David Reimer, 38; After Botched Surgery, He Was Raised as a Girl in Gender Experiment
- Copy Link URL Copied!
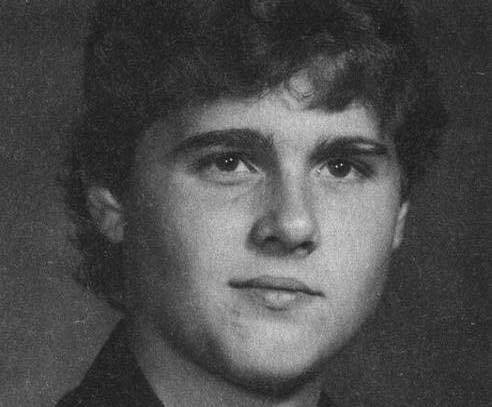
David Reimer, the Canadian man raised as a girl for most of the first 14 years of his life in a highly touted medical experiment that seemed to resolve the debate over the cultural and biological determinants of gender, has died at 38. He committed suicide May 4 in his hometown of Winnipeg, Canada.
At 8 months of age, Reimer became the unwitting subject of “sex reassignment,” a treatment method embraced by his parents after his penis was all but obliterated during a botched circumcision. The American doctor whose advice they sought recommended that their son be castrated, given hormone treatments and raised as a girl. The physician, Dr. John Money, supervised the case for several years and eventually wrote a paper declaring the success of the gender conversion.
For the record:
12:00 a.m. May 15, 2004 For The Record Los Angeles Times Saturday May 15, 2004 Home Edition Main News Part A Page 2 National Desk 0 inches; 25 words Type of Material: Correction Reimer obituary -- The obituary of David Reimer in Thursday’s California section said the doctor who botched Reimer’s circumcision was female. The doctor was male.
Known as the “John/Joan” case, it was widely publicized and gave credence to arguments presented in the 1970s by feminists and others that humans are sexually neutral at birth and that sex roles are largely the product of social conditioning.
But, in fact, the gender conversion was far from successful. Money’s experiment was a disaster for Reimer that created psychological scars he ultimately could not overcome.
Reimer’s story was told in the 2000 book “As Nature Made Him,” by journalist John Colapinto. Reimer said he cooperated with Colapinto in the hope that other children could be spared the miseries he experienced.
Reimer was born on Aug. 22, 1965, 12 minutes before his identical twin brother. His working-class parents named him Bruce and his brother Brian. Both babies were healthy and developed normally until they were seven months old, when they were discovered to have a condition called phimosis, a defect in the foreskin of the penis that makes urination difficult.
The Reimers were told that the problem was easily remedied with circumcision. During the procedure at the hospital, a doctor who did not usually perform such operations was assigned to the Reimer babies. She chose to use an electric cautery machine with a sharp cutting needle to sever the foreskin.
But something went terribly awry. Exactly where the error lay -- in the machine, or in the user -- was never determined. What quickly became clear was that baby Bruce had been irreparably maimed.
(The doctors decided not to try the operation on his brother Brian, whose phimosis later disappeared without treatment.)
The Reimers were distraught. Told that phallic reconstruction was a crude option that would never result in a fully functioning organ, they were without hope until one Sunday evening after the twins’ first birthday when they happened to tune in to an interview with Money on a television talk show. He was describing his successes at Johns Hopkins University in changing the sex of babies born with incomplete or ambiguous genitalia.
He said that through surgeries and hormone treatments he could turn a child into whichever sex seemed most appropriate, and that such reassignments were resulting in happy, healthy children.
Money, a Harvard-educated native of New Zealand, had already established a reputation as one of the world’s leading sex researchers, known for his brilliance and his arrogance. He was credited with coining the term “gender identity” to describe a person’s innate sense of maleness or femaleness.
The Reimers went to see Money, who with unwavering confidence told them that raising Bruce as a girl was the best course, and that they should never say a word to the child about ever having been a boy.
About six weeks before his second birthday, Bruce became Brenda on an operating table at Johns Hopkins. After bringing the toddler home, the Reimers began dressing her like a girl and giving her dolls.
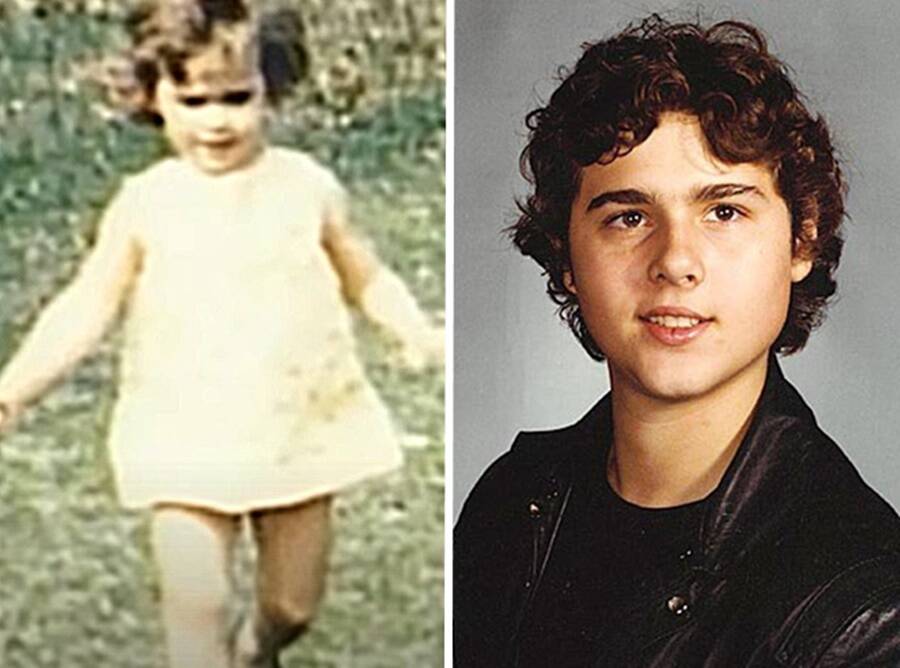
She was, on the surface, an appealing little girl, with round cheeks, curly locks and large, brown eyes. But Brenda rebelled at her imposed identity from the start. She tried to rip off the first dress that her mother sewed for her. When she saw her father shaving, she wanted a razor, too. She favored toy guns and trucks over sewing machines and Barbies. When she fought with her brother, it was clear that she was the stronger of the two. “I recognized Brenda as my sister,” Brian was quoted as saying in the Colapinto book. “But she never, ever acted the part.”
Money continued to perform annual checkups on Brenda, and despite the signs that Brenda was rejecting her feminized self, Money insisted that continuing on the path to womanhood was the proper course for her.
In 1972, when Brenda was 7, Money touted his success with her gender conversion in a speech to the American Assn. for the Advancement of Science in Washington, D.C., and in the book, “Man & Woman, Boy & Girl,” released the same day. The scientists in attendance recognized the significance of the case as readily as Money had years earlier. Because Brenda had an identical male twin, they offered the perfect test of the theory that gender is learned, not inborn.
Money already was the darling of radical feminists such as Kate Millett, who in her bestselling “Sexual Politics” two years earlier had cited Money’s writings from the 1950s as proof that “psychosexual personality is therefore postnatal and learned.”
Now his “success” was written up in Time magazine, which, in reporting on his speech, wrote that Money’s research provided “strong support for a major contention of women’s liberationists: that conventional patterns of masculine and feminine behavior can be altered.” In other words, nurture had trumped nature.
The Reimer case quickly was written into textbooks on pediatrics, psychiatry and sexuality as evidence that anatomy was not destiny, that sexual identity was far more malleable than anyone had thought possible. Money’s claims provided powerful support for those seeking medical or social remedies for gender-based ills.
What went unreported until decades later, however, was that Money’s experiment actually proved the opposite -- the immutability of one’s inborn sense of gender.
Money stopped commenting publicly on the case in 1980 and never acknowledged that the experiment was anything but a glowing success. Dr. Milton Diamond, a sexologist at the University of Hawaii at Manoa, had long been suspicious of Money’s claims. He was finally able to locate Reimer through a Canadian psychiatrist who had seen Reimer as a patient.
In an article published in the Archives of Pediatric and Adolescent Medicine in 1997, Diamond and the psychiatrist, Dr. H. Keith Sigmundson, showed how Brenda had steadily rejected her reassignment from male to female. In early adolescence, she refused to continue receiving the estrogen treatments that had helped her grow breasts. She stopped seeing Money. Finally, at 14, she refused to continue living as a girl.
When she confronted her father, he broke down in tears and told her what had happened shortly after her birth. Instead of being angry, Brenda was relieved. “For the first time everything made sense,” the article by Diamond and Sigmundson quoted her as saying, “and I understood who and what I was.”
She decided to reclaim the identity she was born with by taking male hormone shots and undergoing a double mastectomy and operations to build a penis with skin grafts. She changed her name to David, identifying with the Biblical David who fought Goliath. “It reminded me,” David told Colapinto, “of courage.”
David developed into a muscular, handsome young man. But the grueling surgeries spun him into periods of depression and twice caused him to attempt suicide. He spent months living alone in a cabin in the woods. At 22, he prayed to God for the first time in his life, begging for the chance to be a husband and father.
When he was 25, he married a woman and adopted her three children. Diamond reported that while the phallic reconstruction was only partially successful, David could have sexual intercourse and experience orgasm. He worked in a slaughterhouse and said he was happily adjusted to life as a man.
In interviews for Colapinto’s book, however, he acknowledged a deep well of wrenching anger that would never go away.
“You can never escape the past,” he told the Seattle Post-Intelligencer in 2000. “I had parts of my body cut away and thrown in a wastepaper basket. I’ve had my mind ripped away.”
His life began to unravel with the suicide of his brother two years ago. Brian Reimer had been treated for schizophrenia and took his life by overdosing on drugs. David visited his brother’s grave every day. He lost his job, separated from his wife and was deeply in debt after a failed investment.
He is survived by his wife, Jane; his parents, and his children.
Despite the hardships he experienced, he said he did not blame his parents for their decision to raise him as a girl. As he told Colapinto, “Mom and Dad wanted this to work so I’d be happy. That’s every parent’s dream for their child. But I couldn’t be happy for my parents. I had to be happy for me. You can’t be something that you’re not. You have to be you.”

Elaine Woo is a Los Angeles native who has written for her hometown paper since 1983. She covered public education and filled a variety of editing assignments before joining “the dead beat” – news obituaries – where she has produced artful pieces on celebrated local, national and international figures, including Norman Mailer, Julia Child and Rosa Parks. She left The Times in 2015.

More From the Los Angeles Times

The new COVID vaccine is here. Why these are the best times to get immunized

Opinion: How bringing back the woolly mammoth could save species that still walk the Earth
Aug. 28, 2024

‘I don’t want him to go’: An autistic teen and his family face stark choices
Aug. 27, 2024

Growing need. Glaring gaps. Why mental health care can be a struggle for autistic youth

David Reimer And The Tragic Story Of The ‘John/Joan Case’
David reimer was born a boy in winnipeg, canada in 1965 — but following a botched circumcision at the age of eight months, his parents raised him as a girl..
Facebook Although David Reimer’s story was initially seen as a success by his family and Dr. John Money, his story would eventually prove to have a tragic end.
David Reimer’s parents just wanted to do the right thing for him.
What was supposed to be a routine circumcision in 1965 turned into a life-altering nightmare for the Reimer family when the doctor performing his surgery accidentally singed the infant’s penis.
The damage was irreparable. Concerned that their son’s injury might cause him mental anguish as an adult, Reimer’s parents consulted with famed sexologist Dr. John Money after seeing him on television.
Money consequently suggested that Reimer undergo sex reassignment surgery and instead be raised female. Desperate, Reimer’s parents took his advice and changed their son’s name from “Bruce” to “Brenda.”
YouTube/Facebook David Reimer, born Bruce Reimer and biologically male, began an imposed gender transition as an infant.
Reimer appeared to take easily to his imposed gender identity as a female, and his case was initially seen as a success story by those physicians like Money who believed that gender was a matter of learned or taught behavior and not nature.
But in reality, Reimer struggled even as a child with his gender identity. Once he discovered the truth about his birth as a teenager, Reimer began a painful journey to return to his biological sex.
However, he could never fully recover. Finally, in 2004, David Reimer took his own life at the age of just 38.
David Reimer’s Future Is Decided By Sexologist John Money
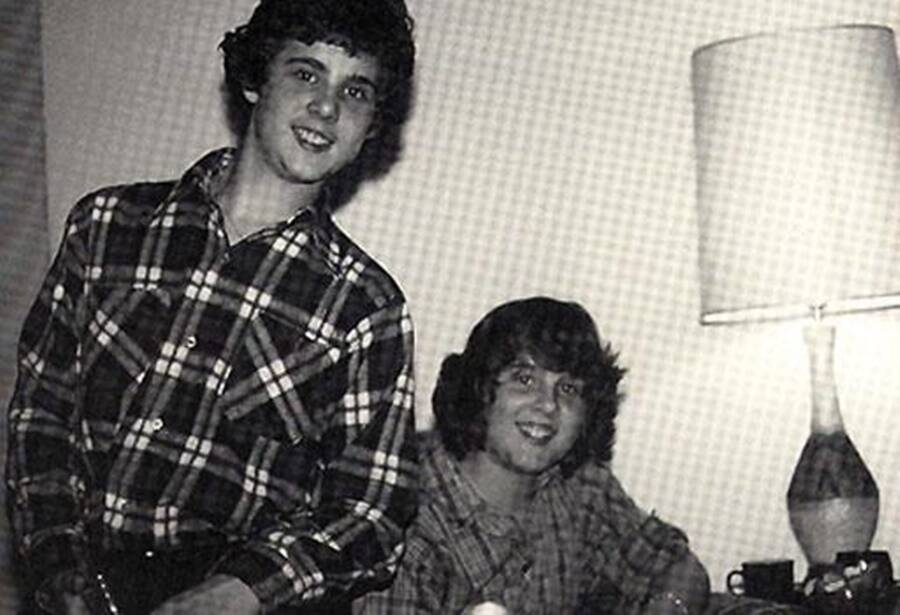
In Memory of David Reimer/Facebook At 14, David Reimer (right) chose to live as a male.
David Reimer was born Bruce Reimer in Winnipeg, Canada, in 1965. He had a twin brother named Brian, and the two were the first children of a rural teenage couple, Janet and Ron.
The baby boys were healthy but, at about eight months old, showed signs of difficulty with urinating. They were diagnosed with phimosis, a condition in which the foreskin cannot retract.
The Reimers took their children to be circumcised at the hospital, but after Bruce Reimer’s surgery went horribly awry because the surgeon used an electrocautery needle instead of a blade, Brian was not subjected to the same surgery and his phimosis healed naturally.
David Reimer’s parents desperately sought solutions for him until they saw psychologist John Money speak about his work on TV.
Money was considered one of the top sex researchers in the United States, and he specialized in the experiences of intersex children who, according to the UN Office of the High Commissioner for Human Rights, “do not fit the typical definitions for male or female bodies.”
Reimer’s mother wrote to Money explaining the horrible accident her son had endured. Within a few weeks, the young parents were on their way to see the doctor at Johns Hopkins Hospital in Baltimore, Maryland.
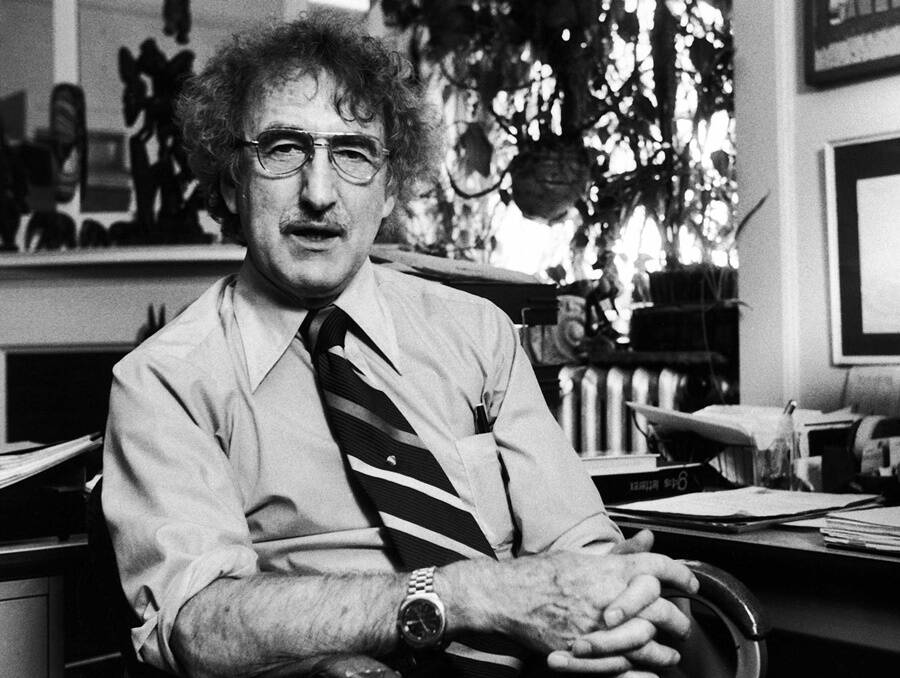
Diana Walker/The LIFE Images Collection via Getty Images Psychologist John Money claimed his gender experiment on the Reimer twins was a success — despite early warning signs that proved otherwise.
Money believed that a person’s gender identity was a social construct and the result of their upbringing. As such, he proposed that someone could be “taught” to identify differently than their biological sex.
Money thought that children were “gender-neutral” until about the age of two and theorized that parents had a period of time that he called the “gender gate” during which they could influence the sex of their child behaviorally.
The doctor thus made the radical proposition to reassign Bruce Reimer’s gender surgically, which would involve castrating his penis and giving him a prosthetic vagina instead. He would then be raised as a girl and not told of his former identity. Reimer’s parents agreed to the procedure and the infant’s imposed transition began shortly before his second birthday in 1967.
To Money, this situation also provided him with an opportunity to investigate his theory about gender identity. But his medical advice would prove fatally wrong in the case of David Reimer.
Related Posts
Reimer’s troubled childhood and the eventual reveal of the truth.

