successful transplanting, health authorities should organize useful debates involving different religious leaders, as they have a significant influence on the clientele of healthcare institutions [ 23 ].
In the present study, individuals indicated that cadavers and brain death are the best candidates for organ donation. Ali et al. [ 31 ] evaluated the knowledge and the ethical views on organ donation among medical students in Pakistan, showing that cadavers, healthy living donors, and brain-death groups were seen as good candidates for organ donation. In recent times, when people die, their organs may be donated if the individual had consented to do so before dying. A person is considered dead once either the heart stops beating or the brain’s function ceases (called brain death). After death, the organs are taken from the body of deceased individuals so that one cadaveric donor can donate organs to a few unique individuals.
In our study, 3 individuals agreed with the use of an animal as a source of organ donation. The main risk associated with organ transplantation from animals to humans is the presence of infectious agents in the transplanted organ and its transference to the recipient, and, eventually, the general population. Predictions such as the likelihood of transmission of disease during organ transplants from animals to humans are difficult to make because the medical community is not equipped to test for any pathogens that can be transferred through this type of transplant. In addition, animal pathogens agents may combine with human pathogens; this can create a new form of patient-specific disease. Mental and psychological issues are essential during organ transplantation from an animal. The human psyche is unpredictable and it is impossible to examine all its dimensions. Only a long-term study can identify the impact on a person. Therefore, the issues raised are more theoretical and its scientific evaluation needs sophisticated studies. Religion plays an essential role in the lives, lifestyles, eating habits, and medical treatments of people. Islam allows organ transplantation from animals to humans as there is no prohibition, unless it has a harmful effect (which is forbidden and unlawful) and is not banned under Islamic law. Based on the studies of researchers and clinical trials of scientists, it seems that organ transplantation from animals to humans will become commonplace. There is no need to lose precious time while patients are waiting on the transplant list. However, human organs will still be needed in the future.
In our study, young patients and people who had not already had organ transplants were the most preferred category for the reception of organs among individuals. Ali et al. [ 31 ] reported that most of the students who participated in their study agreed on the young age group of patients as the preferred group for organ reception due to a desire to increase the life expectancy of younger people. In addition, most individuals believed in equal conditions for organ transplants (i.e., priority should be given to people who have not already had an organ transplant rather than those who have already had organ transplants). They stated that it is not fair for a person to receive an organ several times and another person not to receive an organ even once.
In our study, most individuals had heard about organ donation from television. In recent years, television programs in various countries have dealt with organ transplantation in their storylines in different ways. Weber et al. [ 32 ] carried out a study on the impact of television on attitudes towards organ donation in a sample of the German urban population. They reported that the assumption that TV had a negative impact on donation rates must be rejected. Therefore, a stagnation or decline in donation rates must be blamed on other reasons. Saleem et al. [ 33 ] studied the knowledge, attitudes, and practices regarding organ donation among a selected adult population in Pakistan. They showed that television, print media, and doctors fall in the same order of frequency in being information sources for organ donation. Majidi and Aghaee [ 34 ] studied the role of television in the spread of ideas about organ donation from the perspective of families who donated organs. They found that television documentaries showing donors and recipient families had the most significant role in encouraging donators. The current broadcast of a scene on the advancement of organ donation and its significance in a favorite primetime television reality show caused an influx of reactions, with volunteers signing up for organ donation; this broke every record. In the 48 hours after the scene was broadcast on the family television show ‘Khandevaneh’, nearly 68 000 individuals went to the entrance of the Iranian Society for Organ Donation and signed up for organ donation. A typical strategy to spread awareness is mass communication; this involves creating prominent recognition through education campaigns or public messages on issues that enhance volunteerism.
This study showed that most of the healthcare personnel want to promote organ donation. We found that organ donation knowledge is correlated to the education level and the socioeconomic status of individuals. Our findings show that television, newspapers, and radio can be efficient sources of information. Religious scholars are exceedingly importatnt in mobilizing favorable public opinion towards organ donation. Policymakers should involve religious scholars to promote organ donation. Further studies should be carried out to elucidate the reasons behind attitudes against organ donation among healthcare personnel. This information will guide any future approach towards overcoming the inconsistency between the willingness to donate and unwillingness to donate. In this study, we used a quantitative tool to evaluate the willingness to donate among healthcare personnel in Tehran. Our analysis is a vital baseline document for further studies and a qualitative tool that can be used by future researchers.
In summary, Iran has the third highest rates of organ donation in the world and is the only nation that has addressed the shortage of transplant organs through a legal payment system for organ donation since 1988. It is also the only nation in which organ exchange is authorized. Undoubtedly, organizing and coordinating organ transplantation through the comprehensive organ transplantation system needs purposeful development through the extensive and rapid growth of organ transplantation in Iran. It must have an adequate level of organization for study and prediction, policymaking and planning, implementation, and monitoring education and research on medical organ transplantation.
Acknowledgements
This paper was part of the Ph.D. thesis of Dr. Bahare Salehi supervised by Dr. Mahmoud Abbasi and Dr. Mehrzad Kiani and advised by Dr. Mehdi Ahmadi.
Conflicts of interest
Source of support: This study was financially supported by the Vice-chancellor for Research Affairs of Shahid Beheshti University of Medical Sciences, Tehran, Iran

IMAGES
COMMENTS
Background. Organ transplantation (OT) is one of most successful advances in modern medicine. For patients with end stage disease, transplantation most often provides their only chance for survival. Even before the first transplant was performed, it was clear that OT could only be successful with a multidisciplinary approach.
Organ donation provides a life-giving, life-enhancing opportunity to those who are at the end of the line for hope. And the need for organ donors is growing. When Donna Lee died in 1992, there were 27,000 people on the transplant wait list. When Vikki died just four years later, that number had grown to 47,000 (Unpublished data, OPTN, January ...