In Memory of David Reimer/Facebook Despite his tumultuous life, David Reimer found love with his wife Jane.
Upon John Money’s recommendation, Bruce Reimer began life as Brenda Reimer.
In addition to his sex reassignment surgery, Reimer was given estrogen supplements to help “feminize” his body. The Reimers returned to Money’s office every year so that the doctor could monitor both Brian and Brenda’s growth as a boy and a girl. The radical study became known as the John/Joan case.
Money noted that the twin sister, a.k.a. Brenda, was “much neater” than her twin brother Brian. Money also noted that Brenda was the more stubborn and dominant personality, which he dismissed as “tomboy traits.”
In 1975, when the twins turned nine, Money published his study in a book called Sexual Signatures where he described Reimer’s forced transition to Brenda as a success:
“The girl already preferred dresses to pants enjoyed wearing her hair ribbons, bracelets, and frilly blouses, and loved being her daddy’s little sweetheart. Throughout childhood, her stubbornness and the abundant physical energy she shares with her twin brother and expends freely have made her a tomboyish girl, but nonetheless a girl.”
But nothing could be further from the truth. Indeed, Reimer recalled his childhood as far more distressing.
“I never quite fit in,” David Reimer said in a 2000 interview on Oprah . “Building forts and getting into the odd fistfight, climbing trees — that’s the kind of stuff that I liked, but it was unacceptable as a girl.”
According to author John Colapinto who worked with Reimer on his book As Nature Made Him: The Boy Who Was Raised as A Girl , the frequent visits Reimer made to Money’s office were also traumatic.
Reimer was shown pictures of naked adults to “reinforce Brenda’s gender identity” and pressed by Money to endure more surgeries that would make him more feminine. Both of the twins would later accuse Money of making them pose in various sexual positions which, according to Money, was just another element of his theory that involved “sexual rehearsal play.”
Janet Reimer reportedly wasn’t blind to her child’s discomfort with his female gender identity, either. She recalled the first time that Reimer was put in a dress he angrily tore it off. “There were doubts along the way,” Janet confessed on Oprah . “But I couldn’t afford to contemplate them because I couldn’t afford to be wrong.”
Problems at home extended to school. Reimer was teased by classmates for his “masculine gait” and his standing to pee in the girl’s bathroom. When Reimer complained about feeling like a boy, his parents and other adults convinced him that it was just a phase.
Reimer’s secret disrupted the family. His father sunk into alcoholism and his mother attempted suicide. Reimer’s twin sibling, Brian, later descended into substance abuse and petty crime.
It wasn’t until the twins entered their teens that other doctors convinced the Reimers that it was time to tell their children the truth. After picking up Brenda from a psychologist appointment in 1980, Ron Reimer drove both his children to an ice cream parlor where he told them the whole story.
“Suddenly it all made sense why I felt the way I did,” Reimer said of the revelation. “I wasn’t some sort of weirdo. I wasn’t crazy.”
The Tragic End Of David Reimer’s Story
After discovering the truth, Reimer chose to live as a boy and assumed the name “David.”
He endured multiple surgeries to restore his gender to male, including a double mastectomy to remove the breasts that had grown from years of estrogen therapy and attaching an artificial penis in place of his artificial vagina. He also took testosterone supplements.
But the physical stress wore on his mental health. By his early 20s, Reimer had attempted suicide twice and remained deeply depressed for years after.
Despite his anguish, however, Reimer found love and married a woman named Jane. They were together for 14 years. He was a stepfather to her three children and developed hobbies like camping, fishing, antiques, and collecting old coins.

In Memory of David Reimer/Facebook David Reimer took his own life in May 2004. He was 38.
Reimer later agreed to work with a second sexologist named Milton Diamond on the expectation that speaking about his experience might prevent physicians from making similar decisions for other infants.
Diamond criticized Money’s study for its lack of evidence and worked with Reimer to debunk Money’s theory that gender identity could be totally taught or learned. In 1997, around the time Reimer began speaking publicly about his childhood ordeal, Diamond’s study was published in Archives of Pediatrics and Adolescent Medicine .
The breakthrough paper laid the foundation against performing sex reassignment surgery on intersex infants, which was once considered a “fix” for their gender non-conforming biology.
But the validation of the study wasn’t enough for Reimer to overcome his traumatic childhood. In May 2004, two years after his twin brother succumbed to a drug overdose, David Reimer killed himself. He was 38.
Reimer’s case was complex. His first gender transition was based on a medical accident and a scientific theory. As a result, he experienced gender dysphoria, which is the feeling that one’s biological sex differs from their gender identity. People who identify as transgender often experience gender dysphoria early in life as well.
Reimer may no longer be alive, but his journey to reclaim his gender identity contributed to a better understanding of the relationship between gender and biological sex.
After this look at the story of David Reimer, meet Maryam Khatoon Molkara , the transgender Iranian activist who helped legalize gender-confirming surgeries in Iran. Then, learn about Christine Jorgensen , America’s original transgender celebrity.

PO Box 24091 Brooklyn, NY 11202-4091
John Money Gender Experiment: Reimer Twins
Julia Simkus
Editor at Simply Psychology
BA (Hons) Psychology, Princeton University
Julia Simkus is a graduate of Princeton University with a Bachelor of Arts in Psychology. She is currently studying for a Master's Degree in Counseling for Mental Health and Wellness in September 2023. Julia's research has been published in peer reviewed journals.
Learn about our Editorial Process
Saul McLeod, PhD
Editor-in-Chief for Simply Psychology
BSc (Hons) Psychology, MRes, PhD, University of Manchester
Saul McLeod, PhD., is a qualified psychology teacher with over 18 years of experience in further and higher education. He has been published in peer-reviewed journals, including the Journal of Clinical Psychology.
Olivia Guy-Evans, MSc
Associate Editor for Simply Psychology
BSc (Hons) Psychology, MSc Psychology of Education
Olivia Guy-Evans is a writer and associate editor for Simply Psychology. She has previously worked in healthcare and educational sectors.
The John Money Experiment involved David Reimer, a twin boy raised as a girl following a botched circumcision. Money asserted gender was primarily learned, not innate.
However, David struggled with his female identity and transitioned back to male in adolescence. The case challenged Money’s theory, highlighting the influence of biological sex on gender identity.
- David Reimer was born in 1965; he had a MZ twin brother. When he was 8 months old his penis was accidentally cut off during surgery.
- His parents contacted John Money, a psychologist who was developing a theory of gender neutrality. His theory claimed that a child would take the gender identity he/she was raised with rather than the gender identity corresponding to the biological sex.
- David’s parents brought him up as a girl and Money wrote extensively about this case claiming it supported his theory. However, Brenda as he was named was suffering from severe psychological and emotional difficulties and in her teens, when she found out what had happened, she reverted back to being a boy.
- This case study supports the influence of testosterone on gender development as it shows that David’s brain development was influenced by the presence of this hormone and its effects on gender identity was stronger that the influence of social factors.
What Did John Money Do To The Twins
David Reimer was an identical twin boy born in Canada in 1965. When he was 8 months old, his penis was irreparably damaged during a botched circumcision.
John Money, a psychologist from Johns Hopkins University, had a prominent reputation in the field of sexual development and gender identity.
David’s parents took David to see Dr. Money at Johns Hopkins Hospital in Baltimore, where he advised that David be “sex reassigned” as a girl through surgical, hormonal, and psychological treatments.
John Money believed that gender identity is primarily learned through one’s upbringing (nurture) as opposed to one’s inborn traits (nature).
He proposed that gender identity could be changed through behavioral interventions, and he advocated that gender reassignment was the solution for treating any child with intersex traits or atypical sex anatomies.
Dr. John Money argued that it’s possible to habilitate a baby with a defective penis more effectively as a girl than a boy.
At the age of 22 months, David underwent extensive surgery in which his testes and penis were surgically removed and rudimentary female genitals were constructed.
David’s parents raised him as a female and gave him the name Brenda (this name was chosen to be similar to his birth name, Bruce). David was given estrogen during adolescence to promote the development of breasts.
He was forced to wear dresses and was directed to engage in typical female norms, such as playing with dolls and mingling with other girls.
Throughout his childhood, David was never informed that he was biologically male and that he was an experimental subject in a controversial investigation to bolster Money’s belief in the theory of gender neutrality – that nurture, not nature, determines gender identity and sexual orientation.
David’s twin brother, Brian, served as the ideal control because the brothers had the same genetic makeup, but one was raised as a girl and the other as a boy. Money continued to see David and Brian for consultations and checkups annually.
During these check-ups, Money would force the twins to rehearse sexual acts and inspect one another’s genitals. On some occasions, Money would even photograph the twins doing these exercises. Money claimed that childhood sexual rehearsal play was important for healthy childhood sexual exploration.
David also recalls receiving anger and verbal abuse from Money if they resisted participation.
Money (1972) reported on Reimer’s progress as the “John/Joan case” to keep the identity of David anonymous. Money described David’s transition as successful.
He claimed that David behaved like a little girl and did not demonstrate any of the boyish mannerisms of his twin brother Brian. Money would publish this data to reinforce his theories on gender fluidity and to justify that gender identity is primarily learned.
In reality, though, David was never happy as a girl. He rejected his female identity and experienced severe gender dysphoria . He would complain to his parents and teachers that he felt like a boy and would refuse to wear dresses or play with dolls.
He was severely bullied in school and experienced suicidal depression throughout adolescence. Upon learning about the truth about his birth and sex of rearing from his father at the age of 15, David assumed a male gender identity, calling himself David.
David Reimer underwent treatments to reverse the assignment such as testosterone injections and surgeries to remove his breasts and reconstruct a penis.
David married a woman named Jane at 22 years and adopted three children.
Dr. Milton Diamond, a psychologist and sexologist at the University of Hawaii and a longtime academic rival of John Money, met with David to discuss his story in the mid-1990s.
Diamond (1997) brought David’s experiences to international attention by reporting the true outcome of David’s case to prevent physicians from making similar decisions when treating other infants. Diamond helped debunk Money’s theory that gender identity could be completely learned through intervention.
David continued to suffer from psychological trauma throughout adulthood due to Money’s experiments and his harrowing childhood experiences. David endured unemployment, the death of his twin brother Brian, and marital difficulties.
At the age of thirty-eight, David committed suicide.
David’s case became the subject of multiple books, magazine articles, and documentaries. He brought to attention to the complications of gender identity and called into question the ethicality of sex reassignment of infants and children.
Originally, Money’s view of gender malleability dominated the field as his initial report on David was that the reassignment had been a success. However, this view was disproved once the truth about David came to light.
His case led to a decline in the number of sex reassignment surgeries for unambiguous XY male infants with a micropenis and other congenital malformations and brought into question the malleability of gender and sex.
At present, however, the clinical literature is still deeply divided on the best way to manage cases of intersex infants.
Colapinto, J. (2000). As nature made him: The boy who was raised as a girl. New York, NY: Harper Collins.
Colapinto, J. (2018). As nature made him: The boy who was raised as a girl. Langara College.
Diamond, M., & Sigmundson, H. K. (1997). Sex reassignment at birth: Long-term review and clinical implications . Archives of pediatrics & adolescent medicine, 151(3), 298-304.
Money, J., & Ehrhardt, A. A. (1972). Man & Woman, Boy & Girl : The Differentiation and Dimorphism of Gender Identity from Conception to Maturity. Baltimore, Maryland: Johns Hopkins University Press.
Money, J., & Tucker, P. (1975). Sexual signatures: On being a man or a woman.
Money, J. (1994). The concept of gender identity disorder in childhood and adolescence after 39 years . Journal of sex & marital therapy, 20(3), 163-177.
David Reimer and John Money Gender Reassignment Controversy: The John/Joan Case
In the mid-1960s, psychologist John Money encouraged the gender reassignment of David Reimer, who was born a biological male but suffered irreparable damage to his penis as an infant. Born in 1965 as Bruce Reimer, his penis was irreparably damaged during infancy due to a failed circumcision. After encouragement from Money, Reimer’s parents decided to raise Reimer as a girl. Reimer underwent surgery as an infant to construct rudimentary female genitals, and was given female hormones during puberty. During childhood, Reimer was never told he was biologically male and regularly visited Money, who tracked the progress of his gender reassignment. Reimer unknowingly acted as an experimental subject in Money’s controversial investigation, which he called the John/Joan case. The case provided results that were used to justify thousands of sex reassignment surgeries for cases of children with reproductive abnormalities. Despite his upbringing, Reimer rejected the female identity as a young teenager and began living as a male. He suffered severe depression throughout his life, which culminated in his suicide at thirty-eight years old. Reimer, and his public statements about the trauma of his transition, brought attention to gender identity and called into question the sex reassignment of infants and children.
Bruce Peter Reimer was born on 22 August 1965 in Winnipeg, Ontario, to Janet and Ron Reimer. At six months of age, both Reimer and his identical twin, Brian, were diagnosed with phimosis, a condition in which the foreskin of the penis cannot retract, inhibiting regular urination. On 27 April 1966, Reimer underwent circumcision, a common procedure in which a physician surgically removes the foreskin of the penis. Usually, physicians performing circumcisions use a scalpel or other sharp instrument to remove foreskin. However, Reimer’s physician used the unconventional technique of cauterization, or burning to cause tissue death. Reimer’s circumcision failed. Reimer’s brother did not undergo circumcision and his phimosis healed naturally. While the true extent of Reimer’s penile damage was unclear, the overwhelming majority of biographers and journalists maintained that it was either totally severed or otherwise damaged beyond the possibility of function.
In 1967, Reimer’s parents sought the help of John Money, a psychologist and sexologist who worked at the Johns Hopkins Hospital in Baltimore, Maryland. In the mid-twentieth century, Money helped establish views on the psychology of gender identities and roles. In his academic work, Money argued in favor of the increasingly mainstream idea that gender was a societal construct, malleable from an early age. He stated that being raised as a female was in Reimer’s interest, and recommended sexual reassignment surgery. At the time, infants born with abnormal or intersex genitalia commonly received such interventions.
Following their consultation with Money, Reimer’s parents decided to raise Reimer as a girl. Physicians at the Johns Hopkins Hospital removed Reimer’s testes and damaged penis, and constructed vestigial vulvae and a vaginal canal in their place. The physicians also opened a small hole in Reimer’s lower abdomen for urination. Following his gender reassignment surgery, Reimer was given the first name Brenda, and his parents raised him as a girl. He received estrogen during adolescence to promote the development of breasts. Throughout his childhood, Reimer was not informed about his male biology.
Throughout his childhood, Reimer received annual checkups from Money. His twin brother was also part of Money’s research on sexual development and gender in children. As identical twins growing up in the same family, the Reimer brothers were what Money considered ideal case subjects for a psychology study on gender. Reimer was the first documented case of sex reassignment of a child born developmentally normal, while Reimer’s brother was a control subject who shared Reimer’s genetic makeup, intrauterine space, and household.
During the twin’s psychiatric visits with Money, and as part of his research, Reimer and his twin brother were directed to inspect one another’s genitals and engage in behavior resembling sexual intercourse. Reimer claimed that much of Money’s treatment involved the forced reenactment of sexual positions and motions with his brother. In some exercises, the brothers rehearsed missionary positions with thrusting motions, which Money justified as the rehearsal of healthy childhood sexual exploration. In a Rolling Stone interview, Reimer recalled that at least once, Money photographed those exercises. Money also made the brothers inspect one another’s pubic areas. Reimer stated that Money observed those exercises both alone and with as many as six colleagues. Reimer recounted anger and verbal abuse from Money if he or his brother resisted orders, in contrast to the calm and scientific demeanor Money presented to their parents. Reimer and his brother underwent Money’s treatments at preschool and grade school age. Money described Reimer’s transition as successful, and claimed that Reimer’s girlish behavior stood in stark contrast to his brother’s boyishness. Money reported on Reimer’s case as the John/Joan case, leaving out Reimer’s real name. For over a decade, Reimer and his brother unknowingly provided data that, according to biographers and the Intersex Society of North America, was used to reinforce Money’s theories on gender fluidity and provided justification for thousands of sex reassignment surgeries for children with abnormal genitals.
Contrary to Money’s notes, Reimer reports that as a child he experienced severe gender dysphoria, a condition in which someone experiences distress as a result of their assigned gender. Reimer reported that he did not identify as a girl and resented Money’s visits for treatment. At the age of thirteen, Reimer threatened to commit suicide if his parents took him to Money on the next annual visit. Bullied by peers in school for his masculine traits, Reimer claimed that despite receiving female hormones, wearing dresses, and having his interests directed toward typically female norms, he always felt that he was a boy. In 1980, at the age of fifteen, Reimer’s father told him the truth about his birth and the subsequent procedures. Following that revelation, Reimer assumed a male identity, taking the first name David. By age twenty-one, Reimer had received testosterone therapy and surgeries to remove his breasts and reconstruct a penis. He married Jane Fontaine, a single mother of three, on 22 September 1990.
In adulthood, Reimer reported that he suffered psychological trauma due to Money’s experiments, which Money had used to justify sexual reassignment surgery for children with intersex or damaged genitals since the 1970s. In the mid-1990s, Reimer met Milton Diamond, a psychologist at the University of Hawaii, in Honolulu, Hawaii, and an academic rival of Money. Reimer participated in a follow-up study conducted by Diamond, in which Diamond cataloged the failures of Reimer’s transition.
In 1997, Reimer began speaking publicly about his experiences, beginning with his participation in Diamond’s study. Reimer’s first interview appeared in the December 1997 issue of Rolling Stone magazine. In interviews, and a later book about his experience, Reimer described his interactions with Money as torturous and abusive. Accordingly, Reimer claimed he developed a lifelong distrust of hospitals and medical professionals.
With those reports, Reimer caused a multifaceted controversy over Money’s methods, honesty in data reporting, and the general ethics of sex reassignment surgeries on infants and children. Reimer’s description of his childhood conflicted with the scientific consensus about sex reassignment at the time. According to NOVA , Money led scientists to believe that the John/Joan case demonstrated an unreservedly successful sex transition. Reimer’s parents later blamed Money’s methods and alleged surreptitiousness for the psychological illnesses of their sons, although the notes of a former graduate student in Money’s lab indicated that Reimer’s parents dishonestly represented the transition’s success to Money and his coworkers. Reimer was further alleged by supporters of Money to have incorrectly recalled the details of his treatment. On Reimer’s case, Money publicly dismissed his criticism as anti-feminist and anti-trans bias, but, according to his colleagues, was personally ashamed of the failure.
In his early twenties, Reimer attempted to commit suicide twice. According to Reimer, his adult family life was strained by marital problems and employment difficulty. Reimer’s brother, who suffered from depression and schizophrenia, died from an antidepressant drug overdose in July of 2002. On 2 May 2004, Reimer’s wife told him that she wanted a divorce. Two days later, at the age of thirty-eight, Reimer committed suicide by firearm.
Reimer, Money, and the case became subjects of numerous books and documentaries following the exposé. Reimer also became somewhat iconic in popular culture, being directly referenced or alluded to in the television shows Chicago Hope , Law & Order , and Mental . The BBC series Horizon covered his story in two episodes, “The Boy Who Was Turned into a Girl” (2000) and “Dr. Money and the Boy with No Penis” (2004). Canadian rock group The Weakerthans wrote “Hymn of the Medical Oddity” about Reimer, and the New York-based Ensemble Studio Theatre production Boy was based on Reimer’s life.
- Carey, Benedict. “John William Money, 84, Sexual Identity Researcher, Dies.” New York Times , 11 July 2006.
- Colapinto, John. "The True Story of John/Joan." Rolling Stone 11 (1997): 54–73.
- Colapinto, John. As Nature Made Him: The Boy who was Raised as a Girl . New York: HarperCollins Publishers, 2000.
- Colapinto, John. "Gender Gap—What were the real reasons behind David Reimer’s suicide?" Slate (2004).
- Dr. Money and the Boy with No Penis , documentary, written by Sanjida O’Connell (BBC, 2004), Film.
- The Boy Who Was Turned Into a Girl , documentary, directed by Andrew Cohen (BBC, 2000.), Film.
- “Who was David Reimer (also, sadly, known as John/Joan)?” Intersex Society of North America . http://www.isna.org/faq/reimer (Accessed October 31, 2017).
How to cite
Articles rights and graphics.
Copyright Arizona Board of Regents Licensed as Creative Commons Attribution-NonCommercial-Share Alike 3.0 Unported (CC BY-NC-SA 3.0)
Last modified
Share this page.
'You can't undo surgery': More parents of intersex babies are rejecting operations

Kristina Turner will never forget the moment doctors at a hospital in Washington state told her something was different about her baby. Shortly after Ori was born in 2007, the medical staff noticed that the infant had abnormal genital swelling. Other than that, doctors assured Turner, everything was fine.
“They identified Ori as being female and told us we had a happy, healthy baby, and we went on our way,” Turner told NBC News.
But as a mother, Turner recalled, “I kind of knew something was different.”
A specialist later told Turner, a massage therapist, and her husband, Josh, a construction worker, that their infant had a rare intersex condition called partial androgen insensitivity syndrome with mosaicism. The condition caused Ori to have both XX chromosomes and XY chromosomes and genitalia that doctors did not consider clearly “male” or “female.”
Ori was perfectly healthy, but Turner said surgeons pressured her to agree to cosmetic surgery to make Ori appear more clearly female. She immediately refused.
“Intersex” is an umbrella term for people whose bodies do not match the strict definitions of male or female. Dozens of intersex variations exist, affecting the reproductive organs in ways that may or may not be visible. While the Trump administration seeks to permanently identify people as “male” or “female” based on their physical appearance at birth — a leaked draft proposal was sharply criticized by LGBTQ advocates this week — at least one in 2,000 people are born with atypical genitalia because of one of these conditions, according to Human Rights Watch, an international research and advocacy group.
“Gender normalizing” surgeries have been performed on intersex babies and children since at least the 1950s, often in secrecy, without ever telling the children. In the following decades, some people who underwent these surgeries as children began to speak out against them as human rights violations. Some said they had been assigned the wrong gender, while others had endured severe complications, including sexual dysfunction and infertility.
As their stories piled up, advocacy groups began calling for better education and support for parents of intersex children, as well as for limits on these types of operations. The advocates do not oppose surgery for intersex people in general, but they believe that if the goal is more cosmetic than medical, it’s a choice children should be allowed to make for themselves when they’re older.
This view is gaining traction. Three U.S. surgeons general, the United Nations, the World Health Organization, Physicians for Human Rights, the American Academy of Family Physicians , Human Rights Watch and Amnesty International have condemned medically unnecessary surgery on these children. In August, California became the first state to pass a resolution condemning the operations, though they are still legal there.

NBC OUT 'A baby cannot provide ... consent': Calif. lawmakers denounce infant intersex surgeries
But within the medical community — and within support groups for these children — opinion is not unanimous. The Societies for Pediatric Urology, which represents the physicians who treat these patients, strongly disagreed with the California legislation. The organization believes parents should have the option of choosing surgery for their baby if they believe it’s best for the child’s long-term physical and mental health.
In the absence of clear guidance, hundreds of parents in the U.S. each year face a decision that will have a lifelong impact on their child. There are no official figures, but experts believe that while more parents are deciding against surgery, they are still in the minority.
Dr. Yee-Ming Chan, a pediatric endocrinologist at Harvard Medical School, said there is little research to help parents decide.
“There’s certainly stories of individuals who found it distressing to have ambiguous genitalia, but we don’t know how representative that is,” Chan said. “So I think there really is a ton of unanswered questions.”
ORI’S STORY
Turner, who lives an hour and a half north of Seattle, faced criticism from some extended family members who believed she was placing an enormous burden on her newborn in choosing not to have the surgery.
“But I just completely disagreed,” Turner, 35, said, “because I was like, ‘You can’t undo surgery.’”

Since she couldn’t predict the gender her child would embrace, she said, it didn’t seem like her decision to make. And she recalled that none of the doctors could tell her how the surgery, which involved altering sensitive tissue, might affect the baby as an adult.
Based on the advice of medical professionals, Turner and her husband decided to raise Ori as a girl, because they were told that was how the child would likely identify. But the parents always planned to give Ori leeway to explore. If there was a chance that Ori felt male, Turner wanted it to be clear that that was OK. She concocted a bedtime story in which doctors aren’t sure what a baby’s sex is, so the parents let the baby decide over time.
Around the age of 7, Ori came to Turner one night and said, “I feel like I was supposed to be a boy.”
“I was like, ‘Oh my God, thank God I didn’t make a huge mistake,’” Turner said of her decision not to do the surgery.
For several years, Ori wore boy’s clothing and wanted to be called Alex. Then, around fifth grade, Ori started to dress and behave in ways stereotypical of boys and girls — “a cute hair clip with a really masculine outfit,” Turner recalled.
In 2017, the Turners took Ori to a gathering of people who are intersex in Phoenix. There, Ori met some attendees who identified as transgender or nonbinary (neither male nor female). Ori decided to stop using the name Alex and asked to be called by gender-neutral they/them pronouns.
Ori, now 11, loves playing video games like Minecraft and is enamored with the movie franchise “How to Train Your Dragon.” Ori has not been bullied and said that being intersex is “really fun and awesome.”

The middle schooler wants to be a lawyer and an actor someday — as well as an activist “so I can help intersex kids and adults.” In March, Ori gave a TEDx Talk about growing up intersex. Turner helped with the presentation, but the gregarious preteen did most of the talking.
“I wish that [people] knew that intersex people are just like them,” Ori said. “They’re human.”
THE SURGERY QUESTION
In rare cases, intersex babies need emergency surgery when they are born — for example, if they are unable to urinate properly.
But in the vast majority of cases, the operations are done to prevent a child from suffering presumed psychological distress later in life, experts said. Surgeons prefer to do these operations when children are between 6 and 18 months old — when healing is believed to be optimal and when children are too young to remember, experts said.
"It’s a violation of their human rights to choose what they want their bodies to be like."
In these cases, based on assumptions about a child’s future desires, “medically necessary” is hard to define, Chan said.
“Ultimately, my concern is that we find that things like doing some of the surgeries in infancy might be really helpful and beneficial for some individuals, and really harmful for others, and how do you balance that out?” he asked.
Parents often say that their decision to agree to surgery was at least partly driven by fear, according to a 2017 Human Rights Watch report on surgery on intersex children. There’s a growing acceptance among young Americans for those who identify outside the male-female binary — 56 percent of Generation Z kids know someone who uses gender-neutral pronouns, one survey found — and New York City recently joined four states in allowing gender-neutral birth certificates . But amid the Trump administration’s reported push to more stringently define gender identity, parents still worry about bullying, as well as the judgment their child could face in day care centers and locker rooms.

Opponents of surgery say that it is more likely to cause distress than to prevent it. For instance, if a child who undergoes feminizing surgery later identifies as male, “that’s really a catastrophe,” said Dr. Arlene Baratz, a physician and an advocate at interACT, a group that supports intersex youth.
“To do that before children have a say is, I believe it’s a violation of their human rights to choose what they want their bodies to be like,” Baratz said.
THE CASE FOR SURGERY
Because of the variety of intersex conditions and the range of medical advice, some experts fear California’s legislation and other efforts to restrict surgery could have a negative effect on some intersex children.
Dr. Earl Cheng, a surgeon and urologist with H. Lurie Children’s Hospital of Chicago, called the efforts “a catch-all umbrella in which one size fits all.”
“One size does not fit all,” Cheng said. “You need to have a discussion based upon exactly what that individual has.”
Some adults who underwent the surgery as children say they’re happy with the results.
Lesley Holroyd, 61, a nurse who lives in Florida, was born with congenital adrenal hyperplasia (CAH), which means she is genetically female but was overexposed to male hormones in utero.
“I’ve had no issues,” Holroyd said of having surgery as a child, adding that the thought of not having done so was “horrifying.” She said she has always seen herself as female and does not identify as intersex.
“Parents know their children certainly better than the government does."
A 2018 study found that 79 percent of adult CAH women who received surgery as children were satisfied with surgical outcomes.
The CARES Foundation, an organization that supports families with children with CAH, lobbied to make them exempt from the California resolution, saying surgery should be up to their parents.
“Parents know their children certainly better than the government does,” said Dina Matos, the group’s executive director.
‘JUST LIKE RAISING ANY OTHER KID’
While adults debate what’s best for kids like Ori Turner, the sixth-grader has already figured it out. Asked about surgery, Ori replied that it was unnecessary because “I’m perfect.”
Ori, who goes to school part time and is home-schooled the rest, is writing a children’s book about growing up as an intersex kid, tentatively titled “The Story of Ori.” The preteen wants Washington State to outlaw cosmetic surgeries on intersex infants and plans to start a petition with interACT.
Turner said parenting an intersex child has been challenging at times, especially when some relatives have criticized her choices, but she said she has learned to “stand strong” in her beliefs.
“Raising Ori is just like raising any other kid,” Turner said. “It’s raising the rest of the world that’s the problem.”
FOLLOW NBC OUT ON TWITTER , FACEBOOK AND INSTAGRAM
- The Moving Image
A Perfect Daughter: Gender Reassignment by Gillian Laub
N ikki was born Niko. A biological boy at birth, she began at the age of 10 the complicated transition to becoming girl. With the utmost support of her family and friends, two years later, she is living happily as the person she always knew herself to be — singing, acting and dancing, often draped in pink.
Earlier this summer, PEOPLE magazine commissioned photographer Gillian Laub to spend several days with Nikki’s family in California, documenting her life after the transition through video and photographic stills. Her portrait shows what it was like for Nikki coming out with her gender identity, finding solace in puberty-blocking medication and looking to the gender reassignment surgery on the horizon for her teenage years.
“It’s always an honor when someone is open and wants to share their life in such an intimate way under the gaze of a camera,” Laub tells TIME, “so the minute the editor told me about Nikki, I said of course I would love to do it.”
To gain their trust and to make them feel comfortable, Laub spent the first day just talking with the family without her cameras.
“Nikki told me she spent the first ten years of her life feeling like she was in the wrong body, almost betrayed by it,” she says. “After the transition, she finally felt happy, safe and proud in her body. I wanted to convey the new feeling of freedom and liberation.”
What stood out to Laub most and what she aimed to capture in the video above was how immensely loving Nikki’s family was. With the knowledge that 50% of transgender youth will attempt to commit suicide by the age of 20, they strove to provide all the support they could for their child to lead the life she wanted.
“Although this story ultimately is a very happy ending,” Laub says, “the family went through years of heartache and stress. They lived with a secret that they all struggled with for very long. The reason they were sharing their story publicly is because they wished they had known sooner that this was actually something many families deal with; they wouldn’t have had so many years of worry and confusion.”
Gillian Laub is a photographer based in New York and a frequent contributor to TIME. See more of her work here .
Eugene Reznik is a Brooklyn-based photographer and writer. Follow him on Twitter @eugene_reznik .
More Must-Reads from TIME
- Breaking Down the 2024 Election Calendar
- How Nayib Bukele’s ‘Iron Fist’ Has Transformed El Salvador
- What if Ultra-Processed Foods Aren’t as Bad as You Think?
- How Ukraine Beat Russia in the Battle of the Black Sea
- Long COVID Looks Different in Kids
- How Project 2025 Would Jeopardize Americans’ Health
- What a $129 Frying Pan Says About America’s Eating Habits
- The 32 Most Anticipated Books of Fall 2024
Contact us at [email protected]
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
- My Bibliography
- Collections
- Citation manager
Save citation to file
Email citation, add to collections.
- Create a new collection
- Add to an existing collection
Add to My Bibliography
Your saved search, create a file for external citation management software, your rss feed.
- Search in PubMed
- Search in NLM Catalog
- Add to Search
Sex reassignment at birth. Long-term review and clinical implications
Affiliation.
- 1 Department of Anatomy and Reproductive Biology, Pacific Center for Sex and Society, University of Hawaii-Manoa, USA.
- PMID: 9080940
- DOI: 10.1001/archpedi.1997.02170400084015
This article is a long-term follow-up to a classic case reported in pediatric, psychiatric, and sexological literature. The penis of an XY individual was accidentally ablated and he was subsequently raised as a female. Initially this individual was described as developing into a normally functioning female. The individual, however, was later found to reject this sex of rearing, switched at puberty to living as a male, and has successfully lived as such from that time to the present. The standard in instances of extensive penile damage to infants is to recommend rearing the male as a female. Subsequent cases should, however, be managed in light of this new evidence.
PubMed Disclaimer
- To be male or female--that is the question. Reiner W. Reiner W. Arch Pediatr Adolesc Med. 1997 Mar;151(3):224-5. doi: 10.1001/archpedi.1997.02170400010002. Arch Pediatr Adolesc Med. 1997. PMID: 9080927 No abstract available.
- Sex reassignment at birth: long-term review and clinical implications. Van Howe RS, Cold CJ. Van Howe RS, et al. Arch Pediatr Adolesc Med. 1997 Oct;151(10):1062. doi: 10.1001/archpedi.1997.02170470096021. Arch Pediatr Adolesc Med. 1997. PMID: 9343024 No abstract available.
- Sex reassignment at birth. Benjamin JT. Benjamin JT. Arch Pediatr Adolesc Med. 1997 Oct;151(10):1062-4. doi: 10.1001/archpedi.1997.02170470096023. Arch Pediatr Adolesc Med. 1997. PMID: 9343025 No abstract available.
- Sex reassignment at birth. Schwarz HP. Schwarz HP. Arch Pediatr Adolesc Med. 1997 Oct;151(10):1064. doi: 10.1001/archpedi.1997.02170470098026. Arch Pediatr Adolesc Med. 1997. PMID: 9343026 No abstract available.
Similar articles
- Experiment of nurture: ablatio penis at 2 months, sex reassignment at 7 months, and a psychosexual follow-up in young adulthood. Bradley SJ, Oliver GD, Chernick AB, Zucker KJ. Bradley SJ, et al. Pediatrics. 1998 Jul;102(1):e9. doi: 10.1542/peds.102.1.e9. Pediatrics. 1998. PMID: 9651461
- Ambiguous genitalia, gender-identity problems, and sex reassignment. Dittmann RW. Dittmann RW. J Sex Marital Ther. 1998 Oct-Dec;24(4):255-71. doi: 10.1080/00926239808403961. J Sex Marital Ther. 1998. PMID: 9805286
- [Gender selection and postoperative follow-up analysis in 85 children with 46, XY disorders of sex development]. Zhao M, Gong CX, Liang AM, Song YN, Liu Y, Wang JL, Ma Y, Ji WJ. Zhao M, et al. Zhonghua Er Ke Za Zhi. 2019 Jun 2;57(6):434-439. doi: 10.3760/cma.j.issn.0578-1310.2019.06.007. Zhonghua Er Ke Za Zhi. 2019. PMID: 31216800 Chinese.
- Gender identity outcome in female-raised 46,XY persons with penile agenesis, cloacal exstrophy of the bladder, or penile ablation. Meyer-Bahlburg HF. Meyer-Bahlburg HF. Arch Sex Behav. 2005 Aug;34(4):423-38. doi: 10.1007/s10508-005-4342-9. Arch Sex Behav. 2005. PMID: 16010465 Review.
- Gender identity/role differentiation in adolescents affected by syndromes of abnormal sex differentiation. Wisniewski AB, Migeon CJ. Wisniewski AB, et al. Adolesc Med. 2002 Feb;13(1):119-28, vii. Adolesc Med. 2002. PMID: 11841959 Review.
- Recommendations for 46,XY Disorders/Differences of Sex Development Across Two Decades: Insights from North American Pediatric Endocrinologists and Urologists. Khorashad BS, Gardner M, Lee PA, Kogan BA, Sandberg DE. Khorashad BS, et al. Arch Sex Behav. 2024 Aug;53(8):2939-2956. doi: 10.1007/s10508-024-02942-1. Epub 2024 Jul 22. Arch Sex Behav. 2024. PMID: 39039338 Free PMC article.
- Gender Identity Orientation and Sexual Activity-A Survey among Transgender and Gender-Diverse (TGD) Individuals in Norway. Almås EM, Benestad EEP, Bolstad SH, Karlsen TI, Giami A. Almås EM, et al. Healthcare (Basel). 2024 Feb 16;12(4):482. doi: 10.3390/healthcare12040482. Healthcare (Basel). 2024. PMID: 38391857 Free PMC article.
- "I Think It's Too Early to Know": Gender Identity Labels and Gender Expression of Young Children With Nonbinary or Binary Transgender Parents. Riskind RG, Tornello SL. Riskind RG, et al. Front Psychol. 2022 Aug 17;13:916088. doi: 10.3389/fpsyg.2022.916088. eCollection 2022. Front Psychol. 2022. PMID: 36059766 Free PMC article.
- Low Perinatal Androgens Predict Recalled Childhood Gender Nonconformity in Men. Shirazi TN, Self H, Rosenfield KA, Dawood K, Welling LLM, Cárdenas R, Bailey JM, Balasubramanian R, Delaney A, Breedlove SM, Puts DA. Shirazi TN, et al. Psychol Sci. 2022 Mar;33(3):343-353. doi: 10.1177/09567976211036075. Epub 2022 Feb 22. Psychol Sci. 2022. PMID: 35191784 Free PMC article.
- The "Normalization" of Intersex Bodies and "Othering" of Intersex Identities in Australia. Carpenter M. Carpenter M. J Bioeth Inq. 2018 Dec;15(4):487-495. doi: 10.1007/s11673-018-9855-8. Epub 2018 May 7. J Bioeth Inq. 2018. PMID: 29736897
Publication types
- Search in MeSH
Related information
- Cited in Books
LinkOut - more resources
Full text sources.
- Ovid Technologies, Inc.
- Silverchair Information Systems
- Citation Manager
NCBI Literature Resources
MeSH PMC Bookshelf Disclaimer
The PubMed wordmark and PubMed logo are registered trademarks of the U.S. Department of Health and Human Services (HHS). Unauthorized use of these marks is strictly prohibited.
- GENDER REVOLUTION
In the Operating Room During Gender Reassignment Surgery
Behind the scenes with identical twin Emmie Smith during her medical transition.
Before August 30, 2016, getting stitches at age seven was the most time Emmie Smith had ever spent in a hospital.
That morning, she swapped her plaid shirt and jean shorts for a gown, tucked her hair into a cap, and prepared for surgery to conform her anatomy to the gender she already identified with: woman. In the operating room with her was National Geographic photographer Lynn Johnson. She and Emmie hoped they could demystify the procedure by documenting it, close-up and unflinching. “It was stressful and scary at times, but it almost created a mission other than just recovery,” Emmie says. “We were making something together.”
It had been a year and a half since Emmie had first come out as a transgender woman on Facebook. Telling her family and friends had been an enormous relief. “I’m not sure I could have taken another few years of being closeted,” she says.
Still, it was a challenging time for her family. Her mother, Reverend Kate Malin, is a prominent figure in their Massachusetts town, and her identical twin sons Caleb and Walker were familiar fixtures at her Episcopal church. A month after Walker came out as Emmie, Malin stepped out from behind her pulpit and walked into the aisle. Halfway through her sermon she decided it was time to address the change in her family.
“As most of you know, Bruce and I have three children,” she began. “Caleb and Walker, who are 17, and 13-year-old Owen. Walker’s new name is Emerson, and she prefers Emmie or Em. She’s wearing feminine clothing and makeup and will likely continue to move in the direction of a more feminized body.”
Follow Emmie's transition in pictures

Kate nervously revealed her struggle to the attentive New England crowd. “I feel broken much of the time,” she confessed. “I’ve wanted to run away, and I’ve prayed for this child that I would gladly die for, guilty for how much I miss the person I thought was Walker and everything I thought might be.”
After the sermon, the congregation engulfed her in a hug. Then they moved to offer words of support to the sandy-haired 17-year-old sitting in the pews. In the first of many awkward mistakes the family would later laugh about, it was Caleb—Emmie’s identical twin.
After that sermon, a “new normal” set in. On a Saturday night soon after, they had their first “out” outing. Kate took Emmie—whose hair was still short and chest was flat—to buy a prom dress at David’s Bridal. She feared someone would point or laugh, but the crowds of brides and bridesmaids in the dressing room offered only compliments.
Though she hadn’t initially considered surgery, after a couple of months Emmie had grown frustrated by the tucking and taping required to fit into women’s clothes. That fall, her senior year of high school, she decided to do it.
But waking up after the operation, Emmie felt none of the immediate relief she’d expected. In the recovery room her earbuds played a soothing loop of Bon Iver and Simon and Garfunkel, but it didn’t drown out her disappointment and fear. In retrospect, she thought, hadn’t life before been OK?
It wasn’t until months later, when she was home and could walk and sit again, that Emmie knew she’d made the right choice. “If you’re not living freely that’s time wasted, and I felt my time was wasted pretending to be a boy,” she says. “It was the best decision in my life.”
Now, halfway through a gap year, she’s applying to college theater programs. It’s strange, she says, knowing that her future classmates may watch Johnson’s film and learn the most intimate details of her life. She’s hopeful that her participation will evolve the public’s understanding of gender reassignment surgery. “It’s not science fiction or mythology,” Emmie says. “It’s what happens to women just trying to be at peace with themselves and their bodies.”
Related Topics
You may also like.