Organ transplantation is a procedure in which a functional, intact organ is transferred from one individual to another. ... A new paper describes the development of genetically 'humanized ...
Over the past decade, the number of organ transplants performed worldwide has significantly increased for patients with advanced organ failure [1,2,3,4,5].In the United States, 41,354 organ transplants were performed in 2021, increasing by 5.9% compared to 2020 [].While there have been significant improvements in the short-term survival of solid organ transplant recipients due to advances in ...
Organ transplantation (OT) is one of most successful advances in modern medicine. For patients with end stage disease, transplantation most often provides their only chance for survival. ... Isolated islet transplantation is being performed with increasing frequency and is the topic of much ongoing research. Intestinal transplantation. The ...
Compared with opt-in systems, opt-out systems are associated with higher donor rates ranging from 23.3% to 61.5% according to some studies 106, 107. However, a 2019 study of 35 countries found no ...
Ethical Challenges of Organ Transplantation: Current Debates and International Perspectives. Bielefeld: Transcript Verlag. ISBN 978-3-8376-4643-6 ... Another avenue for future research is the impact of the COVID-19 pandemic. Briefly discussed in chapters 16 and 18, the pandemic has more recently prompted ethical issues in organ transplantation ...
Qualitative research has provided insights into why socioeconomic inequities in access and barriers to organ donation and transplantation exist, why patients are nonadherent to immunosuppressive regimens, how patients experience and cope with the complex psychosocial outcomes of transplantation, and patient attitudes toward increased risk, or ...
"Ethical Challenges of Organ Transplantation: Current Debates and International Perspectives" is a tour de force of the complex ethical issues faced in the field of solid organ transplantation. The editors of this book are Solveig Hansen, a PhD bioethicist and Silke Schickantz, a professor of Medical Ethics and History. As expected from the background of the editors, many of the chapters ...
Browse the latest research articles on organ transplantation, including kidney, liver, heart and lung transplantation. Find topics such as immunosuppression, metabolism, infection, donor acceptance and more.
Organ donation and transplantation encompass a broad spectrum of social, religious, ethical, medical and legal issues. 7 Across and within jurisdictions, there is a plurality of opinion in how best to address organ shortage and to prevent exploitation of vulnerable individuals. In this paper we explore key ethical and legal issues as they ...
Solid organ transplant recipients are at greater risk of infection than the non-immunosuppressed population (Table 3) . Infections are the most common non-cardiovascular causes of mortality following kidney transplantation, accounting for 15%-20% of mortality [131,135]. The first six months post-transplant is the time of greatest infection risk.
Survival after lung transplantation has significantly improved during the last two decades. The refinement of the already existing extracorporeal life support (ECLS) systems, such as extracorporeal membrane oxygenation (ECMO), and the introduction of new techniques for donor lung optimization, such as ex vivo lung perfusion (EVLP), have allowed the extension of transplant indication to ...
This study assessed the knowledge, attitude and willingness of undergraduate medical students towards organ donation at Jimma University. It found a high level of knowledge but a low level of positive attitude and willingness, and identified some factors that influenced organ donation.
Abstract. This report provides recommendations from the Research and Innovation domain as part of the International Donation and Transplantation Legislative and Policy Forum (hereafter the Forum) to provide expert guidance on the structure of an ideal organ and tissue donation and transplantation system. The recommendations focus on deceased ...
This is very much the case in the question of brain death. What sustains the debate on the ethical side are two convictions shared by most people engaged in the field: First, that transplantation of human organs from dead patients is a highly beneficial practice which should be extended rather than restricted.
Importance: The disparity between patients awaiting organ transplantation and organ availability increases each year. As a consequence, organ trafficking has emerged and developed into a multibillion-dollar-a-year industry. Objective: To identify and address barriers to organ donation in the United States and globally. Evidence review: Evidence-based peer-reviewed articles, including ...
These include organ donors, families of the deceased, organ recipients, patients on transplant waitlists, donation and transplantation professionals, and organ donation organizations. Given that donation research may impact the distribution of scarce healthcare resources, organ allocation, and public trust, society at large may also be affected.
Donation refers to donating human cells, tissues, or organs. intended for human applications. The donor is a human being, living or deceased, who is a source of cells, tissues, or organs. for the ...
This systematic review synthesizes 18 qualitative studies that explored factors influencing the decision to be an organ donor. It identifies eight themes, such as relational ties, religious beliefs, cultural influences and medical mistrust, that shape people's views and behaviours.
The NHS Blood and Transplant Service has recently told the BBC that over the past 5 years more than 500 families in the UK have blocked organ donation from a deceased relative, despite them being on the organ donor register. In the USA, more than 117 000 people await an organ transplant, says a report from the National Academy of Sciences (NAS) on the Opportunities for Organ Donor Intervention ...
Organ transplantation may be considered a miracle of twentieth century medicine. By increasing life expectancies and improving the quality of life, it remains the best therapy for terminal and irreversible organ failure. The introduction of antibiotics, massive vaccinations of the general population to prevent infectious diseases, and organ ...
Aim:To understand what influences the decision of families to donate in order to guide clinical practice, education, training and increase donation rates to 80% in line with the NHS Blood and Transplant - Taking Organ Donation to 2020 strategy. Method: A literature review of published research. Results: Seven papers met the inclusion criteria ...
Background. The transplantation of human organs in the case of the irreversible failure of an organ has been raised for a long time in scientific and social committees, and this topic has been addressed from scientific, moral, religious, political, and legal perspectives [1-4].Organ donation options, such as the heart, lungs, kidneys, the liver, and the eyes, from a patient with brain death ...