Meet the 5 iconic women being honored on new quarters in 2024
Source page for gender identity map.

How science is helping us understand gender
Redefining gender.

Prehistoric female hunter discovery upends gender role assumptions
- Environment
- Paid Content
History & Culture
- History & Culture
- Terms of Use
- Privacy Policy
- Your US State Privacy Rights
- Children's Online Privacy Policy
- Interest-Based Ads
- About Nielsen Measurement
- Do Not Sell or Share My Personal Information
- Nat Geo Home
- Attend a Live Event
- Book a Trip
- Inspire Your Kids
- Shop Nat Geo
- Visit the D.C. Museum
- Learn About Our Impact
- Support Our Mission
- Advertise With Us
- Customer Service
- Renew Subscription
- Manage Your Subscription
- Work at Nat Geo
- Sign Up for Our Newsletters
- Contribute to Protect the Planet
Copyright © 1996-2015 National Geographic Society Copyright © 2015-2024 National Geographic Partners, LLC. All rights reserved
Your browser is out-of-date!
Internet Explorer 11 has been retired by Microsoft as of June 15, 2022. To get the best experience on this website, we recommend using a modern browser, such as Safari, Chrome or Edge.
What Is Gender Confirmation Surgery?
Learn about transgender surgery: male-to-female, female-to-male.

Transgender individuals feel that the sex they were assigned at birth, such as male or female, does not match the gender with which they identify. For example, a baby assigned “male” at birth may grow up with a sense of feeling they are female.
As a result of feeling that they were born in the wrong gender, some transgender individuals experience psychological distress known as “ gender dysphoria ” and take various actions to better align their gender identification with their external appearance. For some individuals, the transition process from one gender to another may include medical treatments, such as hormone therapy and gender confirmation surgery.
What is hormone therapy?
Usually the first step in the gender transition process, hormone therapy is intended to suppress the assigned sex characteristics, promote the desired characteristics, or both. For example, men who identify as women may take anti-androgens to block production of the male hormone testosterone, as well as estrogen to appear more feminine. Similarly, women who identify as men may take testosterone to develop more masculine features, such as facial hair.
What is gender confirmation surgery?
If hormone therapy does not have the desired effectiveness, gender confirmation surgery may be an option. Also called gender reassignment surgery, the goal of this procedure is to create the outward physical appearance of the gender with which the person identifies. “Top surgery” refers to surgery above the waist, while “bottom surgery” refers to surgery below the waist.
Transgender surgery is major surgery and generally not considered reversible, so many healthcare providers require transgender individuals to complete several steps before they will proceed with surgery. These may include requiring a formal diagnosis of gender dysphoria and having counseling to determine their psychological readiness for surgery.
“Gender confirmation surgery involves both physical and psychological aspects,” says Manish Champaneria, MD , a plastic surgeon at Scripps Clinic. “Scripps follows the recommendations of the World Professional Association for Transgender Health (WPATH) regarding preparation for surgery, including having a referral from a mental health provider. Patients undergoing surgery are urged to live as the gender they identify as for at least 12 months before having the procedure.”
Gender confirmation surgery options
Scripps offers gender confirmation surgery procedures for both male-to-female (MTF) or transwomen patients, and female-to-male (FTM) or transmen patients.
Top surgery
Performed on the chest, top surgery is intended to create a more gender-confirming physique. Top surgery procedures include mastectomies for transmen and breast augmentation for transwomen. In most cases, top surgeries are completed in a single procedure.
MTF top surgery
MTF top surgery to augment the breasts may involve fat transfer or breast implants. In a fat transfer procedure, the surgeon removes fat from other parts of the body and injects it into the breasts. Fat transfer may be recommended for patients who wish to increase breast size without breast implants.
Patients who seek larger breasts may choose to have breast implants, which are surgically placed under the chest muscles to enhance breast size and shape. The surgeon and patient together determine the most appropriate size and type of implants.
FTM top surgery
In FTM top surgery, the surgeon removes breast tissue and manipulates the remaining tissue to create a more masculine appearance.
Facial feminization surgery
During MTF facial feminization surgery, the surgeon restructures masculine facial features to achieve a more feminine look. This involves reshaping bones and soft tissues and may be performed as a single procedure or in several stages.
Body contouring
Using various procedures, body contouring reshapes the body to create a more masculine or feminine physique. Specific procedures depend on the patient’s original body shape and desired outcomes. For example, fat transfer may be used to reduce curves in some areas and create them in others.
“We understand that gender confirmation surgery is a life-changing procedure that requires multidisciplinary medical expertise and experience, and we work very closely with our transgender patients every step of the way,” says Dr. Champaneria. “We urge anyone considering this surgery to start by talking with a trusted and physician who is experienced in transgender procedures.”
Related tags:
- Health and Wellness
- Women’s Health
- Men’s Health

The Debate About Sex Assigned at Birth
Accounting for sex in biological research is complicated..
Posted June 29, 2024 | Reviewed by Devon Frye
- There has been a lot of rethinking about how we define biological sex of late.
- Some biological scientists struggle with these changes because of the way studies are traditionally conducted.
- We need a middle path to understand the true nature of sex and gender.
It is becoming increasingly common in many medical and academic circles to stop referring to a person as “male” or “female” and instead refer to their “sex assigned at birth.” The motivation behind this is a welcome desire to understand the needs of transgender and gender-diverse people who are often the victims of discrimination and stigma , which can lead to significant disparities in health care and imperil the health of sexual minority people.
Yet the move away from talking about sex in biological research and medicine may also be problematic in certain circumstances. As discussed in a May 15 article in the journal Nature , “ Neglecting sex and gender in research is a public-health risk ,” there is no question that differences exist between men and women in a variety of health outcomes.
The authors write that three things about sex and gender must be considered in biological research and medical practice: “How sex and gender can have huge effects on health outcomes; how these effects are often disregarded in basic research and clinical trials; and that change can come only through increasing awareness among all stakeholders of the importance” of rethinking how we approach the topics of sex and gender.
Is Sex Assigned at Birth Problematic?
A philosopher, Alex Byrne, and an evolutionary biologist, Carole K. Hooven, recently decried the use of the phrase “sex assigned at birth” in a New York Times op-ed. “Sex is a fundamental biological feature with significant consequences for our species,” they wrote last April, “so there are costs to encouraging misconceptions about it.”
They go on to reiterate the points made in the Nature article, emphasizing that there are unmistakable differences in many aspects of health that are based on an individual’s biological sex, and state that the phrase sex assigned at birth “can also suggest that there is no objective reality behind ‘male’ and ‘female,’ no biological categories to which the words refer.” Byrne and Hooven reject the idea promulgated by philosophers like Michel Foucault and Judith Butler that “sex is somehow a cultural production, the result of labeling babies male and female” and insist that “Sexed organisms were present on Earth at least a billion years ago, and males and females would have been around even if humans never evolved.”


Health Outcomes Differ Between Males and Females
As noted in the Nature article, “For Alzheimer’s [disease] and many other diseases that are common causes of death, including cardiovascular diseases, cancer, chronic respiratory conditions, and diabetes, a person’s sex and gender can influence their risk of developing the disease, how quickly and accurately they are diagnosed, what treatment they receive and how they fare.”
Note that these authors refer both to sex and gender. Sex is generally conceived of as encompassing the biological differences between males and females, based on genetics and sex hormones , whereas gender includes “the social, psychological, cultural and behavioral aspects of being a man or woman (whether cisgender or transgender), non-binary or identifying with one or more other evolving terms.”
The Nature authors point to a host of differences in the expression of diseases like heart attacks, strokes, and cancer. Examples include that men develop cardiovascular disease earlier than women, women are more likely to develop Alzheimer’s disease than men, cancer chemotherapies work better in women than men and so on—to which we would add that depression and anxiety disorders are more common in women than men.
Some of these may be explained by sociocultural factors. For instance, men are more likely to smoke tobacco than women and this increases the risk for cardiovascular disease and many forms of cancer.
Other differences, however, in disease expression and health outcomes may be due to more clearly biological factors and these are, according to the Nature authors, substantially understudied. “Take the sex of the cell lines that are stored in commercial cell banks,” they point out, “which have been studied for decades and are the source of today’s textbook knowledge.” In many cases, male lines outnumber female lines.

On a clinical level, women are underrepresented in many trials of new therapeutics, leading to a significant lack of knowledge about differences in treatment responses between the sexes. This can have disastrous consequences. “Between 1976 and 2000… eight prescription drugs were retracted from the U.S. market because inadequate clinical testing in women had failed to identify that the drugs put women at greater risk of developing health problems than men.”
The debate about how to talk about sex is clearly heated. On the one hand, there are risks to ignoring biological differences between men and women and to taking the position that sex lacks any objective reality. On the other hand, insisting that everything about sex is biological and determined by genes and hormones ignores the complexities of human psychology and denies the reality of people who do not conform to binary sex categories.
More Nuanced Research Needed
Clearly, a more nuanced approach is necessary. An example of this is research recently reported from the University of Montreal that examined both biological factors and psychosocial factors that determine cognitive differences.
It is known that in general women perform better than men on tests of verbal and fine motor ability, whereas men do better on spatial and mental rotation tasks. The Montreal investigators recruited 222 adults who represented several different subgroups: cisgender heterosexual men, cisgender non-heterosexual men, cisgender heterosexual women, cisgender non-heterosexual women, and gender diverse people. The research study participants were administered a series of cognitive tests, gave saliva samples for measurement of sex hormones, and completed self-report questionnaires about psychosocial variables.
The study found that “biological factors seem to better explain differences in male-typed cognitive tasks (i.e., spatial), while psychosocial factors seem to better explain differences in female-typed cognitive tasks (i.e., verbal).” Hence, sex was associated with cognitive abilities commonly found to be stronger in men than women whereas gender was associated with cognitive abilities commonly found to be stronger in women than men.
Of course, studies like this one need to be replicated before we draw conclusions, but this one represents a welcome accounting of a variety of factors to try to disentangle differences between males and females, some based on biology and others on cultural and psychological factors. Until we have more of this kind of work, we will be left in the dark about the fundamental ways in which men and women differ, making us ignorant of factors with profound influence on the expression and course of many human diseases.
For now, we will continue to use the phrase “sex assigned at birth” because we recognize the importance of the inclusion of people who don’t identify as binary. However, we will also support research aimed at furthering our understanding of the ways the complexity of sex and gender affects human health.

Sara Gorman, PhD, MPH, is a public health specialist, and Jack M. Gorman, MD, is a psychiatrist.
- Find a Therapist
- Find a Treatment Center
- Find a Psychiatrist
- Find a Support Group
- Find Online Therapy
- United States
- Brooklyn, NY
- Chicago, IL
- Houston, TX
- Los Angeles, CA
- New York, NY
- Portland, OR
- San Diego, CA
- San Francisco, CA
- Seattle, WA
- Washington, DC
- Asperger's
- Bipolar Disorder
- Chronic Pain
- Eating Disorders
- Passive Aggression
- Personality
- Goal Setting
- Positive Psychology
- Stopping Smoking
- Low Sexual Desire
- Relationships
- Child Development
- Self Tests NEW
- Therapy Center
- Diagnosis Dictionary
- Types of Therapy

Sticking up for yourself is no easy task. But there are concrete skills you can use to hone your assertiveness and advocate for yourself.
- Emotional Intelligence
- Gaslighting
- Affective Forecasting
- Neuroscience
Putting numbers on the rise in children seeking gender care
By ROBIN RESPAUT and CHAD TERHUNE
Filed Oct. 6, 2022, 11 a.m. GMT

Thousands of children in the United States now openly identify as a gender different from the one they were assigned at birth, their numbers surging amid growing recognition of transgender identity and rights even as they face persistent prejudice and discrimination.
As the number of transgender children has grown, so has their access to gender-affirming care, much of it provided at scores of clinics at major hospitals.
Reliable counts of adolescents receiving gender-affirming treatment have long been guesswork – until now. Reuters worked with health technology company Komodo Health Inc to identify how many youths have sought and received care. The data show that more and more families across the country are grappling with profound questions about what type of care to pursue for their children, placing them at the center of a vitriolic national political debate over what it means to protect youth who identify as transgender.
Diagnoses of youths with gender dysphoria surge
In 2021, about 42,000 children and teens across the United States received a diagnosis of gender dysphoria, nearly triple the number in 2017, according to data Komodo compiled for Reuters. Gender dysphoria is defined as the distress caused by a discrepancy between a person’s gender identity and the one assigned to them at birth.
Overall, the analysis found that at least 121,882 children ages 6 to 17 were diagnosed with gender dysphoria from 2017 through 2021. Reuters found similar trends when it requested state-level data on diagnoses among children covered by Medicaid, the public insurance program for lower-income families.
Gender-affirming care for youths takes several forms, from social recognition of a preferred name and pronouns to medical interventions such as hormone therapy and, sometimes, surgery. A small but increasing number of U.S. children diagnosed with gender dysphoria are choosing medical interventions to express their identity and help alleviate their distress.
These medical treatments don’t begin until the onset of puberty, typically around age 10 or 11.
For children at this age and stage of development, puberty-blocking medications are an option. These drugs, known as GnRH agonists, suppress the release of the sex hormones testosterone and estrogen. The U.S. Food and Drug Administration has approved the drugs to treat prostate cancer, endometriosis and central precocious puberty, but not gender dysphoria. Their off-label use in gender-affirming care, while legal, lacks the support of clinical trials to establish their safety for such treatment.
Over the last five years, there were at least 4,780 adolescents who started on puberty blockers and had a prior gender dysphoria diagnosis.
This tally and others in the Komodo analysis are likely an undercount because they didn’t include treatment that wasn’t covered by insurance and were limited to pediatric patients with a gender dysphoria diagnosis. Practitioners may not log this diagnosis when prescribing treatment.
By suppressing sex hormones, puberty-blocking medications stop the onset of secondary sex characteristics, such as breast development and menstruation in adolescents assigned female at birth. For those assigned male at birth, the drugs inhibit development of a deeper voice and an Adam’s apple and growth of facial and body hair. They also limit growth of genitalia.
Without puberty blockers, such physical changes can cause severe distress in many transgender children. If an adolescent stops the medication, puberty resumes.
The medications are administered as injections, typically every few months, or through an implant under the skin of the upper arm.
After suppressing puberty, a child may pursue hormone treatments to initiate a puberty that aligns with their gender identity. Those for whom the opportunity to block puberty has already passed or who declined the option may also pursue hormone therapy.
At least 14,726 minors started hormone treatment with a prior gender dysphoria diagnosis from 2017 through 2021, according to the Komodo analysis.
Hormones – testosterone for adolescents assigned female at birth and estrogen for those assigned male – promote development of secondary sex characteristics. Adolescents assigned female at birth who take testosterone may notice that fat is redistributed from the hips and thighs to the abdomen. Arms and legs may appear more muscular. The brow and jawline may become more pronounced. Body hair may coarsen and thicken. Teens assigned male at birth who take estrogen may notice the hair on their body softens and thins. Fat may be redistributed from the abdomen to the buttocks and thighs. Their testicles may shrink and sex drive diminish. Some changes from hormone treatment are permanent.
Hormones are taken in a variety of ways: injections, pills, patches and gels. Some minors will continue to take hormones for many years well into adulthood, or they may stop if they achieve the physical traits they want.
Hormone treatment may leave an adolescent infertile, especially if the child also took puberty blockers at an early age. That and other potential side effects are not well-studied, experts say.
The ultimate step in gender-affirming medical treatment is surgery, which is uncommon in patients under age 18. Some children’s hospitals and gender clinics don’t offer surgery to minors, requiring that they be adults before deciding on procedures that are irreversible and carry a heightened risk of complications.
The Komodo analysis of insurance claims found 56 genital surgeries among patients ages 13 to 17 with a prior gender dysphoria diagnosis from 2019 to 2021. Among teens, “top surgery” to remove breasts is more common. In the three years ending in 2021, at least 776 mastectomies were performed in the United States on patients ages 13 to 17 with a gender dysphoria diagnosis, according to Komodo’s data analysis of insurance claims. This tally does not include procedures that were paid for out of pocket.
A note on the data
Komodo’s analysis draws on full or partial health insurance claims for about 330 million U.S. patients over the five years from 2017 to 2021, including patients covered by private health plans and public insurance like Medicaid. The data include roughly 40 million patients annually, ages 6 through 17, and comprise health insurance claims that document diagnoses and procedures administered by U.S. clinicians and facilities.
To determine the number of new patients who initiated puberty blockers or hormones, or who received an initial dysphoria diagnosis, Komodo looked back at least one year prior in each patient’s record. For the surgery data, Komodo counted multiple procedures on a single day as one procedure.
For the analysis of pediatric patients initiating puberty blockers or hormones, Komodo searched for patients with a prior gender dysphoria diagnosis. Patients with a diagnosis of central precocious puberty were removed. A total of 17,683 patients, ages 6 through 17, with a prior gender dysphoria diagnosis initiated either puberty blockers or hormones or both during the five-year period. Of these, 4,780 patients had initiated puberty blockers and 14,726 patients had initiated hormone treatment.
Youth in Transition
By Robin Respaut and Chad Terhune
Photo editing: Corrine Perkins
Art direction: John Emerson
Edited by Michele Gershberg and John Blanton
- Follow Reuters Investigates
Other Reuters investigations
- Sex and Gender Identity
- What's intersex?
- What are gender roles and stereotypes?
There’s a lot more to being male, female, or any gender than the sex assigned at birth. Your biological or assigned sex does not always tell your complete story.
What are the differences between sex, gender, and gender identity?
It’s common for people to confuse sex, gender, and gender identity. But they’re actually all different things.
Sex is a label — male or female — that you’re assigned by a doctor at birth based on the genitals you’re born with and the chromosomes you have. It goes on your birth certificate.
Gender is much more complex: It’s a social and legal status, and set of expectations from society, about behaviors, characteristics, and thoughts. Each culture has standards about the way that people should behave based on their gender. This is also generally male or female. But instead of being about body parts, it’s more about how you’re expected to act, because of your sex.
Gender identity is how you feel inside and how you express your gender through clothing, behavior, and personal appearance. It’s a feeling that begins very early in life.
What’s assigned sex (aka “biological sex”)?
Assigned sex is a label that you’re given at birth based on medical factors, including your hormones, chromosomes, and genitals. Most people are assigned male or female, and this is what’s put on their birth certificates.
When someone’s sexual and reproductive anatomy doesn’t seem to fit the typical definitions of female or male, they may be described as intersex .
Some people call the sex we’re assigned at birth “biological sex.” But this term doesn’t fully capture the complex biological, anatomical, and chromosomal variations that can occur. Having only two options (biological male or biological female) might not describe what’s going on inside a person’s body.
Instead of saying “biological sex,” some people use the phrase “assigned male at birth” or “assigned female at birth.” This acknowledges that someone (often a doctor) is making a decision for someone else. The assignment of a biological sex may or may not align with what’s going on with a person’s body, how they feel, or how they identify.
The factors that determine our assigned sex begin as early as fertilization .
Each sperm has either an X or a Y chromosome in it. All eggs have an X chromosome.
When sperm fertilizes an egg, its X or Y chromosome combines with the X chromosome of the egg.
A person with XX chromosomes usually has female sex and reproductive organs, and is therefore usually assigned biologically female.
A person with XY chromosomes usually has male sex and reproductive organs, and is therefore usually assigned biologically male.
Other arrangements of chromosomes, hormones, and body parts can happen, which results in someone being intersex .
What’s gender?
Gender is much bigger and more complicated than assigned sex. Gender includes gender roles , which are expectations society and people have about behaviors, thoughts, and characteristics that go along with a person’s assigned sex.
For example, ideas about how men and women are expected to behave, dress, and communicate all contribute to gender. Gender is also a social and legal status as girls and boys, men, and women.
It’s easy to confuse sex and gender. Just remember that biological or assigned sex is about biology, anatomy, and chromosomes. Gender is society’s set of expectations, standards, and characteristics about how men and women are supposed to act.
What’s gender identity?
Your gender identity is how you feel inside and how you express those feelings. Clothing, appearance, and behaviors can all be ways to express your gender identity.
Most people feel that they’re either male or female. Some people feel like a masculine female, or a feminine male. Some people feel neither male nor female. These people may choose labels such as “genderqueer,” “gender variant,” or “gender fluid.” Your feelings about your gender identity begin as early as age 2 or 3.
Some people’s assigned sex and gender identity are pretty much the same, or in line with each other. These people are called cisgender. Other people feel that their assigned sex is of the other gender from their gender identity (i.e., assigned sex is female, but gender identity is male). These people are called transgender or trans. Not all transgender people share the same exact identity.
Are you a teenager who wants support?
Q Chat Space hosts live chats where LGBTQ+ teens can give and receive support.
- imi offers guides to help queer teens explore their identity and care for their mental health.
Book an Appointment
Please enter your age and the first day of your last period for more accurate abortion options. Your information is private and anonymous.
Or call 1-800-230-7526
This website uses cookies
Planned Parenthood cares about your data privacy. We and our third-party vendors use cookies and other tools to collect, store, monitor, and analyze information about your interaction with our site to improve performance, analyze your use of our sites and assist in our marketing efforts. You may opt out of the use of these cookies and other tools at any time by visiting Cookie Settings . By clicking “Allow All Cookies” you consent to our collection and use of such data, and our Terms of Use . For more information, see our Privacy Notice .
Cookie Settings
Planned Parenthood cares about your data privacy. We and our third-party vendors, use cookies, pixels, and other tracking technologies to collect, store, monitor, and process certain information about you when you access and use our services, read our emails, or otherwise engage with us. The information collected might relate to you, your preferences, or your device. We use that information to make the site work, analyze performance and traffic on our website, to provide a more personalized web experience, and assist in our marketing efforts. We also share information with our social media, advertising, and analytics partners. You can change your default settings according to your preference. You cannot opt-out of required cookies when utilizing our site; this includes necessary cookies that help our site to function (such as remembering your cookie preference settings). For more information, please see our Privacy Notice .
We use online advertising to promote our mission and help constituents find our services. Marketing pixels help us measure the success of our campaigns.
Performance
We use qualitative data, including session replay, to learn about your user experience and improve our products and services.
We use web analytics to help us understand user engagement with our website, trends, and overall reach of our products.
- Type 2 Diabetes
- Heart Disease
- Digestive Health
- Multiple Sclerosis
- Diet & Nutrition
- Health Insurance
- Public Health
- Patient Rights
- Caregivers & Loved Ones
- End of Life Concerns
- Health News
- Thyroid Test Analyzer
- Doctor Discussion Guides
- Hemoglobin A1c Test Analyzer
- Lipid Test Analyzer
- Complete Blood Count (CBC) Analyzer
- What to Buy
- Editorial Process
- Meet Our Medical Expert Board
Gender Confirmation Surgery (GCS)
What is Gender Confirmation Surgery?
- Transfeminine Tr
Transmasculine Transition
- Traveling Abroad
Choosing a Surgeon
Gender confirmation surgery (GCS), known clinically as genitoplasty, are procedures that surgically confirm a person's gender by altering the genitalia and other physical features to align with their desired physical characteristics. Gender confirmation surgeries are also called gender affirmation procedures. These are both respectful terms.
Gender dysphoria , an experience of misalignment between gender and sex, is becoming more widely diagnosed. People diagnosed with gender dysphoria are often referred to as "transgender," though one does not necessarily need to experience gender dysphoria to be a member of the transgender community. It is important to note there is controversy around the gender dysphoria diagnosis. Many disapprove of it, noting that the diagnosis suggests that being transgender is an illness.
Ellen Lindner / Verywell
Transfeminine Transition
Transfeminine is a term inclusive of trans women and non-binary trans people assigned male at birth.
Gender confirmation procedures that a transfeminine person may undergo include:
- Penectomy is the surgical removal of external male genitalia.
- Orchiectomy is the surgical removal of the testes.
- Vaginoplasty is the surgical creation of a vagina.
- Feminizing genitoplasty creates internal female genitalia.
- Breast implants create breasts.
- Gluteoplasty increases buttock volume.
- Chondrolaryngoplasty is a procedure on the throat that can minimize the appearance of Adam's apple .
Feminizing hormones are commonly used for at least 12 months prior to breast augmentation to maximize breast growth and achieve a better surgical outcome. They are also often used for approximately 12 months prior to feminizing genital surgeries.
Facial feminization surgery (FFS) is often done to soften the lines of the face. FFS can include softening the brow line, rhinoplasty (nose job), smoothing the jaw and forehead, and altering the cheekbones. Each person is unique and the procedures that are done are based on the individual's need and budget,
Transmasculine is a term inclusive of trans men and non-binary trans people assigned female at birth.
Gender confirmation procedures that a transmasculine person may undergo include:
- Masculinizing genitoplasty is the surgical creation of external genitalia. This procedure uses the tissue of the labia to create a penis.
- Phalloplasty is the surgical construction of a penis using a skin graft from the forearm, thigh, or upper back.
- Metoidioplasty is the creation of a penis from the hormonally enlarged clitoris.
- Scrotoplasty is the creation of a scrotum.
Procedures that change the genitalia are performed with other procedures, which may be extensive.
The change to a masculine appearance may also include hormone therapy with testosterone, a mastectomy (surgical removal of the breasts), hysterectomy (surgical removal of the uterus), and perhaps additional cosmetic procedures intended to masculinize the appearance.
Paying For Gender Confirmation Surgery
Medicare and some health insurance providers in the United States may cover a portion of the cost of gender confirmation surgery.
It is unlawful to discriminate or withhold healthcare based on sex or gender. However, many plans do have exclusions.
For most transgender individuals, the burden of financing the procedure(s) is the main difficulty in obtaining treatment. The cost of transitioning can often exceed $100,000 in the United States, depending upon the procedures needed.
A typical genitoplasty alone averages about $18,000. Rhinoplasty, or a nose job, averaged $5,409 in 2019.
Traveling Abroad for GCS
Some patients seek gender confirmation surgery overseas, as the procedures can be less expensive in some other countries. It is important to remember that traveling to a foreign country for surgery, also known as surgery tourism, can be very risky.
Regardless of where the surgery will be performed, it is essential that your surgeon is skilled in the procedure being performed and that your surgery will be performed in a reputable facility that offers high-quality care.
When choosing a surgeon , it is important to do your research, whether the surgery is performed in the U.S. or elsewhere. Talk to people who have already had the procedure and ask about their experience and their surgeon.
Before and after photos don't tell the whole story, and can easily be altered, so consider asking for a patient reference with whom you can speak.
It is important to remember that surgeons have specialties and to stick with your surgeon's specialty. For example, you may choose to have one surgeon perform a genitoplasty, but another to perform facial surgeries. This may result in more expenses, but it can result in a better outcome.
A Word From Verywell
Gender confirmation surgery is very complex, and the procedures that one person needs to achieve their desired result can be very different from what another person wants.
Each individual's goals for their appearance will be different. For example, one individual may feel strongly that breast implants are essential to having a desirable and feminine appearance, while a different person may not feel that breast size is a concern. A personalized approach is essential to satisfaction because personal appearance is so highly individualized.
Davy Z, Toze M. What is gender dysphoria? A critical systematic narrative review . Transgend Health . 2018;3(1):159-169. doi:10.1089/trgh.2018.0014
Morrison SD, Vyas KS, Motakef S, et al. Facial Feminization: Systematic Review of the Literature . Plast Reconstr Surg. 2016;137(6):1759-70. doi:10.1097/PRS.0000000000002171
Hadj-moussa M, Agarwal S, Ohl DA, Kuzon WM. Masculinizing Genital Gender Confirmation Surgery . Sex Med Rev . 2019;7(1):141-155. doi:10.1016/j.sxmr.2018.06.004
Dowshen NL, Christensen J, Gruschow SM. Health Insurance Coverage of Recommended Gender-Affirming Health Care Services for Transgender Youth: Shopping Online for Coverage Information . Transgend Health . 2019;4(1):131-135. doi:10.1089/trgh.2018.0055
American Society of Plastic Surgeons. Rhinoplasty nose surgery .
Rights Group: More U.S. Companies Covering Cost of Gender Reassignment Surgery. CNS News. http://cnsnews.com/news/article/rights-group-more-us-companies-covering-cost-gender-reassignment-surgery
The Sex Change Capital of the US. CBS News. http://www.cbsnews.com/2100-3445_162-4423154.html
By Jennifer Whitlock, RN, MSN, FN Jennifer Whitlock, RN, MSN, FNP-C, is a board-certified family nurse practitioner. She has experience in primary care and hospital medicine.
Thank you for visiting nature.com. You are using a browser version with limited support for CSS. To obtain the best experience, we recommend you use a more up to date browser (or turn off compatibility mode in Internet Explorer). In the meantime, to ensure continued support, we are displaying the site without styles and JavaScript.
- View all journals
- Explore content
- About the journal
- Publish with us
- Sign up for alerts
- 1998 Abstracts The American Pediatric Society and The Society for Pediatric Research
- Published: 01 April 1998
Gender Assignment at Birth: Three Cases of Reassignment/Ambiguity At or Beyond Adolesence † 466
- Chanika Phornphutkul 1 ,
- Charlotte M Boney 1 ,
- Anne Fausto-Sterling 1 &
- Philip A Gruppuso 1
Pediatric Research volume 43 , page 82 ( 1998 ) Cite this article
3151 Accesses
6 Altmetric
Metrics details
Gender assignment at birth in cases of ambiguous genitalia (AG) has long been based on anatomical appearance, adequacy of the phallus and/or response to testosterone. Recent reports have questioned the validity of this approach. We have encountered three patients born with AG, all with 46XY karyotype, whose gender assignments were made shortly after birth but later questioned or altered by the patients themselves. CASE 1: This patient, exposed to dilantin in utero , was born with a small phallus (considered to be an enlarged clitoris) and bilaterally descended testes in the labioscrotal fold. Female gender was assigned. No specific hormonal diagnosis was made; however, androgen insensitivity and 5α-reductase deficiency were ruled out. Gonadectomy was performed at 1 mo. of age. Starting at age 4 yr., the patient described herself as not feeling “like a girl”. She was described as “tomboyish” . At 12 y.o. she was started on estrogen but later discontinued the therapy. At age 17 yr. she declared herself male, changed her name, had mammoplasty and began testosterone therapy. CASE 2: An infant, born with AG and non-palpable gonads was assigned male gender at birth and raised as a boy. No specific diagnosis was made. Throughout childhood, he did not accept being told he was “a normal boy” . Hypospadias repair and gonadectomy were done at 5 y.o. At age 11 yr. testosterone was started but the patient did not accept the treatment and has been non-compliant since. Testicular prostheses were placed at 13 y.o. and removed at the patient's request at 18 y.o. Now, at age 27 yr., the patient identifies himself as “intersex” . CASE 3: This patient, born with AG and non-palpable gonads, was assigned female gender at birth because of the presence of a uterus and microphallus. Ovotestes were removed surgically. Vaginoplasty and clitoral recession were performed subsequently. Shortly after starting estrogen treatment at age 12, the patient expressed resistance to hormonal therapy because she was uncertain about her gender identity. SUMMARY: In all three cases, gender assignment was accepted by the patients' parents, but not by the patients themselves. These three cases inidicate that the traditional approach to gender assignment in newborns with AG may be associated with lack of acceptance on the patient's part, thus placing patients at risk for unwanted and unnecessary surgery and/or hormonal therapy.
Author information
Authors and affiliations.
Pediatrics, Rhode Island Hospital and Brown University, Providence, RI
Chanika Phornphutkul, Charlotte M Boney, Anne Fausto-Sterling & Philip A Gruppuso
You can also search for this author in PubMed Google Scholar
Rights and permissions
Reprints and permissions
About this article
Cite this article.
Phornphutkul, C., Boney, C., Fausto-Sterling, A. et al. Gender Assignment at Birth: Three Cases of Reassignment/Ambiguity At or Beyond Adolesence † 466. Pediatr Res 43 (Suppl 4), 82 (1998). https://doi.org/10.1203/00006450-199804001-00487
Download citation
Issue Date : 01 April 1998
DOI : https://doi.org/10.1203/00006450-199804001-00487
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
Quick links
- Explore articles by subject
- Guide to authors
- Editorial policies
- Patient Care & Health Information
- Tests & Procedures
- Feminizing surgery
Feminizing surgery, also called gender-affirming surgery or gender-confirmation surgery, involves procedures that help better align the body with a person's gender identity. Feminizing surgery includes several options, such as top surgery to increase the size of the breasts. That procedure also is called breast augmentation. Bottom surgery can involve removal of the testicles, or removal of the testicles and penis and the creation of a vagina, labia and clitoris. Facial procedures or body-contouring procedures can be used as well.
Not everybody chooses to have feminizing surgery. These surgeries can be expensive, carry risks and complications, and involve follow-up medical care and procedures. Certain surgeries change fertility and sexual sensations. They also may change how you feel about your body.
Your health care team can talk with you about your options and help you weigh the risks and benefits.
Products & Services
- A Book: Mayo Clinic Family Health Book
- Available Sexual Health Solutions at Mayo Clinic Store
- Newsletter: Mayo Clinic Health Letter — Digital Edition
Why it's done
Many people seek feminizing surgery as a step in the process of treating discomfort or distress because their gender identity differs from their sex assigned at birth. The medical term for this is gender dysphoria.
For some people, having feminizing surgery feels like a natural step. It's important to their sense of self. Others choose not to have surgery. All people relate to their bodies differently and should make individual choices that best suit their needs.
Feminizing surgery may include:
- Removal of the testicles alone. This is called orchiectomy.
- Removal of the penis, called penectomy.
- Removal of the testicles.
- Creation of a vagina, called vaginoplasty.
- Creation of a clitoris, called clitoroplasty.
- Creation of labia, called labioplasty.
- Breast surgery. Surgery to increase breast size is called top surgery or breast augmentation. It can be done through implants, the placement of tissue expanders under breast tissue, or the transplantation of fat from other parts of the body into the breast.
- Plastic surgery on the face. This is called facial feminization surgery. It involves plastic surgery techniques in which the jaw, chin, cheeks, forehead, nose, and areas surrounding the eyes, ears or lips are changed to create a more feminine appearance.
- Tummy tuck, called abdominoplasty.
- Buttock lift, called gluteal augmentation.
- Liposuction, a surgical procedure that uses a suction technique to remove fat from specific areas of the body.
- Voice feminizing therapy and surgery. These are techniques used to raise voice pitch.
- Tracheal shave. This surgery reduces the thyroid cartilage, also called the Adam's apple.
- Scalp hair transplant. This procedure removes hair follicles from the back and side of the head and transplants them to balding areas.
- Hair removal. A laser can be used to remove unwanted hair. Another option is electrolysis, a procedure that involves inserting a tiny needle into each hair follicle. The needle emits a pulse of electric current that damages and eventually destroys the follicle.
Your health care provider might advise against these surgeries if you have:
- Significant medical conditions that haven't been addressed.
- Behavioral health conditions that haven't been addressed.
- Any condition that limits your ability to give your informed consent.
Like any other type of major surgery, many types of feminizing surgery pose a risk of bleeding, infection and a reaction to anesthesia. Other complications might include:
- Delayed wound healing
- Fluid buildup beneath the skin, called seroma
- Bruising, also called hematoma
- Changes in skin sensation such as pain that doesn't go away, tingling, reduced sensation or numbness
- Damaged or dead body tissue — a condition known as tissue necrosis — such as in the vagina or labia
- A blood clot in a deep vein, called deep vein thrombosis, or a blood clot in the lung, called pulmonary embolism
- Development of an irregular connection between two body parts, called a fistula, such as between the bladder or bowel into the vagina
- Urinary problems, such as incontinence
- Pelvic floor problems
- Permanent scarring
- Loss of sexual pleasure or function
- Worsening of a behavioral health problem
Certain types of feminizing surgery may limit or end fertility. If you want to have biological children and you're having surgery that involves your reproductive organs, talk to your health care provider before surgery. You may be able to freeze sperm with a technique called sperm cryopreservation.
How you prepare
Before surgery, you meet with your surgeon. Work with a surgeon who is board certified and experienced in the procedures you want. Your surgeon talks with you about your options and the potential results. The surgeon also may provide information on details such as the type of anesthesia that will be used during surgery and the kind of follow-up care that you may need.
Follow your health care team's directions on preparing for your procedures. This may include guidelines on eating and drinking. You may need to make changes in the medicine you take and stop using nicotine, including vaping, smoking and chewing tobacco.
Because feminizing surgery might cause physical changes that cannot be reversed, you must give informed consent after thoroughly discussing:
- Risks and benefits
- Alternatives to surgery
- Expectations and goals
- Social and legal implications
- Potential complications
- Impact on sexual function and fertility
Evaluation for surgery
Before surgery, a health care provider evaluates your health to address any medical conditions that might prevent you from having surgery or that could affect the procedure. This evaluation may be done by a provider with expertise in transgender medicine. The evaluation might include:
- A review of your personal and family medical history
- A physical exam
- A review of your vaccinations
- Screening tests for some conditions and diseases
- Identification and management, if needed, of tobacco use, drug use, alcohol use disorder, HIV or other sexually transmitted infections
- Discussion about birth control, fertility and sexual function
You also may have a behavioral health evaluation by a health care provider with expertise in transgender health. That evaluation might assess:
- Gender identity
- Gender dysphoria
- Mental health concerns
- Sexual health concerns
- The impact of gender identity at work, at school, at home and in social settings
- The role of social transitioning and hormone therapy before surgery
- Risky behaviors, such as substance use or use of unapproved hormone therapy or supplements
- Support from family, friends and caregivers
- Your goals and expectations of treatment
- Care planning and follow-up after surgery
Other considerations
Health insurance coverage for feminizing surgery varies widely. Before you have surgery, check with your insurance provider to see what will be covered.
Before surgery, you might consider talking to others who have had feminizing surgery. If you don't know someone, ask your health care provider about support groups in your area or online resources you can trust. People who have gone through the process may be able to help you set your expectations and offer a point of comparison for your own goals of the surgery.
What you can expect
Facial feminization surgery.
Facial feminization surgery may involve a range of procedures to change facial features, including:
- Moving the hairline to create a smaller forehead
- Enlarging the lips and cheekbones with implants
- Reshaping the jaw and chin
- Undergoing skin-tightening surgery after bone reduction
These surgeries are typically done on an outpatient basis, requiring no hospital stay. Recovery time for most of them is several weeks. Recovering from jaw procedures takes longer.
Tracheal shave
A tracheal shave minimizes the thyroid cartilage, also called the Adam's apple. During this procedure, a small cut is made under the chin, in the shadow of the neck or in a skin fold to conceal the scar. The surgeon then reduces and reshapes the cartilage. This is typically an outpatient procedure, requiring no hospital stay.
Top surgery
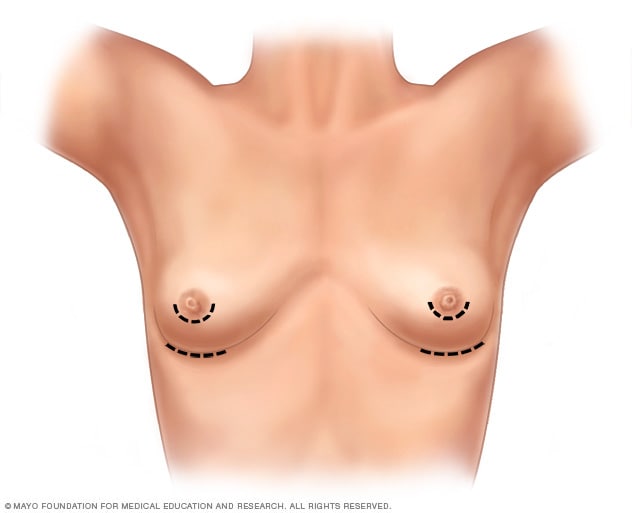
- Breast augmentation incisions
As part of top surgery, the surgeon makes cuts around the areola, near the armpit or in the crease under the breast.
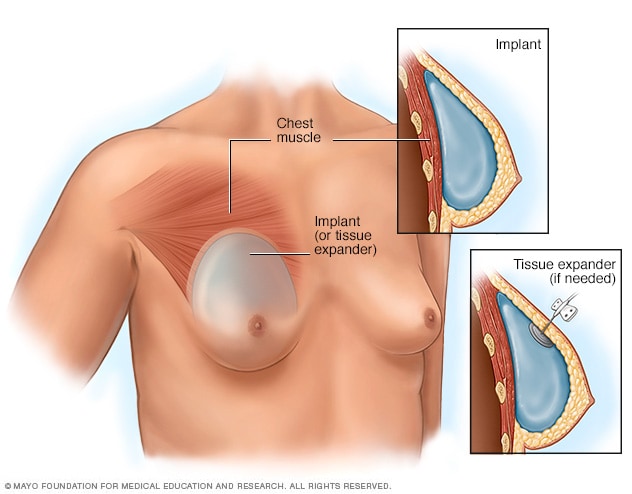
- Placement of breast implants or tissue expanders
During top surgery, the surgeon places the implants under the breast tissue. If feminizing hormones haven't made the breasts large enough, an initial surgery might be needed to have devices called tissue expanders placed in front of the chest muscles.
Hormone therapy with estrogen stimulates breast growth, but many people aren't satisfied with that growth alone. Top surgery is a surgical procedure to increase breast size that may involve implants, fat grafting or both.
During this surgery, a surgeon makes cuts around the areola, near the armpit or in the crease under the breast. Next, silicone or saline implants are placed under the breast tissue. Another option is to transplant fat, muscles or tissue from other parts of the body into the breasts.
If feminizing hormones haven't made the breasts large enough for top surgery, an initial surgery may be needed to place devices called tissue expanders in front of the chest muscles. After that surgery, visits to a health care provider are needed every few weeks to have a small amount of saline injected into the tissue expanders. This slowly stretches the chest skin and other tissues to make room for the implants. When the skin has been stretched enough, another surgery is done to remove the expanders and place the implants.
Genital surgery
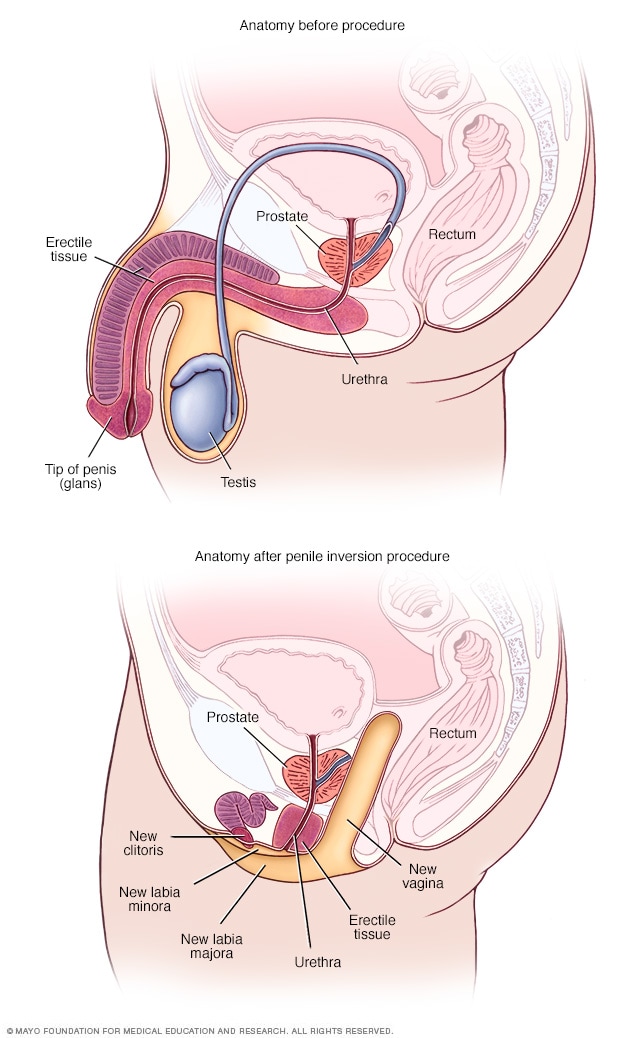
- Anatomy before and after penile inversion
During penile inversion, the surgeon makes a cut in the area between the rectum and the urethra and prostate. This forms a tunnel that becomes the new vagina. The surgeon lines the inside of the tunnel with skin from the scrotum, the penis or both. If there's not enough penile or scrotal skin, the surgeon might take skin from another area of the body and use it for the new vagina as well.
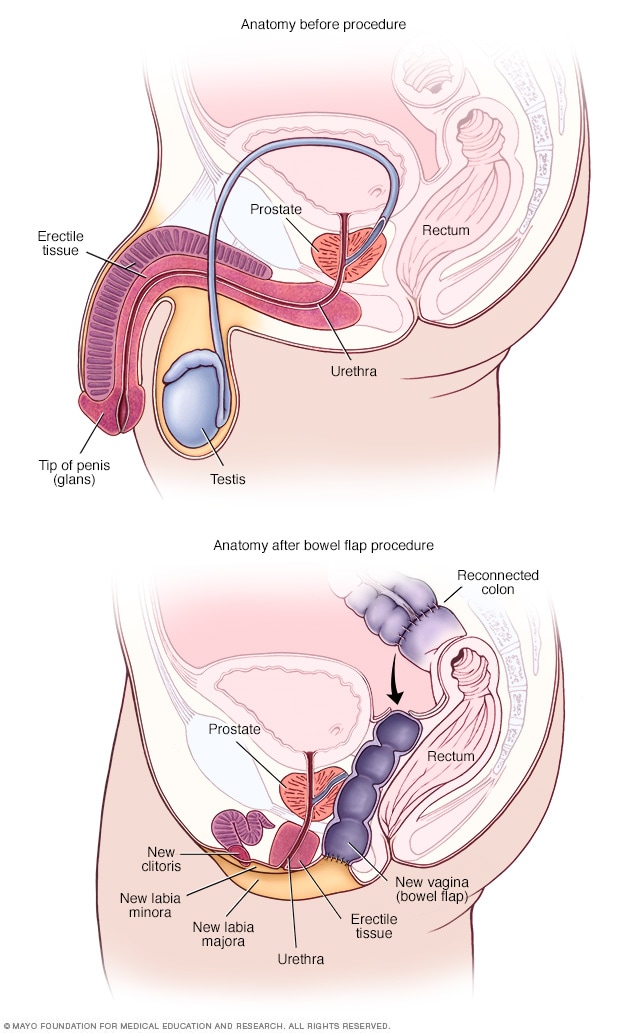
- Anatomy before and after bowel flap procedure
A bowel flap procedure might be done if there's not enough tissue or skin in the penis or scrotum. The surgeon moves a segment of the colon or small bowel to form a new vagina. That segment is called a bowel flap or conduit. The surgeon reconnects the remaining parts of the colon.
Orchiectomy
Orchiectomy is a surgery to remove the testicles. Because testicles produce sperm and the hormone testosterone, an orchiectomy might eliminate the need to use testosterone blockers. It also may lower the amount of estrogen needed to achieve and maintain the appearance you want.
This type of surgery is typically done on an outpatient basis. A local anesthetic may be used, so only the testicular area is numbed. Or the surgery may be done using general anesthesia. This means you are in a sleep-like state during the procedure.
To remove the testicles, a surgeon makes a cut in the scrotum and removes the testicles through the opening. Orchiectomy is typically done as part of the surgery for vaginoplasty. But some people prefer to have it done alone without other genital surgery.
Vaginoplasty
Vaginoplasty is the surgical creation of a vagina. During vaginoplasty, skin from the shaft of the penis and the scrotum is used to create a vaginal canal. This surgical approach is called penile inversion. In some techniques, the skin also is used to create the labia. That procedure is called labiaplasty. To surgically create a clitoris, the tip of the penis and the nerves that supply it are used. This procedure is called a clitoroplasty. In some cases, skin can be taken from another area of the body or tissue from the colon may be used to create the vagina. This approach is called a bowel flap procedure. During vaginoplasty, the testicles are removed if that has not been done previously.
Some surgeons use a technique that requires laser hair removal in the area of the penis and scrotum to provide hair-free tissue for the procedure. That process can take several months. Other techniques don't require hair removal prior to surgery because the hair follicles are destroyed during the procedure.
After vaginoplasty, a tube called a catheter is placed in the urethra to collect urine for several days. You need to be closely watched for about a week after surgery. Recovery can take up to two months. Your health care provider gives you instructions about when you may begin sexual activity with your new vagina.
After surgery, you're given a set of vaginal dilators of increasing sizes. You insert the dilators in your vagina to maintain, lengthen and stretch it. Follow your health care provider's directions on how often to use the dilators. To keep the vagina open, dilation needs to continue long term.
Because the prostate gland isn't removed during surgery, you need to follow age-appropriate recommendations for prostate cancer screening. Following surgery, it is possible to develop urinary symptoms from enlargement of the prostate.
Dilation after gender-affirming surgery
This material is for your education and information only. This content does not replace medical advice, diagnosis and treatment. If you have questions about a medical condition, always talk with your health care provider.
Narrator: Vaginal dilation is important to your recovery and ongoing care. You have to dilate to maintain the size and shape of your vaginal canal and to keep it open.
Jessi: I think for many trans women, including myself, but especially myself, I looked forward to one day having surgery for a long time. So that meant looking up on the internet what the routines would be, what the surgery entailed. So I knew going into it that dilation was going to be a very big part of my routine post-op, but just going forward, permanently.
Narrator: Vaginal dilation is part of your self-care. You will need to do vaginal dilation for the rest of your life.
Alissa (nurse): If you do not do dilation, your vagina may shrink or close. If that happens, these changes might not be able to be reversed.
Narrator: For the first year after surgery, you will dilate many times a day. After the first year, you may only need to dilate once a week. Most people dilate for the rest of their life.
Jessi: The dilation became easier mostly because I healed the scars, the stitches held up a little bit better, and I knew how to do it better. Each transgender woman's vagina is going to be a little bit different based on anatomy, and I grew to learn mine. I understand, you know, what position I needed to put the dilator in, how much force I needed to use, and once I learned how far I needed to put it in and I didn't force it and I didn't worry so much on oh, did I put it in too far, am I not putting it in far enough, and I have all these worries and then I stress out and then my body tenses up. Once I stopped having those thoughts, I relaxed more and it was a lot easier.
Narrator: You will have dilators of different sizes. Your health care provider will determine which sizes are best for you. Dilation will most likely be painful at first. It's important to dilate even if you have pain.
Alissa (nurse): Learning how to relax the muscles and breathe as you dilate will help. If you wish, you can take the pain medication recommended by your health care team before you dilate.
Narrator: Dilation requires time and privacy. Plan ahead so you have a private area at home or at work. Be sure to have your dilators, a mirror, water-based lubricant and towels available. Wash your hands and the dilators with warm soapy water, rinse well and dry on a clean towel. Use a water-based lubricant to moisten the rounded end of the dilators. Water-based lubricants are available over-the-counter. Do not use oil-based lubricants, such as petroleum jelly or baby oil. These can irritate the vagina. Find a comfortable position in bed or elsewhere. Use pillows to support your back and thighs as you lean back to a 45-degree angle. Start your dilation session with the smallest dilator. Hold a mirror in one hand. Use the other hand to find the opening of your vagina. Separate the skin. Relax through your hips, abdomen and pelvic floor. Take slow, deep breaths. Position the rounded end of the dilator with the lubricant at the opening to your vaginal canal. The rounded end should point toward your back. Insert the dilator. Go slowly and gently. Think of its path as a gentle curving swoop. The dilator doesn't go straight in. It follows the natural curve of the vaginal canal. Keep gentle down and inward pressure on the dilator as you insert it. Stop when the dilator's rounded end reaches the end of your vaginal canal. The dilators have dots or markers that measure depth. Hold the dilator in place in your vaginal canal. Use gentle but constant inward pressure for the correct amount of time at the right depth for you. If you're feeling pain, breathe and relax the muscles. When time is up, slowly remove the dilator, then repeat with the other dilators you need to use. Wash the dilators and your hands. If you have increased discharge following dilation, you may want to wear a pad to protect your clothing.
Jessi: I mean, it's such a strange, unfamiliar feeling to dilate and to have a dilator, you know to insert a dilator into your own vagina. Because it's not a pleasurable experience, and it's quite painful at first when you start to dilate. It feels much like a foreign body entering and it doesn't feel familiar and your body kind of wants to get it out of there. It's really tough at the beginning, but if you can get through the first month, couple months, it's going to be a lot easier and it's not going to be so much of an emotional and uncomfortable experience.
Narrator: You need to stay on schedule even when traveling. Bring your dilators with you. If your schedule at work creates challenges, ask your health care team if some of your dilation sessions can be done overnight.
Alissa (nurse): You can't skip days now and do more dilation later. You must do dilation on schedule to keep vaginal depth and width. It is important to dilate even if you have pain. Dilation should cause less pain over time.
Jessi: I hear that from a lot of other women that it's an overwhelming experience. There's lots of emotions that are coming through all at once. But at the end of the day for me, it was a very happy experience. I was glad to have the opportunity because that meant that while I have a vagina now, at the end of the day I had a vagina. Yes, it hurts, and it's not pleasant to dilate, but I have the vagina and it's worth it. It's a long process and it's not going to be easy. But you can do it.
Narrator: If you feel dilation may not be working or you have any questions about dilation, please talk with a member of your health care team.
Research has found that gender-affirming surgery can have a positive impact on well-being and sexual function. It's important to follow your health care provider's advice for long-term care and follow-up after surgery. Continued care after surgery is associated with good outcomes for long-term health.
Before you have surgery, talk to members of your health care team about what to expect after surgery and the ongoing care you may need.
Clinical trials
Explore Mayo Clinic studies of tests and procedures to help prevent, detect, treat or manage conditions.
Feminizing surgery care at Mayo Clinic
- Tangpricha V, et al. Transgender women: Evaluation and management. https://www.uptodate.com/ contents/search. Accessed Aug. 16, 2022.
- Erickson-Schroth L, ed. Surgical transition. In: Trans Bodies, Trans Selves: A Resource by and for Transgender Communities. 2nd ed. Kindle edition. Oxford University Press; 2022. Accessed Aug. 17, 2022.
- Coleman E, et al. Standards of care for the health of transgender and gender diverse people, version 8. International Journal of Transgender Health. 2022; doi:10.1080/26895269.2022.2100644.
- AskMayoExpert. Gender-affirming procedures (adult). Mayo Clinic; 2022.
- Nahabedian, M. Implant-based breast reconstruction and augmentation. https://www.uptodate.com/contents/search. Accessed Aug. 17, 2022.
- Erickson-Schroth L, ed. Medical transition. In: Trans Bodies, Trans Selves: A Resource by and for Transgender Communities. 2nd ed. Kindle edition. Oxford University Press; 2022. Accessed Aug. 17, 2022.
- Ferrando C, et al. Gender-affirming surgery: Male to female. https://www.uptodate.com/contents/search. Accessed Aug. 17, 2022.
- Doctors & Departments
- Care at Mayo Clinic
Mayo Clinic does not endorse companies or products. Advertising revenue supports our not-for-profit mission.
- Opportunities
Mayo Clinic Press
Check out these best-sellers and special offers on books and newsletters from Mayo Clinic Press .
- Mayo Clinic on Incontinence - Mayo Clinic Press Mayo Clinic on Incontinence
- The Essential Diabetes Book - Mayo Clinic Press The Essential Diabetes Book
- Mayo Clinic on Hearing and Balance - Mayo Clinic Press Mayo Clinic on Hearing and Balance
- FREE Mayo Clinic Diet Assessment - Mayo Clinic Press FREE Mayo Clinic Diet Assessment
- Mayo Clinic Health Letter - FREE book - Mayo Clinic Press Mayo Clinic Health Letter - FREE book
5X Challenge
Thanks to generous benefactors, your gift today can have 5X the impact to advance AI innovation at Mayo Clinic.
Information
- Author Services
Initiatives
You are accessing a machine-readable page. In order to be human-readable, please install an RSS reader.
All articles published by MDPI are made immediately available worldwide under an open access license. No special permission is required to reuse all or part of the article published by MDPI, including figures and tables. For articles published under an open access Creative Common CC BY license, any part of the article may be reused without permission provided that the original article is clearly cited. For more information, please refer to https://www.mdpi.com/openaccess .
Feature papers represent the most advanced research with significant potential for high impact in the field. A Feature Paper should be a substantial original Article that involves several techniques or approaches, provides an outlook for future research directions and describes possible research applications.
Feature papers are submitted upon individual invitation or recommendation by the scientific editors and must receive positive feedback from the reviewers.
Editor’s Choice articles are based on recommendations by the scientific editors of MDPI journals from around the world. Editors select a small number of articles recently published in the journal that they believe will be particularly interesting to readers, or important in the respective research area. The aim is to provide a snapshot of some of the most exciting work published in the various research areas of the journal.
Original Submission Date Received: .
- Active Journals
- Find a Journal
- Proceedings Series
- For Authors
- For Reviewers
- For Editors
- For Librarians
- For Publishers
- For Societies
- For Conference Organizers
- Open Access Policy
- Institutional Open Access Program
- Special Issues Guidelines
- Editorial Process
- Research and Publication Ethics
- Article Processing Charges
- Testimonials
- Preprints.org
- SciProfiles
- Encyclopedia

Article Menu

- Subscribe SciFeed
- Recommended Articles
- Google Scholar
- on Google Scholar
- Table of Contents
Find support for a specific problem in the support section of our website.
Please let us know what you think of our products and services.
Visit our dedicated information section to learn more about MDPI.
JSmol Viewer
Gender reassignment and the role of the laboratory in monitoring gender-affirming hormone therapy.

1. Introduction
3. gender development, genesis of gender incongruence, 4. guidelines for gaht, 4.1. adolescent gi, 4.2. adult gi, 5. laboratory tests in transgender afab/amab individuals, 5.1. red blood cell indices, 5.2. renal function, 5.3. liver enzymes, 5.4. lipids, 5.5. cardiac biomarkers, 5.6. reproductive hormones, 5.7. ferritin, 5.8. prostate specific antigen.
| Laboratory Tests | Comments | Reference | ||
|---|---|---|---|---|
| Estradiol treatment | Testosterone treatment | Estradiol GAHT shifts haemoglobin, haematocrit to lower values in line with cisgender women’s reference intervals. Testosterone GAHTshifts reference intervals to higher levels in line with cisgender men’s reference intervals | [ ] | |
| RBC | Decrease | Increase | ||
| Hemoglobin | Decrease | Increase | ||
| Hematocrit | Decrease | Increase | ||
| Creatinine | Decrease | Increase | The most reno protective calculated GFR either male/female is suggested; 24h creatinine clearance if indicated | [ ] |
| High sensitivity troponin I | Report a reference range that would allow critical results to be appropriately followed; an approach of least harm to the patient is suggested | [ ] | ||
| Ferritin | Laboratories use dual reference ranges for cisgender individuals. Interpretation is based on clinical presentation (e.g., pregnancy) in combination with full blood count, liver function test, and markers of inflammation, e.g., CRP. Iron overload: If secondary causes excluded, investigation for primary haemochromatosis gene may be indicated | [ ] | ||
| Reproductive hormones | Testosterone, Estradiol | Following stabilisation of treatment with gender-affirming hormones, guidelines suggest treatment goals are physiological levels of the affirmed gender identity cisgender adults. The time of measurement of the hormone is dependent on the method of administration as well as formulation of the GAHT | [ ] | |
| Reproductive hormones | LH, FSH, AMH, and DHEAS are variable in a transgender population and are interpreted with clinical information | [ , ] | ||
| PSA | Data for reference ranges in transgender AMAB people and from screening for prostatic cancer is not available | [ ] | ||
| Renal function/liver function/lipid profile | Guidelines suggest monitoring of liver function/renal function and lipids during GAHT treatment. Sex-specific reference ranges are not ordinarily stated for the measurements | [ ] |
5.9. Laboratory Test Reference Intervals for Transgender Population
6. electronic medical record systems (emr), 7. gaht and other laboratory markers, 7.1. risk of venous thromboembolism in amab people, 7.2. hyperprolactinemia, 7.3. other sex hormone dependent tumours, 7.4. bone mineral density, 8. gaht, vascular health and cardiovascular disease, and impact of aging in transgender adults, 9. conclusions, 10. future directions, conflicts of interest.
- Glintborg, D.; T’Sjoen, G.; Ravn, P.; Andersen, M.S. Management of endocrine disease: Optimal feminizing hormone treatment in transgender people. Eur. J. Endocrinol. 2021 , 185 , R49–R63. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Hembree, W.C.; Cohen-Kettenis, P.T.; Gooren, L.; Hannema, S.E.; Meyer, W.J.; Murad, M.H.; Rosenthal, S.M.; Safer, J.D.; Tangpricha, V.; T’Sjoen, G.G. Endocrine Treatment of Gender-Dysphoric/Gender-Incongruent Persons: An Endocrine Society Clinical Practice Guideline. J. Clin. Endocrinol. Metab. 2017 , 102 , 3869–3903, Erratum in J. Clin. Endocrinol. Metab. 2018 , 103 , 699. Erratum in J. Clin. Endocrinol. Metab. 2018 , 103 , 2758–2759. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Coleman, E.; Radix, A.E.; Bouman, W.P.; Brown, G.R.; de Vries, A.L.C.; Deutsch, M.B.; Ettner, R.; Fraser, L.; Goodman, M.; Green, J.; et al. Standards of Care for the Health of Transgender and Gender Diverse People, Version 8. Int. J. Transgender Health. 2022 , 23 (Suppl. 1), S1–S259. [ Google Scholar ] [ CrossRef ] [ PubMed ] [ PubMed Central ]
- Available online: https://auspath.org.au/wp-content/uploads/2022/05/AusPATH_Informed-Consent-Guidelines_DIGITAL.pdf (accessed on 2 June 2024).
- Cheung, A.S.; Wynne, K.; Erasmus, J.; Murray, S.; Zajac, J.D. Position statement on the hormonal management of adult transgender and gender diverse individuals. Med. J. Aust. 2019 , 211 , 127–133. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Beek, F.T.; Cohen-Kettenis, P.T.; Kreukels, B.P.C. Gender incongruence/gender dysphoria and its classification history. Int. Rev. Psychiatry 2016 , 28 , 5–12. [ Google Scholar ] [ CrossRef ]
- Reyes, A.P.; León, N.Y.; Frost, E.R.; Harley, V.R. Genetic control of typical and atypical sex development. Nat. Rev. Urol. 2023 , 20 , 434–451. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Richardson, B.E.; Lehmann, R. Mechanisms guiding primordial germ cell migration: Strategies from different organisms. Nat. Rev. Mol. Cell Biol. 2010 , 11 , 37–49. [ Google Scholar ] [ CrossRef ] [ PubMed ] [ PubMed Central ]
- Ostrer, H.; Huang, H.Y.; Masch, R.J.; Shapiro, E. A cellular study of human testis development. Sex. Dev. 2007 , 1 , 286–292. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- She, Z.Y.; Yang, W.X. Sry and SoxE genes: How they participate in mammalian sex determination and gonadal development? Semin. Cell Dev. Biol. 2017 , 63 , 13–22. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Edelsztein, N.Y.; Valeri, C.; Lovaisa, M.M.; Schteingart, H.F.; Rey, R.A. AMH Regulation by Steroids in the Mammalian Testis: Underlying Mechanisms and Clinical Implications. Front. Endocrinol. 2022 , 13 , 906381. [ Google Scholar ] [ CrossRef ] [ PubMed ] [ PubMed Central ]
- Rey, R.A.; Grinspon, R.P. Normal male sexual differentiation and aetiology of disorders of sex development. Best. Pract. Res. Clin. Endocrinol. Metab. 2011 , 25 , 221–238. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Emmanuel, M.; Bokor, B.R. Tanner Stages. [Updated 11 December 2022]. In StatPearls [Internet] ; StatPearls Publishing: Treasure Island, FL, USA, 2024. Available online: https://www.ncbi.nlm.nih.gov/books/NBK470280/ (accessed on 25 August 2024).
- Eliot, L.; Ahmed, A.; Khan, H.; Patel, J. Dump the “dimorphism”: Comprehensive synthesis of human brain studies reveals few male-female differences beyond size. Neurosci. Biobehav. Rev. 2021 , 125 , 667–697. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Ruigrok, A.N.; Salimi-Khorshidi, G.; Lai, M.C.; Baron-Cohen, S.; Lombardo, M.V.; Tait, R.J.; Suckling, J. A meta-analysis of sex differences in human brain structure. Neurosci. Biobehav. Rev. 2014 , 39 , 34–50. [ Google Scholar ] [ CrossRef ] [ PubMed ] [ PubMed Central ]
- Lafta, M.S.; Mwinyi, J.; Affatato, O.; Rukh, G.; Dang, J.; Andersson, G.; Schiöth, H.B. Exploring sex differences: Insights into gene expression, neuroanatomy, neurochemistry, cognition, and pathology. Front. Neurosci. 2024 , 18 , 1340108. [ Google Scholar ] [ CrossRef ] [ PubMed ] [ PubMed Central ]
- Fine, R.D.; Olson, K.R.; Gülgöz, S.; Horton, R.; Gelman, S.A. Gender Essentialism Predicts Prejudice against Gender Nonconformity in Two Cultural Contexts. Soc. Dev. 2024 , 33 , e12720. [ Google Scholar ] [ CrossRef ] [ PubMed ] [ PubMed Central ]
- Mueller, S.C.; Guillamon, A.; Zubiaurre-Elorza, L.; Junque, C.; Gomez-Gil, E.; Uribe, C.; Khorashad, B.S.; Khazai, B.; Talaei, A.; Habel, U.; et al. The Neuroanatomy of Transgender Identity: Mega-Analytic Findings From the ENIGMA Transgender Persons Working Group. J. Sex. Med. 2021 , 18 , 1122–1129. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Saraswat, A.; Weinand, J.D.; Safer, J.D. Evidence supporting the biologic nature of gender identity. Endocr. Pract. 2015 , 21 , 199–204. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Foreman, M.; Hare, L.; York, K.; Balakrishnan, K.; Sánchez, F.J.; Harte, F.; Erasmus, J.; Vilain, E.; Harley, V.R. Genetic Link Between Gender Dysphoria and Sex Hormone Signaling. J. Clin. Endocrinol. Metab. 2019 , 104 , 390–396, Erratum in J. Clin. Endocrinol. Metab. 2020 , 105 , 393. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Fernández, R.; Guillamon, A.; Cortés-Cortés, J.; Gómez-Gil, E.; Jácome, A.; Esteva, I.; Almaraz, M.; Mora, M.; Aranda, G.; Pásaro, E. Molecular basis of Gender Dysphoria: Androgen and estrogen receptor interaction. Psychoneuroendocrinology 2018 , 98 , 161–167. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Steensma, T.D.; Kreukels, B.P.; de Vries, A.L.; Cohen-Kettenis, P.T. Gender identity development in adolescence. Horm. Behav. 2013 , 64 , 288–297. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Zhang, Q.; Goodman, M.; Adams, N.; Corneil, T.; Hashemi, L.; Kreukels, B.; Motmans, J.; Snyder, R.; Coleman, E. Epidemiological considerations in transgender health: A systematic review with focus on higher quality data. Int. J. Transgender Health. 2020 , 21 , 125–137. [ Google Scholar ] [ CrossRef ] [ PubMed ] [ PubMed Central ]
- Brierley, J.; Larcher, V.; Hadjipanayis, A.A.; Grossman, Z. European Academy of Paediatrics statement on the clinical management of children and adolescents with gender dysphoria. Front. Pediatr. 2024 , 12 , 1298884. [ Google Scholar ] [ CrossRef ] [ PubMed ] [ PubMed Central ]
- Claahsen-van der Grinten, H.; Verhaak, C.; Steensma, T.; Middelberg, T.; Roeffen, J.; Klink, D. Gender incongruence and gender dysphoria in childhood and adolescence-current insights in diagnostics, management, and follow-up. Eur. J. Pediatr. 2021 , 180 , 1349–1357. [ Google Scholar ] [ CrossRef ] [ PubMed ] [ PubMed Central ]
- Brik, T.; Vrouenraets, L.J.J.J.; de Vries, M.C.; Hannema, S.E. Trajectories of Adolescents Treated with Gonadotropin-Releasing Hormone Analogues for Gender Dysphoria. Arch. Sex. Behav. 2020 , 49 , 2611–2618. [ Google Scholar ] [ CrossRef ] [ PubMed ] [ PubMed Central ]
- Steininger, J.; Knaus, S.; Kaufmann, U.; Ott, J.; Riedl, S. Treatment trajectories of gender incongruent Austrian youth seeking gender-affirming hormone therapy. Front. Endocrinol. 2024 , 15 , 1258495. [ Google Scholar ] [ CrossRef ] [ PubMed ] [ PubMed Central ]
- Panagiotakopoulos, L. Transgender medicine—Puberty suppression. Rev. Endocr. Metab. Disord. 2018 , 19 , 221–225. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Halasz, G.; Amos, A. Gender dysphoria: Reconsidering ethical and iatrogenic factors in clinical practice. Australas. Psychiatry 2024 , 32 , 26–31. [ Google Scholar ] [ CrossRef ] [ PubMed ] [ PubMed Central ]
- Calcaterra, V.; Tornese, G.; Zuccotti, G.; Staiano, A.; Cherubini, V.; Gaudino, R.; Fazzi, E.M.; Barbi, E.; Chiarelli, F.; Corsello, G.; et al. Adolescent gender dysphoria management: Position paper from the Italian Academy of Pediatrics, the Italian Society of Pediatrics, the Italian Society for Pediatric Endocrinology and Diabetes, the Italian Society of Adolescent Medicine and the Italian Society of Child and Adolescent Neuropsychiatry. Ital. J. Pediatr. 2024 , 50 , 73. [ Google Scholar ] [ CrossRef ] [ PubMed ] [ PubMed Central ]
- Dahlen, S.; Connolly, D.; Arif, I.; Junejo, M.H.; Bewley, S.; Meads, C. International clinical practice guidelines for gender minority/trans people: Systematic review and quality assessment. BMJ Open 2021 , 11 , e048943. [ Google Scholar ] [ CrossRef ]
- Humble, R.M.; Imborek, K.L.; Nisly, N.; Greene, D.N.; Krasowski, M.D. Common Hormone Therapies Used to Care for Transgender Patients Influence Laboratory Results. J. Appl. Lab. Med. 2019 , 3 , 799–814. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- SoRelle, J.A.; Jiao, R.; Gao, E.; Veazey, J.; Frame, I.; Quinn, A.M.; Day, P.; Pagels, P.; Gimpel, N.; Patel, K. Impact of Hormone Therapy on Laboratory Values in Transgender Patients. Clin. Chem. 2019 , 65 , 170–179. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Allen, A.N.; Jiao, R.; Day, P.; Pagels, P.; Gimpel, N.; SoRelle, J.A. Dynamic Impact of Hormone Therapy on Laboratory Values in Transgender Patients over Time. J. Appl. Lab. Med. 2021 , 6 , 27–40. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Millington, K.; Lee, J.Y.; Olson-Kennedy, J.; Garofalo, R.; Rosenthal, S.M.; Chan, Y.M. Laboratory Changes During Gender-Affirming Hormone Therapy in Transgender Adolescents. Pediatrics 2024 , 153 , e2023064380. [ Google Scholar ] [ CrossRef ] [ PubMed ] [ PubMed Central ]
- Murphy, W.G. The sex difference in haemoglobin levels in adults—Mechanisms, causes, and consequences. Blood Rev. 2014 , 28 , 41–47. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Greene, D.N.; McPherson, G.W.; Rongitsch, J.; Imborek, K.L.; Schmidt, R.L.; Humble, R.M.; Nisly, N.; Dole, N.J.; Dane, S.K.; Frerichs, J.; et al. Hematology reference intervals for transgender adults on stable hormone therapy. Clin. Chim. Acta. 2019 , 492 , 84–90. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Humble, R.M.; Greene, D.N.; Schmidt, R.L.; Winston McPherson, G.; Rongitsch, J.; Imborek, K.L.; Nisly, N.; Dole, N.J.; Dane, S.K.; Frerichs, J.; et al. Reference Intervals for Clinical Chemistry Analytes for Transgender Men and Women on Stable Hormone Therapy. J. Appl. Lab. Med. 2022 , 7 , 1131–1144. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Hashemi, L.; Zhang, Q.; Getahun, D.; Jasuja, G.K.; McCracken, C.; Pisegna, J.; Roblin, D.; Silverberg, M.J.; Tangpricha, V.; Vupputuri, S.; et al. Longitudinal Changes in Liver Enzyme Levels Among Transgender People Receiving Gender Affirming Hormone Therapy. J. Sex. Med. 2021 , 18 , 1662–1675. [ Google Scholar ] [ CrossRef ] [ PubMed ] [ PubMed Central ]
- Krasowski, M.D.; Hines, N.G.; Imborek, K.L.; Greene, D.N. Impact of sex used for assignment of reference intervals in a population of patients taking gender-affirming hormones. J. Clin. Transl. Endocrinol. 2024 , 36 , 100350. [ Google Scholar ] [ CrossRef ] [ PubMed ] [ PubMed Central ]
- Wierckx, K.; Van Caenegem, E.; Schreiner, T.; Haraldsen, I.; Fisher, A.D.; Toye, K.; Kaufman, J.M.; T’Sjoen, G. Cross-sex hormone therapy in trans persons is safe and effective at short-time follow-up: Results from the European network for the investigation of gender incongruence. J. Sex. Med. 2014 , 11 , 1999–2011. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Deutsch, M.B.; Bhakri, V.; Kubicek, K. Effects of cross-sex hormone treatment on transgender women and men. Obstet. Gynecol. 2015 , 125 , 605–610. [ Google Scholar ] [ CrossRef ] [ PubMed ] [ PubMed Central ]
- Fernandez, J.D.; Tannock, L.R. Metabolic effects of hormone therapy in transgender patients. Endocr. Pract. 2016 , 22 , 383–388. [ Google Scholar ] [ CrossRef ] [ PubMed ] [ PubMed Central ]
- Waters, J.; Linsenmeyer, W. The impact of gender-affirming hormone therapy on nutrition-relevant biochemical measures. Front. Nutr. 2024 , 11 , 1339311. [ Google Scholar ] [ CrossRef ] [ PubMed ] [ PubMed Central ]
- Greene, D.N.; Schmidt, R.L.; Christenson, R.H.; Rongitsch, J.; Imborek, K.L.; Rebuck, H.; Lorey, T.S.; Saenger, A.K.; Krasowski, M.D. Distribution of High-Sensitivity Cardiac Troponin and N-Terminal Pro-Brain Natriuretic Peptide in Healthy Transgender People. JAMA Cardiol. 2022 , 7 , 1170–1174. [ Google Scholar ] [ CrossRef ] [ PubMed ] [ PubMed Central ]
- Wang, J.; Taur, A.; Chen, A.; Wu, Y.L.; Lee, M.S. Sex-Specific Cardiac Troponin Thresholds in Transgender Patients With Suspected Acute Coronary Syndrome. JAMA Netw. Open. 2023 , 6 , e2337345. [ Google Scholar ] [ CrossRef ] [ PubMed ] [ PubMed Central ]
- Greene, D.N.; Schmidt, R.L.; Winston McPherson, G.; Rongitsch, J.; Imborek, K.L.; Dickerson, J.A.; Drees, J.C.; Humble, R.M.; Nisly, N.; Dole, N.J.; et al. Reproductive Endocrinology Reference Intervals for Transgender Women on Stable Hormone Therapy. J. Appl. Lab. Med. 2021 , 6 , 15–26. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Greene, D.N.; Schmidt, R.L.; Winston-McPherson, G.; Rongitsch, J.; Imborek, K.L.; Dickerson, J.A.; Drees, J.C.; Humble, R.M.; Nisly, N.; Dole, N.J.; et al. Reproductive Endocrinology Reference Intervals for Transgender Men on Stable Hormone Therapy. J. Appl. Lab. Med. 2021 , 6 , 41–50. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- McKinnon, E.J.; Rossi, E.; Beilby, J.P.; Trinder, D.; Olynyk, J.K. Factors that affect serum levels of ferritin in Australian adults and implications for follow-up. Clin. Gastroenterol. Hepatol. 2014 , 12 , 101–108.e4. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- de Nie, I.; de Blok, C.J.M.; van der Sluis, T.M.; Barbé, E.; Pigot, G.L.S.; Wiepjes, C.M.; Nota, N.M.; van Mello, N.M.; Valkenburg, N.E.; Huirne, J.; et al. Prostate Cancer Incidence under Androgen Deprivation: Nationwide Cohort Study in Trans Women Receiving Hormone Treatment. J. Clin. Endocrinol. Metab. 2020 , 105 , e3293–e3299. [ Google Scholar ] [ CrossRef ] [ PubMed ] [ PubMed Central ]
- Loria, M.; Gilbert, D.; Tabernacki, T.; Maravillas, M.A.; McNamara, M.; Gupta, S.; Mishra, K. Incidence of prostate cancer in transgender women in the US: A large database analysis. Prostate Cancer Prostatic Dis. 2024; Epub ahead of print . [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Crowley, F.; Mihalopoulos, M.; Gaglani, S.; Tewari, A.K.; Tsao, C.K.; Djordjevic, M.; Kyprianou, N.; Purohit, R.S.; Lundon, D.J. Prostate cancer in transgender women: Considerations for screening, diagnosis and management. Br. J. Cancer. 2023 , 128 , 177–189. [ Google Scholar ] [ CrossRef ] [ PubMed ] [ PubMed Central ]
- Irwig, M.S. Which reference range should we use for transgender and gender diverse patients? J. Clin. Endocrinol. Metab. 2021 , 106 , e1479–e1480. [ Google Scholar ] [ CrossRef ] [ PubMed ] [ PubMed Central ]
- Cheung, A.S.; Lim, H.Y.; Cook, T.; Zwickl, S.; Ginger, A.; Chiang, C.; Zajac, J.D. Approach to Interpreting Common Laboratory Pathology Tests in Transgender Individuals. J. Clin. Endocrinol. Metab. 2021 , 106 , 893–901. [ Google Scholar ] [ CrossRef ] [ PubMed ] [ PubMed Central ]
- Cahill, S.R.; Baker, K.; Deutsch, M.B.; Keatley, J.; Makadon, H.J. Inclusion of Sexual Orientation and Gender Identity in Stage 3 Meaningful Use Guidelines: A Huge Step Forward for LGBT Health. LGBT Health 2016 , 3 , 100–102. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Patel, K.; Lyon, M.E.; Luu, H.S. Providing Inclusive Care for Transgender Patients: Capturing Sex and Gender in the Electronic Medical Record. J. Appl. Lab. Med. 2021 , 6 , 210–218. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Totaro, M.; Palazzi, S.; Castellini, C.; Parisi, A.; D’Amato, F.; Tienforti, D.; Baroni, M.G.; Francavilla, S.; Barbonetti, A. Risk of Venous Thromboembolism in Transgender People Undergoing Hormone Feminizing Therapy: A Prevalence Meta-Analysis and Meta-Regression Study. Front. Endocrinol. 2021 , 12 , 741866. [ Google Scholar ] [ CrossRef ] [ PubMed ] [ PubMed Central ]
- Ott, J.; Kaufmann, U.; Bentz, E.K.; Huber, J.C.; Tempfer, C.B. Incidence of thrombophilia and venous thrombosis in transsexuals under cross-sex hormone therapy. Fertil. Steril. 2010 , 93 , 1267–1272. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Dix, C.; Moloney, M.; Tran, H.A.; McFadyen, J.D. Venous Thromboembolism and Estrogen-Containing Gender-Affirming Hormone Therapy. Thromb. Haemost. 2024 , 124 , 387–398. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Wilson, L.M.; Baker, K.E.; Sharma, R.; Dukhanin, V.; McArthur, K.; Robinson, K.A. Effects of antiandrogens on prolactin levels among transgender women on estrogen therapy: A systematic review. Int. J. Transgender Health 2020 , 21 , 391–402. [ Google Scholar ] [ CrossRef ] [ PubMed ] [ PubMed Central ]
- Wahlström, E.; Audisio, R.A.; Selvaggi, G. Aspects to consider regarding breast cancer risk in trans men: A systematic review and risk management approach. PLoS ONE 2024 , 19 , e0299333. [ Google Scholar ] [ CrossRef ] [ PubMed ] [ PubMed Central ]
- Pamulapati, S.; Conroy, M.; Cortina, C.; Harding, E.; Kamaraju, S. Systematic Review on Gender-Affirming Testosterone Therapy and the Risk of Breast Cancer: A Challenge for Physicians Treating Patients from Transgender and Gender-Diverse Populations. Arch. Sex. Behav. 2024 , 53 , 1969–1980. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Schagen, S.E.E.; Wouters, F.M.; Cohen-Kettenis, P.T.; Gooren, L.J.; Hannema, S.E. Bone Development in Transgender Adolescents Treated With GnRH Analogues and Subsequent Gender-Affirming Hormones. J. Clin. Endocrinol. Metab. 2020 , 105 , e4252–e4263. [ Google Scholar ] [ CrossRef ] [ PubMed ] [ PubMed Central ]
- Verroken, C.; Collet, S.; Lapauw, B.; T’Sjoen, G. Osteoporosis and Bone Health in Transgender Individuals. Calcif. Tissue Int. 2022 , 110 , 615–623. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Venkatesh, V.S.; Nie, T.; Zajac, J.D.; Grossmann, M.; Davey, R.A. The Utility of Preclinical Models in Understanding the Bone Health of Transgender Individuals Undergoing Gender-Affirming Hormone Therapy. Curr. Osteoporos. Rep. 2023 , 21 , 825–841. [ Google Scholar ] [ CrossRef ] [ PubMed ] [ PubMed Central ]
- Rothman, M.S.; Iwamoto, S.J. Bone Health in the Transgender Population. Clin. Rev. Bone Miner. Metab. 2019 , 17 , 77–85. [ Google Scholar ] [ CrossRef ] [ PubMed ] [ PubMed Central ]
- Rosen, H.N.; Hamnvik, O.R.; Jaisamrarn, U.; Malabanan, A.O.; Safer, J.D.; Tangpricha, V.; Wattanachanya, L.; Yeap, S.S. Bone Densitometry in Transgender and Gender Non-Conforming (TGNC) Individuals: 2019 ISCD Official Position. J. Clin. Densitom. 2019 , 22 , 544–553. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Shuhart, C.R.; Yeap, S.S.; Anderson, P.A.; Jankowski, L.G.; Lewiecki, E.M.; Morse, L.R.; Rosen, H.N.; Weber, D.R.; Zemel, B.S.; Shepherd, J.A. Executive Summary of the 2019 ISCD Position Development Conference on Monitoring Treatment, DXA Cross-calibration and Least Significant Change, Spinal Cord Injury, Peri-prosthetic and Orthopedic Bone Health, Transgender Medicine, and Pediatrics. J. Clin. Densitom. 2019 , 22 , 453–471. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- van Leerdam, T.R.; Zajac, J.D.; Cheung, A.S. The Effect of Gender-Affirming Hormones on Gender Dysphoria, Quality of Life, and Psychological Functioning in Transgender Individuals: A Systematic Review. Transgender Health 2023 , 8 , 6–21. [ Google Scholar ] [ CrossRef ] [ PubMed ] [ PubMed Central ]
- Bouck, E.G.; Grinsztejn, E.; Mcnamara, M.; Stavrou, E.X.; Wolberg, A.S. Thromboembolic risk with gender-affirming hormone therapy: Potential role of global coagulation and fibrinolysis assays. Res. Pract. Thromb. Haemost. 2023 , 7 , 102197. [ Google Scholar ] [ CrossRef ] [ PubMed ] [ PubMed Central ]
- Aranda, G.; Halperin, I.; Gomez-Gil, E.; Hanzu, F.A.; Seguí, N.; Guillamon, A.; Mora, M. Cardiovascular Risk Associated With Gender Affirming Hormone Therapy in Transgender Population. Front. Endocrinol. 2021 , 12 , 718200. [ Google Scholar ] [ CrossRef ] [ PubMed ] [ PubMed Central ]
- Cheung, A.S.; Nolan, B.J.; Zwickl, S. Transgender health and the impact of aging and menopause. Climacteric 2023 , 26 , 256–262. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Lucas-Herald, A.K.; Bashamboo, A. Gonadal development. Endocr. Dev. 2014 , 27 , 1–16. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Available online: https://www.socialstyrelsen.se/globalassets/sharepoint-dokument/artikelkatalog/kunskapsstod/2023-1-8330.pdf (accessed on 2 July 2024).
Click here to enlarge figure
| Tanner Stage | Pubic Hair (Male and Female) | Breast Development (Females) | Testicular Volume (Males) |
|---|---|---|---|
| 1 | No hair | No glandular breast tissue palpable | Testicular volume < 4 mL or long axis < 2.5 cm |
| 2 | Downy hair | Breast bud palpable under the areola (1st pubertal sign in females) | 4–8 mL (or 2.5 to 3.3 cm long), 1st pubertal sign in males |
| 3 | Scant terminal hair | Breast tissue palpable outside areola; no areolar development | 9–12 mL (or 3.4 to 4.0 cm long) |
| 4 | Terminal hair that fills the entire triangle overlying the pubic region | Areola elevated above the contour of the breast, forming a “double scoop” appearance | 15–20 mL (or 4.1 to 4.5 cm long) |
| 5 | Terminal hair that extends beyond the inguinal crease onto the thigh | Areolar mound recedes into single breast contour with areolar hyperpigmentation, papillae development, and nipple protrusion | >20 mL (or >4.5 cm long) |
| Guidelines | Society of Endocrinology | The World Professional Association for Transgender Health (WPATH) | Australian Professional Association for Trans Health (AusPATH) |
|---|---|---|---|
| Evaluation of prospective patients | Clinicians can add gender-affirming hormones after multidisciplinary team (MDT) team has confirmed the persistence of GI and sufficient mental capacity to give informed consent to treatment. The clinicians and mental health practitioners must be trained to diagnose GI. | Health care professionals have competencies in the assessment of transgender and gender diverse people wishing gender-related medical treatment and consider the role of social transition together with the individual. Liaise with professionals from different disciplines within the field of transgender health prior to gender-affirming treatment | |
| Treatment | Unless there is agreement among the parents, the adolescent, and medical practitioner regarding competence, diagnosis, and treatment, a Family Court order is required for access to gender-affirming puberty blockers, hormone treatment, and surgery for adolescents under 18 years old. | ||
| Puberty Induction Regimen | Transgender AMAB people: Increasing doses of oral or transdermal 17β-estradiol, until adult dosage is reached. In postpubertal transgender AMAB people, the dose is increased more rapidly. Transgender AFAB people: Increasing doses of testosterone until adult values are reached. In postpubertal males, the dose is increased more rapidly. Adult maintenance dose is to mimic physiological adult levels. | In eligible youth who have reached the early stages of puberty, the aim is to delay further pubertal progression with GnRHas until an appropriate time when GAHT can be introduced. In these cases, pubertal suppression is considered medically necessary. | |
| Treatment of transgender AFAB/AMAB people | Transgender AFAB people: treatment with both parenteral and transdermal testosterone Transgender AMAB people: Oral, transdermal or parenteral oestrogen. Antiandrogens: spironolactone, cyproterone acetate, GnRH agonist. Estradiol and testosterone are maintained at premenopausal female levels. Gender-affirming hormones are maintained at normal adult ranges | Transgender AFAB people: Masculinising treatment, usually with testosterone. Transgender AMAB people: treatment is usually with oestrogen and androgen-lowering medication. | Transgender AFAB people: masculinising treatment is with different formulations of testosterone Transgender AMAB people: Feminising treatment includes oestrogen and androgen blockers. It is usual to start with low doses and titrate upwards. |
| Monitoring | Periodic monitoring of hormone levels, metabolic parameters, and assessment of prostate gland, gonads, and uterus as well as bone density | Hormone levels are measured during gender-affirming treatment to ensure endogenous sex steroids are lowered and administered sex steroids are maintained at levels appropriate for the treatment goals of transgender people according to the Tanner stage. | For masculinising treatment, total testosterone levels are maintained at the lower male reference range, and for feminising treatment, estradiol is aimed to be within the female reference range. |
| Reference | [ ] | [ ] | [ , ] |
| Clinical Chemistry Tests | Other Tests | |
|---|---|---|
| LH, FSH, E2/T, 25(OH)D | Anthropometry: height, weight, blood pressure, Tanner stages | |
| Suggested Interval | 6–12 months | 3–6 months |
| Bone density using DXA | ||
| Suggested Interval | 1–2 years | |
| Reference | [ ] |
| Laboratory Tests | Other Tests | |
|---|---|---|
| Transgender AFAB people | T | Monitor for virilization |
| Suggested Interval | 3 monthly until levels within adult range | Every 3 months the first year and then one or two times per year |
| Haematocrit or haemoglobin | Screening for osteoporosis, cervical screening (if cervical tissue present), breast cancer screening as recommended | |
| Suggested Interval | 3 monthly for first year then one/two times per year | |
| Lipids at regular intervals | ||
| Transgender AFAM people | Serum T and estradiol | Feminisation |
| Suggested Interval | Every 3 months | Every 3 months the first year and then one or two times per year |
| If treated with spironolactone, electrolytes | Routine cancer screening and bone density | |
| Every 3 months the first year and then annually | ||
| Reference | [ ] |
| The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
Share and Cite
Ramasamy, I. Gender Reassignment and the Role of the Laboratory in Monitoring Gender-Affirming Hormone Therapy. J. Clin. Med. 2024 , 13 , 5134. https://doi.org/10.3390/jcm13175134
Ramasamy I. Gender Reassignment and the Role of the Laboratory in Monitoring Gender-Affirming Hormone Therapy. Journal of Clinical Medicine . 2024; 13(17):5134. https://doi.org/10.3390/jcm13175134
Ramasamy, Indra. 2024. "Gender Reassignment and the Role of the Laboratory in Monitoring Gender-Affirming Hormone Therapy" Journal of Clinical Medicine 13, no. 17: 5134. https://doi.org/10.3390/jcm13175134
Article Metrics
Article access statistics, further information, mdpi initiatives, follow mdpi.

Subscribe to receive issue release notifications and newsletters from MDPI journals

IMAGES
VIDEO
COMMENTS
At 8 months of age, Reimer became the unwitting subject of "sex reassignment," a treatment method embraced by his parents after his penis was all but obliterated during a botched circumcision.
The breakthrough paper laid the foundation against performing sex reassignment surgery on intersex infants, which was once considered a "fix" for their gender non-conforming biology.
Finally, on 14 March 1980, Reimer's parents told him the truth about his sex reassignment, [ 29] following advice from Reimer's endocrinologist and psychiatrist. At the age of 14, having been informed of his past by his father, Reimer decided to assume a male gender identity, calling himself David.
The John Money Experiment involved David Reimer, a twin boy raised as a girl following a botched circumcision. Money asserted gender was primarily learned, not innate. However, David struggled with his female identity and transitioned back to male in adolescence. The case challenged Money's theory, highlighting the influence of biological sex on gender identity.
In the mid-1960s, psychologist John Money encouraged the gender reassignment of David Reimer, who was born a biological male but suffered irreparable damage to his penis as an infant.
"Gender normalizing" operations have been performed on intersex babies since at least the 1950s. Now, parents are questioning whether the surgery is necessary.
During the past 50 years, the medical paradigm in the US has held that appropriate adjustment to the gender assigned at birth would be dependent upon the external genitalia appearing entirely ...
Nikki, born a biological boy named Niko, began at the age of 10 the complicated transition to becoming girl. Gillian Laub's video captures how through the loving support of family and friends, two ...
The individual, however, was later found to reject this sex of rearing, switched at puberty to living as a male, and has successfully lived as such from that time to the present. The standard in instances of extensive penile damage to infants is to recommend rearing the male as a female. Subsequent cases should, however, be managed in light of ...
In an age of increasing gender fluidity, it is surprising that so many find it difficult to accept the gender of their birth and take the drastic step of changing it through surgery. What are ...
In the Operating Room During Gender Reassignment Surgery. Behind the scenes with identical twin Emmie Smith during her medical transition. Before August 30, 2016, getting stitches at age seven was ...
Also called gender reassignment surgery, the goal of this procedure is to create the outward physical appearance of the gender with which the person identifies. "Top surgery" refers to surgery above the waist, while "bottom surgery" refers to surgery below the waist. Transgender surgery is major surgery and generally not considered ...
Sex is generally conceived of as encompassing the biological differences between males and females, based on genetics and sex hormones, whereas gender includes "the social, psychological ...
Gender-affirming surgery is a surgical procedure, or series of procedures, that alters a person's physical appearance and sexual characteristics to resemble those associated with their identified gender. The phrase is most often associated with transgender health care and intersex medical interventions, although many such treatments are also ...
Sex assignment. Sex assignment (also known as gender assignment[ 1][ 2]) is the discernment of an infant's sex, typically made at birth based on an examination of the baby's external genitalia by a healthcare provider such as a midwife, nurse, or physician. [ 3] In the vast majority of cases (99.95%), sex is assigned unambiguously at birth.
Thousands of children in the United States now openly identify as a gender different from the one they were assigned at birth, their numbers surging amid growing recognition of transgender ...
Gender dysphoria—a condition in which an individual has a severe discontent with the gender they were born with—can be treated with gender reassignment surgery. In this article, Selvaggi and ...
Sex is a label — male or female — that you're assigned by a doctor at birth based on the genitals you're born with and the chromosomes you have. It goes on your birth certificate. Gender is much more complex: It's a social and legal status, and set of expectations from society, about behaviors, characteristics, and thoughts.
Gender Confirmation (GCS), formerly known as sex reassignment surgery, can be very complex. Find out more about these procedures.
Gender assignment at birth in cases of ambiguous genitalia (AG) has long been based on anatomical appearance, adequacy of the phallus and/or response to testosterone.
Assigned sex is a biological label - male or female - you're born with. Gender describes your identity through behaviors and societal expectations of masculinity and femininity. Many people in the LGTBQ+ community delay care because of fear of judgement. While both terms are related, sex and gender have different meanings—and some gender ...
Feminizing surgery, also called gender-affirming surgery or gender-confirmation surgery, involves procedures that help better align the body with a person's gender identity. Feminizing surgery includes several options, such as top surgery to increase the size of the breasts. That procedure also is called breast augmentation.
Transgender people experience distress due to gender incongruence (i.e., a discrepancy between their gender identity and sex assigned at birth). Gender-affirming hormone treatment (GAHT) is a part of gender reassignment treatment. The therapeutic goals of the treatment are to develop the physical characteristics of the affirmed gender as far as possible. Guidelines have been developed for GAHT ...